Factors Associated with Induced Preterm Birth and Its Immediate Outcome in Addis Ababa Public Hospitals, Ethiopia
Received: 25-Sep-2018 / Accepted Date: 23-Oct-2018 / Published Date: 31-Oct-2018 DOI: 10.4172/2572-4983.1000170
Abstract
Objective: It was to assess factors associated with induced preterm birth and its immediate outcome from 2011 to 2015 in Addis Ababa public hospitals.
Methods: The hospitals were selected by simple random sampling. Following this, the neonatal medical records were selected by systematic sampling from admission neonatal intensive care unit’s log book. Data were collected using structured questionnaire. Finally data were entered to EPIDATA3.1 and transported to SPSS 22 for analysis. Analysis was undertaken using bivariate and multivariate logistic regression.
Result: Majority (66.1%) of preterm births were spontaneous and 33.9% were induced preterm births. From those admitted preterm births to Neonatal intensive care unit, 45.3% were died and 54.7% discharged alive. Maternal Human immune deficiency virus (HIV) infection [p=0.003, AOR=6.446, 95%CI: (3.085, 26.279)] was one of the factors associated with both the induced preterm birth and immediate death outcome of preterm birth.
Conclusion: Maternal HIV infection and hypertension during pregnancy were associated with the induced preterm birth; and maternal HIV infection, premature rupture of membrane, low Appearance, pulse, grimace, activity and respiration (APGAR) score and respiratory distress were associated with immediate death outcome of preterm birth.
Keywords: Preterm; Induced; Immediate death outcome
Introduction
WHO defined Preterm birth as a delivery that occurs before 37 completed weeks of gestation. It is classified as extremely preterm (<28 weeks), very preterm (28 to <32 weeks), and moderate to late preterm (32 to <37 weeks). On similar basis, preterm birth can be categorized by birth weight. Neonates less than 2500 g are classified as low birth weight (LBW), <1500 g, as very low birth weight (VLBW) and <1000 gas extremely low birth weight (ELBW) preterm. Preterm birth can also be spontaneous or provider initiated (induced). Spontaneous preterm birth is commencement of labor with intact or pre labor rapture of membrane and birth before 37 weeks of gestation. Providerinitiated (induced) preterm birth results from intervention such as induction of labor or caesarian section taken for maternal or fetal condition. Spontaneous and induced (provider initiated) preterm births account for 65-70% and 30-35% of all preterm births respectively [1].
Preterm birth is the leading cause of infant morbidity and mortality throughout the world. It has significant consequences on health, social, psychology and economy. Global rate of preterm birth is increasing from which 5% to 7% is in developed countries and significantly higher in least developed countries. From total 135 million live births in the world, 14.9 million (11.1%) babies were born preterm in 2010. Greater than 60% of preterm births occurred in Sub-Saharan Africa and south Asia 12.8% (9.1 million) [2].
As gestational age decrease mortality rate increases, and being born both preterm and small for gestational age are at even high risk. In many low income countries, only 30% of those born at 28 to 32 weeks survive while almost all preterm births <28 weeks die within the first few days of life. In all settings, majority of deaths stand for very or extremely preterm births, especially where simple care is lacking in low income countries. Although their absolute numbers are lower, preterm-SGA infants carry a higher risk of mortality in the newborn and infant period than term-SGA infants. Estimate of 86% of extremely preterm live birth babies died in the early neonatal period compared to 50.5% of very preterm babies [3-6].
The highest rate (23%) of preterm birth in Southeast Nigeria was evidenced during 2012 and the increment from 9.8% to 17.1% was realized from 2009 to 2013. In this region, majority (57%) of preterm births were spontaneous and the rest (43%) were induced (providerinitiated) preterm births. 2011 EDHS reported 37/1000 live births Neonatal Mortality Rate (NMR) which was almost similar with 2005 EDHS report of 39/1000 live births. Commonly stated causes of neonatal death were prematurity (37%), infection (28%), and asphyxia (24%) [4,7,8]. In Northwest Ethiopia, Gondar University hospital about 14.3% was found to be preterm birth and 31.4% rate of preterm delivery in mothers having pregnancy related hypertension was recorded in Mettu Karl hospital, Southwestern Ethiopia [9-11].
