Evaluation of Cerebral Blood Flow in Dementia with Lewy Bodies by 99mTECD SPECT Imaging
Received: 17-May-2018 / Accepted Date: 26-May-2018 / Published Date: 02-Jun-2018 DOI: 10.4172/2161-0460.1000440
Abstract
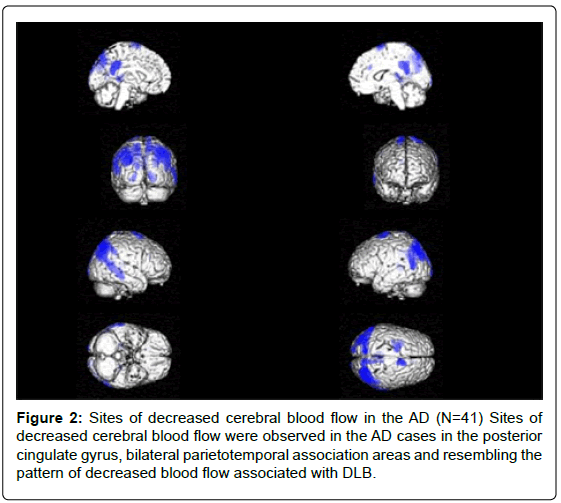
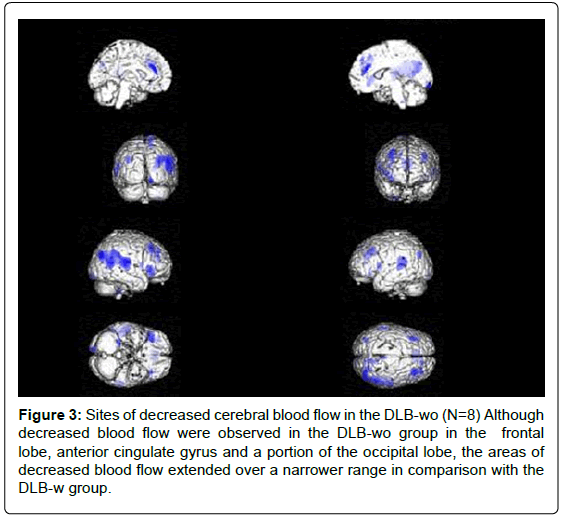
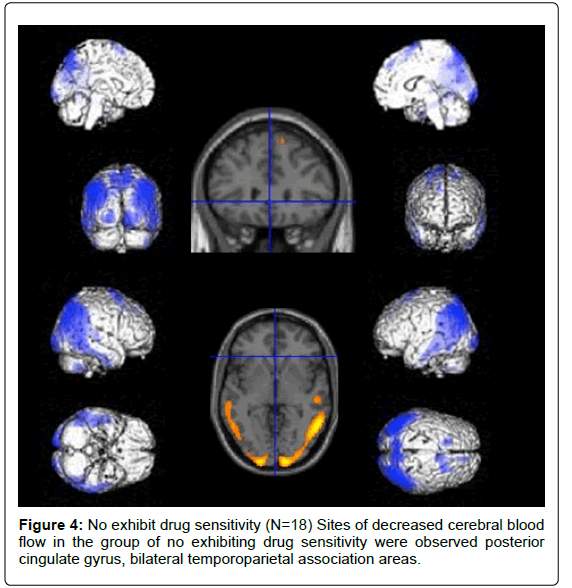
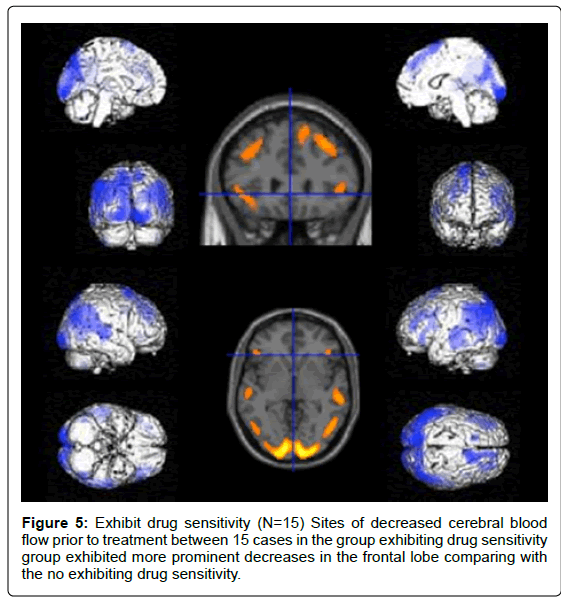
To clarify differences between dementia with Lewy Bodies (DLB) and Alzheimer’s disease (AD) in the actual clinical setting, we studied sites of decreased cerebral blood flow (CBF) in cases of DLB and AD by 99mT-ECD-SPECT imaging using statistical parametric mapping (SPM8). In addition, the drug sensitivity was analyzed by SPM8. Twentyfive cases were classified as DLB with AD (DLB-w) and 8 cases were DLB without AD (DLB-wo). Sites of decreased CBF in the DLB-w group were observed in the posterior cingulate gyrus, bilateral parietotemporal association areas and the occipital lobe, and these sites resembled the pattern of decreased CBF associated with AD. Among the DLBwo cases, decreased CBF was observed in frontal lobe, anterior cingulate gyrus and occipital lobe. In a comparison of sites of decreased CBF prior to treatment between 15 cases in the group exhibiting drug sensitivity and 18 cases in the group not exhibiting drug sensitivity, the drug sensitivity group exhibited more prominent decreases in CBF in the frontal lobe. In summary, 78% of DLB cases were determined to be complicated with DAT based on SPECT imaging, and the pattern of decreased CBF in these cases resembled that of DAT.