In later life, being born preterm predisposes infants to bad health outcomes like chronic diseases which can end with death. Thus, the issue of addressing preterm birth is crucial for accelerating progress towards Universal Sustainable Development Goal 4. Specially, infants born before 32 weeks of gestation are at particularly high risk of adverse outcomes [5,12-17].
Little is known about risk factors and immediate outcome of induced preterm in Ethiopia. Therefore, this study serves as base line information about factors associated with induced preterm birth and it’s immediate out come in the context of this country. Beside, this supports for the readiness of health facilities so as to make appropriate diagnosis and evaluation of the causes of preterm births and their deaths.
The aim of this study was to assess factors associated with induced preterm birth and its immediate outcome that intended to contribute improvement and necessary adjustments to neonatal care.
Materials and Methods
The design applied to this study was institutional based cross sectional study. Six Addis Ababa public hospitals had neonatal intensive care unit. From these, simple random sampling was the sampling method to select the three hospitals. Proportional allocation of the sample to the selected hospitals was undertaken on the basis of their number of preterm admissions. Medical records of the preterm neonates were sought from registry log book of the neonatal intensive care unit and study unit selection was handled by systematic sampling. Data collection was accomplished by using structured, pretested questionnaire which was adopted and modified from different related studies [2,3,11,18-21].
EpiData3.1 was used for data entry and later exported to SPSS version 22 where data cleaning, recoding and analysis were performed. Bivariate and multivariate logistic regression analyses were done to assess associations between variables. The cut point of P-value <0.05 was used to indicate statistical significance of the variables.
Official letter from Addis Ababa University, school of Allied health sciences department of nursing and midwifery was written to Black lion specialized hospital and Addis Ababa regional health office for permission of both Gandhi and Zewditu memorial hospitals. Then, the city health Bearue processed the permission of the two hospitals. Following this, permission from the medical director, neonatology and pediatric department of the three hospitals were processed, and medical record office of the respective hospital was contacted accordingly. Finally, respectful care for the patient’s medical record with maintaining of confidentiality was involved to the end of data collection.
Results
The age of the mother ranges 14 to 43 years with mean age of 26.09 (±4.772908 SD). Majority (51.7%) of them were above the mean age (>26). Around fifty one percent and 52.9% (203) were primigravida and primipara respectively. Abortion stands first (34.8%) and neonatal death was the rare (3.9%) outcome of the immediate previous pregnancy (Table 1). From multi-para mothers, 24.3% (44), 29.8% (54), 35.9% (65), 9.4% (17) and 0.6% (1) have given birth before 12 months, 18 months, 24 months, 36 months and further than 36 months respectively.
| Out come | Frequency | Percent |
|---|---|---|
| Preterm birth | 45 | 24.9 |
| Still birth | 19 | 10.5 |
| Neonatal death | 7 | 3.9 |
| Abortion | 63 | 34.8 |
| Normal | 47 | 26.0 |
| Total | 181 | 100.0 |
Table 1: Outcome of immediate previous pregnancy of preterm baby’s mothers, Addis Ababa, Ethiopia, April 2016.
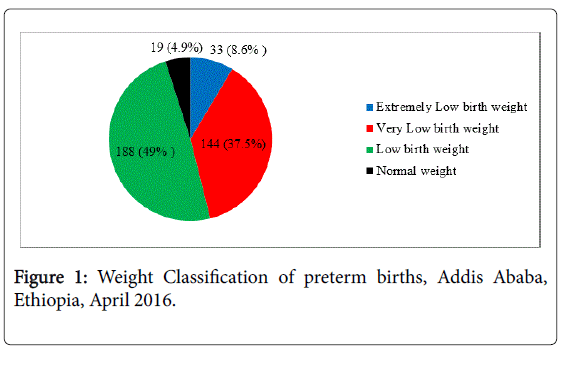
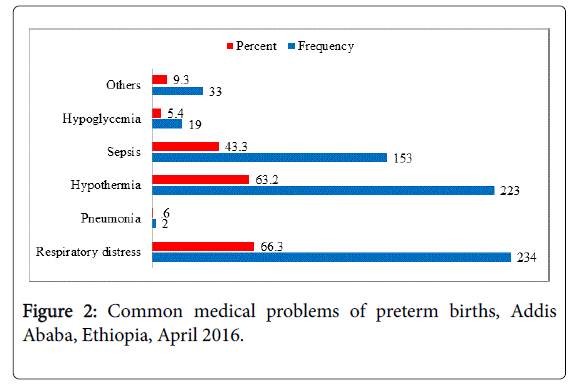
The mean gestational age was 32.45 weeks (±2.903 SD). Majority of the preterm births were under moderate to late preterm. The mean of first minute APGAR was 5.64 (+1.592) and majority (68%) had had low APGAR score. Averagely, they were 41.77 cm long with standard deviation of 5.137. The mean weight was 1669.4 g (±508.688 SD) while 700 g was the minimum weight and the maximum to be 4000 g (Figure 1). Three hundred fifty three (91.9%) of the neonates were diagnosed at least to have one medical problem and the left 8.1% (31) had no medical problems on admission. Of these; 66.3% (234) had respiratory distress and 0.6% (2) had Pneumonia (Figure 2).
Factors associated with induced preterm birth
In bivariate analysis, maternal age, maternal HIV infection, diagnosis of medical disorder during pregnancy, hypertension during pregnancy, premature rupture of membrane had significant association with induced preterm birth. However, variables like parity, gravidity, multiple pregnancies, outcome of immediate previous pregnancy, time and mode of previous delivery had not shown significant association with induced preterm birth in this study.
From those variables shown significant statistical association in bivariate analysis, only maternal HIV infection and hypertension during pregnancy remained significant in multivariate analysis (Table 2). Accordingly, mothers who had hypertension during pregnancy 5 times more likely gave induced preterm birth than those who had no hypertension during pregnancy (p=0.001, AOR=5.082, 95%CI: 1.913, 13.498). On the contrary, mothers with HIV infection had less odds of giving induced preterm birth than their counter part (p=0.035, AOR=0.28, 95%CI: 0.090, 0.916).
| Characteristics | Indicated preterm | S.E. | P-value | AOR (95% C.I) | ||
|---|---|---|---|---|---|---|
| Yes: # (%) | No: # (%) | |||||
| Age of mother | ||||||
| <25 | 52 (27.8) | 135 (72.2) | 0.406 | 0.247 | 1.600 (0.723, 3.543) | |
| >26* | 78 (39.6) | 119 (60.4) | - | - | 1 | |
| Gravidity | ||||||
| <1 | 60 (30.8) | 135 (69.2) | 1.561 | 0.691 | 1.859 (0.087, 39.624) | |
| >2* | 70 (37.0) | 119 (63.0) | - | - | 1 | |
| Parity | ||||||
| <1 | 62 (30.5) | 141 (69.5) | 1.542 | 0.927 | 0.868 (0.042, 17.822) | |
| >2* | 68 (37.6) | 113 (62.4) | - | - | 1 | |
| Multiple pregnancy | ||||||
| Yes | 29 (39.7) | 44 (60.3) | 0.535 | 0.808 | 0.878 (0.307, 2.508) | |
| No* | 101 (32.5) | 210 (67.5) | - | - | 1 | |
| Maternal HIV infection | ||||||
| Yes | 6 (25.0) | 18 (75.0) | 0.592 | 0.035* | 0.287 (0.090, 0.916) | |
| No* | 74 (56.1) | 58 (43.9) | - | - | 1 | |
| Hypertension during pregnancy | ||||||
| Yes | 53 (80.3) | 13 (19.7) | 0.498 | 0.001* | 5.082 (1.913, 13.498) | |
| No* | 27 (30.0) | 63 (70.0) | - | - | 1 | |
| PROM | ||||||
| Yes | 24 (51.1) | 23 (48.9) | 0.527 | 0.054 | 0.362 (0.129, 1.017) | |
| No* | 57 (52.3) | 52 (47.7) | - | - | 1 | |
*Significant in multivariate analysis
Table 2: Multivariate Analysis of factors associated with induced Preterm birth, Addis Ababa, Ethiopia, April 2016.