Keywords: Dementia with lewy bodies; Statistical parametric mapping; Sites of decreased cerebral blood; Alzheimer disease; DLB in autopsy cases in japan; Drug sensitivity
Introduction
Although dementia with Lewy bodies (DLB) and Alzheimer’s disease (AD) are different diseases, they frequently present pathologies resulting from complication by both diseases. As a result of a detailed investigation of 37 autopsied cases of DLB in Japan conducted by Kosaka, et al. 75.7% were complicated with some form of AD pathology. These cases were referred to as the common type. On the other hand, 24.3% of the cases consisted of pure DLB not presenting with Alzheimer lesions, and these cases were referred to as the pure type. Since the pathogenesis might be overlapped between DLB and AD, differential diagnosis of these two entities is often quite difficult and confusing.
In this study, we examined the degree to which cases clinically diagnosed with DLB were complicated with AD pathology using the Easy Z-score Imaging System (eZIS) [1-4]. The latter is a SPECT image statistical analysis technique for cerebral blood flow developed by Matsuda, et al. eZIS depicts changes in cerebral blood flow on the brain surface after converting SPECT images of the cerebral blood flow of individuals to that of a standard brain using SPM2 based on Z-score mapping. This image analysis technique is performed using a procedure similar to that of three-dimensional stereotactic projection (3D-SSP) [5,6] developed by Minoshima, et al., and is currently widely popular in Japan. Moreover, since eZIS makes it possible to set a specific region of decreased blood flow (specific VOI) in the early stages of AD, and assign numerical values to the severity and extent of the decrease in blood flow in that region as well as the ratio between the specific extent of decreased blood flow and the extent of decreased blood flow throughout the brain, comparison of these parameters makes it possible to acquire an objective picture of the relationship with the severity of AD and the degree of progression of the disease.
The purpose of this study is to examine SPECT images of DLB by using the three parameters of eZIS to categorize cases that exceeded one or more AD reference values as being complicated with AD pathology (DLB-w) and cases in which all parameters were equal to or less than the reference values as not being complicated with AD pathology (DLB-wo) for the purpose of conducting a comparative study of differences between the two based on sites of decreased cerebral blood flow.
Subjects and Methods
Subjects
The subjects consisted of 33 cases of DLB diagnosed using revised criteria for the clinical and pathologic diagnosis of DLB that were outpatients at the Department of Geriatric Medicine of the Tokyo Medical University Hachioji Medical Center (19 men, 14 women, average age: 81.7 years).
Methods
Comparison of decreased cerebral blood flow during initial examination: SPECT examinations using 99mTc-ECD were performed, and those cases exhibiting values for severity, extent and ratio that exceeded reference values based on easy Z-score Imaging System (eZIS)- specific volume of interest analysis (SVA) established by Matsuda, et al., were categorized as DLB with AD (DLB-w), while those cases exhibiting values that were equal to or less than those reference values were categorized as DLB without AD (DLB-wo), followed by conducting a comparative study of sites of decreased cerebral blood flow prior to treatment using SPM8.
Relationship between presence of drug sensitivity and cerebral blood flow: Thirty cases of DLB that underwent treatment consisting primarily of donepezil hydrochloride (Aricept) were categorized into a group that exhibited some degree of drug sensitivity consisting of 12 cases and a group that did not exhibit drug sensitivity consisting of 18 cases, and those sites of decreased cerebral blood flow prior to treatment were compared for each group using SPM8.