Factors associated with immediate outcome of preterm birth
In bivariate analysis, factors like maternal age, gravidity, parity, multiple pregnancy, birth intervals, diabetes and hypertension during pregnancy had no significant association while some variables shown significant association with immediate death outcome of the preterm birth. For instance preterm neonate of HIV mother more likely died before discharge than that of HIV negative mothers (P=0.004, OR=4.200, 95%CI: 1.566, 11.265). Likewise, those preterm neonates who were born to mothers who experienced premature rupture of membrane had about 4 times more probability of death (p=0.000, OR=4.066, 95%CI: 1.947, 8.493) than those who born to mothers who did not develop rupture of membrane.
Compared to moderate to late preterm birth, extremely preterm (P=0.024, OR=2.091, 95%CI: 1.104, 3.958) and very preterm (P=0.000, OR=2.723, 95%CI: 1.726, 4.296) more likely died before discharge. Extremely low birth weight (P=0.002, OR=7.467, 95%CI: 2.083, 26.762) and very low birth weight preterm (P=0.042, OR=3.043, 95%CI: 1.042, 8.892) more likely died before discharge in comparison to preterm babies with normal weight, but low birth weight had no significant association with death. Preterm with low APGAR score (P=0.000, OR=5.215, 95%CI: 3.154, 8.623) died 5 folds greater than those with normal APGAR score before discharge. In relative to induced preterm birth, spontaneous preterm (P=0.005, OR=0.541, 95%CI: 0.353, 0.829) had less chance of death before discharge. Preterm baby who had sepsis more likely died before discharge unlike who had no sepsis (P=0.000, OR=3.07, 95%CI: 1.988, 4.770). Diagnosis of respiratory distress had also shown significant association (P=0.000, OR=4.081, 95%CI: 2.512, 6.629) that those diagnosed with respiratory distress had 4.081 times greater odds of death than preterm births who had no respiratory distress. However, hypothermia and pneumonia didn’t show any significant association in bivariate analysis. Also weight category (being SGA, AGA, and LGA) had no significant association with immediate death outcome of the preterm neonate.
Only Maternal HIV infection, premature rupture of membrane (PROM), low APGAR score and respiratory distress remained significantly associated in multivariate analysis. Thus, preterm babies born to HIV positive mother more likely (p=0.003, AOR=6.446, 95%CI: 3.085, 26.279) died before discharge than those who born to HIV negative mother. Also preterm died before discharge had greater odds (P=0.00, AOR=8.365, 95%CI: 6.897, 23.242) of being born after premature rupture of membrane that is 8.365 times greater odds of those who born before their mothers experienced rupture of membrane. Likewise those preterm births with low APGAR score 4 times more likely died before discharge than those with normal APGAR score (P=0.0444, AOR=4.342, 95%CI:1.040, 18.135). Similarly, preterm birth with respiratory distress also died almost 5 times more likely than those who hadn’t the problem (P=0.044, AOR=4.956, 95%CI: 1.041, 23.585) (Table 3).
| Characteristics | Death before discharge | S.E. | P-value | AOR (95% C.I) | ||
|---|---|---|---|---|---|---|
| Yes: # (%) | No: # (%) | |||||
| Maternal HIV infection | ||||||
| Yes | 18 (75.0) | 6 (25.0) | 1.133 | 0.003** | 6.446 (3.085,26.279) | |
| No* | 55 (41.7) | 77 (58.3) | - | - | 1 | |
| Hypertension during pregnancy | ||||||
| Yes | 35 (53.0) | 31 (47.0) | 0.870 | 0.546 | 1.691 (0.307, 9.304) | |
| No* | 38 (42.2) | 52 (57.8) | - | - | 1 | |
| PROM | ||||||
| Yes | 33 (70.2) | 14 (29.8) | 0.901 | 0.000** | 8.365 (6.897, 23.242) | |
| No* | 40 (36.7) | 69 (63.3) | - | - | 1 | |
| Spontaneous Preterm birth | ||||||
| Yes | 102 (40.2) | 152 (59.8) | 0.820 | 0.073 | 0.230 (0.046,1.149) | |
| No* | 72 (55.4) | 58 (44.6) | - | - | 1 | |
| GA based classification | ||||||
| Extremely preterm | 25 (53.2) | 22 (46.8) | 0.924 | 0.208 | 3.198 (0.523, 19.545 | |
| Very preterm | 74 (59.7) | 50 (40.3) | 0.753 | 0.473 | 1.717 (0.392, 7.511) | |
| Moderate to late preterm* | 75 (35.2) | 138 (64.8) | - | - | 1 | |
| Weight based classification | ||||||
| ELBW | 24 (72.7) | 9 (27.3) | 5584.45 | 0.997 | 1.480 (0.000, …) | |
| VLBW | 75 (52.1) | 69 (47.9) | 5584.45 | 0.997 | 4.203 (.000…) | |
| Normal weight* | 5 (26.3) | 14 (73.7) | - | - | 1 | |
| APGAR score | ||||||
| Low APGAR score | 149 (57.1) | 112 (42.9) | 0.729 | 0.044** | 4.342 (1.040, 18.135) | |
| Normal APGAR score* | 25 (20.3) | 98 (79.7) | - | - | 1 | |
| Hypothermia | ||||||
| Yes | 114 (51.1) | 109 (48.9) | 0.603 | 0.965 | 1.027 (0.315,3.351) | |
| No* | 109 (48.9) | 75 (57.7) | - | - | 1 | |
| Respiratory distress | ||||||
| Yes | 138 (59.0) | 96 (41.0) | 0.796 | 0.044** | 4.956 (1.041,23.585) | |
| No* | 31 (26.1) | 88 (73.9) | - | - | 1 | |
| Sepsis | ||||||
| Yes | 97 (63.4) | 56 (36.6) | 5584.45 | 0.997 | 47.625 (0.000, …) | |
| No* | 72 (36.0) | 128 (64.0) | - | - | 1 | |
**Significant in multivariate analysis
Table 3: Multivariate Analysis of factors associated with immediate death outcome of Preterm birth, Addis Ababa, Ethiopia, April 2016.
Discussion
Average gestational age of the preterm in this study (32.45 weeks) is almost similar with the recorded mean age of preterm in Gondar university hospital, but higher than that of gestational age in preterm birth in Vali-e ASR hospital of Tehran Iran [21,22]. Methodological and socio-economic difference might play a role for this variation. Proportion of preterm-AGA (70.3) was greater than the proportion of preterm-SGA. This is similar with that of finding in East Africa [11]. In line with evidence from study of Southeast Nigeria, few preterm had normal birth weight [3]. Mothers with HIV infection had less odds of giving induced preterm birth than their counter group even though it increased risk of giving preterm birth in Tanzania [23]. As it was evidenced in different studies [23-25] for preterm, hypertension was significantly associated with preterm birth and highly increased risk of induced preterm birth.