Ethical Considerations
Informed written consent was received from all patients and their families for blood collection, psychological testing, and SPECT imaging.
Results
There were 25 cases (75.8%) which were categorized as DLB-w (14 men, 11 women, average age: 80.1 years) while 8 cases (24.2%) categorized as DLB-wo (5 men, 3 women, average age: 83.3 years). These percentages closely resembled the percentages of common DLB (28 cases: 75.5%) and pure DLB (9 cases: 24.3%) based on the DLB classifications of 37 autopsy cases by Kosaka (Tables 1 and 2).
| DLB-w | DLB-wo | Total | |
|---|---|---|---|
| No of cases | 25(75.8%) | 8(24.2%) | 33 |
| Gender ratio | Male:14; Female:11 | Male:5; Female:3 | Male:19; Female:14 |
| average age | 80.1 y.o | 83.3 y.o | 81.7 y.o |
| Drug sensitivity | Yes: 14 (56.0%) | Yes: 1 (12.6%) | Yes: 15 (45.5%) |
| No: 11 (44.0%) | No: 7 (87.4%) | No: 18 (54.4%) |
Table 1: Classification of DLB cases in this study. There were 25 cases (75.8%) categorized as DLB-w (14 men, 11 women, average age: 80.1 years) and 8 cases (24.2%) categorized as DLB-wo (5 men, 3 women, average age: 83.3 years) 14 of 25 cases (56%) exhibited drug sensitivity in the DLB-w group, while 1 of 8 cases (12.6%) exhibited drug sensitivity in the DLB-wo group, with the DLB-w group tending to have a large number of cases exhibiting drug sensitivity.
| Common type (28 cases 75.7%) Ave.age 69.2 y.o. | Presenting with some degree of Alzheimer lesions |
| Pure type (9 cases 24.3%) Ave.age 38.9 y.o. | No or few presenting with Alzheimer lesions |
Table 2: DLB classification of 37 autopsy in JAPAN by Kosaka. The percentages of common DLB (28 cases: 75.5%) and pure DLB (9 cases: 24.3%) based on the DLB classifications of 37 autopsy cases by Kosaka.
In the DLB-w group, 14 of 25 cases (56%) exhibited drug sensitivity, while 1 of 8 cases (12.6%) exhibited drug sensitivity in the DLB-wo group. The DLB-w group showed a higher drug sensitivity.
Sites of decreased cerebral blood flow were observed in the DLB-w group in the posterior cingulate gyrus, bilateral temporoparietal association areas and over a wide range of the occipital lobe, resembling the pattern of decreased blood flow associated with AD (Figures 1 and 2). Although decreased blood flow was observed in the DLB-wo group in the frontal lobe, anterior cingulate gyrus and a portion of the occipital lobe, the areas of decreased blood flow extended over a narrower range in comparison with the DLB-w group (Figure 3).
Figure 1: Sites of decreased cerebral blood flow in the DLB-w (N=25) Sites of decreased cerebral blood flow were observed in the DLB-w group in the posterior cingulate gyrus, bilateral temporoparietal association areas and over a wide range of the occipital lobe, resembling the pattern of decreased blood flow associated with AD.
Figure 3: Sites of decreased cerebral blood flow in the DLB-wo (N=8) Although decreased blood flow were observed in the DLB-wo group in the frontal lobe, anterior cingulate gyrus and a portion of the occipital lobe, the areas of decreased blood flow extended over a narrower range in comparison with the DLB-w group.
In a comparison of sites of decreased cerebral blood flow prior to treatment between 15 cases in the group exhibiting drug sensitivity and 18 cases in the group not exhibiting drug sensitivity, the drug sensitivity group exhibited more prominent decreases in blood flow in the frontal lobe (Figures 4 and 5).
Discussion
According to the classification of 37 autopsy cases of dementia with Lewy bodies (DLB) made by Kosaka, 28 cases (75.7%) were categorized as “common DLB”, presenting with some degree of Alzheimer lesions, while 9 cases (24.3%) were categorized as “pure DLB”, not presenting with Alzheimer`s disease (AD) lesions, and the common form was reported to be observed much more frequently than the pure form. In this study, there were 25 cases complicated with AD (75.8%) and 8 cases not complicated with AD (24.2%). These percentages closely resembled those of the 37 autopsied cases determined by Kosaka. This suggests that the presence or absence of AD pathology can be inferred using SPECT images.
In the comparison of sites of decreased cerebral blood flow as determined using SPM8, those sites of decreased cerebral blood flow among DLB-w cases were observed in the posterior cingulate gyrus, bilateral parietal-lateral association areas and over a wide range of the occipital lobe, and in contrast to these sites resembling the pattern of decreased blood flow observed in DAT, among the DLB-wo cases, although decreases were observed in the frontal lobe, anterior cingulate cortex and a portion of the occipital lobe, regions of decreased blood flow were less extensive in comparison with DLB-w.
Although one of the characteristics symptoms of DLB is drug hypersensitivity, the cause of this is not fully understood [7]. In a randomized placebo-controlled trial of donepezil for dementia with Lewy bodies conducted in Japan, the incidences of adverse events in a placebo dose group, donepezil 3 mg dose group, donepezil 5 mg dose group and donepezil 10 mg dose group were 70.6%, 68.6%, 81.8% and 86.5%, respectively, and although gastrointestinal symptoms such as diarrhea, nausea and loss of appetite were reported, there were no differences observed between the three donepezil dose groups [8]. In other words, although drug hypersensitivity is widely reported to be associated with DLB, drug hypersensitivity with respect to donepezil was similar to that of the placebo and there were no well-defined differences observed.
However, according to the results of our study, drug hypersensitivity appeared in 15 of 33 cases (45.5%), appearing in 14 of 25 cases in the DLB-w group (56%) but only in 1 of 8 cases (12.6%) in the DLB-wo group, thereby demonstrating a more prominent trend in the DLB-w group. Moreover, in a comparison of sites of decreased blood flow prior to treatment between 15 cases that demonstrated drug hypersensitivity and 18 cases that did not demonstrate drug hypersensitivity, decreased blood flow was strongly indicated in the frontal lobe in the group that demonstrated drug hypersensitivity. This indicates that complaints of drug hypersensitivity may frequently be associated with feeling-related factors such as “feeling poorly” or “feeling bad”, and that the frontal lobe may be related to control of how a patient feels and his or her emotions. Although DLB is known to frequently be complicated with symptoms of depression [9], when considering that decreased blood flow in the frontal lobe was conspicuous among members of the group that demonstrated drug hypersensitivity, the possibility that drug hypersensitivity appears in the form of a neurological manifestation such as depression cannot be ruled out. There are many aspects of DLB that are not yet understood both in terms of the clinical picture and pathology. It is expected that further research will be conducted through the accumulation of a greater number of cases in the future.
References
- Kosaka K (1990) Diffuse lewy body disease in japan. J Neurol 237: 197-204.
- Matsuda H, Mizumura S, Nagao T (2007) Automated discrimination between very early Alzheimer disease and controls using an easy Z-score imaging system for multicenter brain perfusion single-photon emission tomography. AJNR Am Neuroradiol 28: 731-736.
- Waragai M, Mizumura S, Yamada T, Matsuda H (2008) Differentiation of early-stage Alzheimer's disease from other types of dementia using brain perfusion single photon emission computed tomography with easy Z-score imaging system analysis. Dement Geriatr Cogn Disord. 26: 547-555.
- Matsuda H (2007) [Neurological diseases and SPECT--analysis using easy Z-score imaging system (eZIS)]. Brain Nerve 59: 487-493.
- Minoshima S, Frey KA, Koeppe RA, Foster NL, Kuhl DE (1995) A diagnostic approach in Alzheimer's disease using three-dimensional stereotactic surface projections of fluorine-18-FDG PET. J Nucl Med 36: 1238-1248.
- Minoshima S, Koeppe RA, Frey KA, Kuhl DE (1994) Anatomic standardization: Linear scaling and nonlinear warping of functional brain images. J Nucl Med 35: 1528-1537.
- Campbell S, Stephens S, Ballard C (2001) Dementia with lewy bodies: Clinical features and treatment. Drugs Aging 18: 397-407.
- Mori E, Ikeda M, Kosaka K, Donepezil-DLB Study Investigators (2012) Donepezil for dementia with lewy bodies: A randomized, placebo-controlled trial. Ann Neurol 72: 41-52.
- McKeith IG, Dickson DW, Lowe J, Emre M, O'Brien JT, et al. (2005) Diagnosis and management of dementia with lewy bodies: Third report of the DLB Consortium. Neurology 65: 1863-1872.
Citation: Kanaya K, Abe S, Hanyu H (2018) Evaluation of Cerebral Blood Flow in Dementia with Lewy Bodies by 99mT-ECD SPECT Imaging. J Alzheimers Dis Parkinsonism 8: 440 DOI: 10.4172/2161-0460.1000440
Copyright: © 2018 Kanaya K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5666
- [From(publication date): 0-2018 - Oct 18, 2025]
- Breakdown by view type
- HTML page views: 4735
- PDF downloads: 931