This study also found out factors associated with immediate death outcome of preterm birth. From maternal factors, those born to HIV positive mothers had greater risk of death before discharge both in bivariate and multi-variate analysis. Finding from rural South Africa similarly stated greater risk of infant mortality for those born to HIVpositive mothers [25]. Even though it was not stated in other studies, those preterm baby who were born to mothers having history of premature rupture of membrane (PROM) had greater risk of death before discharge than those who had no history of premature rupture of membrane. Since PROM can put the neonate at high risk of developing sepsis which was significantly associated with higher risk of death for the preterm baby, this might be the reason behind of this association. But except maternal history of premature rupture of membrane, neonatal sepsis turned insignificant in multivariate analysis. Compared to moderate to late preterm, very preterm and extremely preterm had greater odds of death in bivariate analysis which is similar to study in southeast Nigeria [3]. Similar to study of Valie-ASR hospital, extremely and very low birth weight preterm births more likely died before discharge when compared to preterm birth with normal weight. But their significance was not repeated in multivariate analysis. Again, the diagnosis of respiratory distress had also shown significant association that those diagnosed with respiratory distress had greater odds of death. This finding is supported with studies in Sub-Saharan Africa and Mettu Karl hospitals, Ethiopia [12,22,26].
Conclusions
Hypertension during pregnancy and maternal HIV infection were factors associated with induced preterm birth. On the other hand, maternal HIV infection, premature rupture of membrane, low APGAR score and respiratory distress were significantly associated with immediate death outcome of preterm birth.
Acknowledgments
For its academic support, Addis Ababa University deserves the gratitude. The three study sites also share gratitude of this study.
References
- WHO (2015) International statistical classification of diseases and related health problems (5thedn), WHO, Geneva, Switzerland.
- Plunkett J, Borecki I, Morgan T, Stamilio D, Muglia LJ (2008) Population-based estimate of sibling risk for preterm birth, preterm premature rupture of membranes, placental abruption and Pre-eclampsia. BMC Genet 6: 1-9.
- Iyoke CA, Lawani OL, Ezugwu EC, Ilechukwu G, Nkwo PO, et al. (2014) Prevalence and perinatal mortality associated with preterm births in a tertiary medical center in South East Nigeria. Int J Womens Health 6: 881-888.
- Mekonnen Y, Tensou B, Telake DS, Degefie T, Bekele A (2013) Neonatal mortality in Ethiopia : trends and determinants. BMC Public Health 13: 483.
- Blencowe H, Cousens S, Oestergaard MZ, Chou D, Moller AB, et al. (2012) National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet 379: 2162-2172.
- Katz J, Lee AC, Kozuki N, Lawn JE, Cousens S, et al. (2013) Mortality risk in preterm and small-for-gestational-age infants in low-income and middle-income countries: a pooled country analysis. Lancet 382: 417-425.
- Debelew GT, Afework MF, Yalew AW (2014) Determinants and Causes of Neonatal Mortality in Jimma Zone, Southwest Ethiopia : A Multilevel Analysis of Prospective Follow Up Study. PLoS One 9: e107184.
- https://www.globalfinancingfacility.org/ethiopia-health-sector-transformation-plan-201516-201920
- Zeitlin J, Szamotulska K, Drewniak N, Mohangoo AD, Chalmers J, et al. (2013) Preterm birth time trends in Europe : a study of 19 countries. BJOG 120: 1356-1365.
- Yuan W, Duffner AM, Chen L, Hunt LP, Sellers SM, et al. (2010) Analysis of preterm deliveries below 35 weeks ’ gestation in a tertiary referral hospital in the UK. A case-control survey. BMC Res Notes 3: 119.
- Kariuki S, Kuile F, Marchant T, Willey B, Katz J, et al. (2012) Neonatal Mortality Risk Associated with Preterm Birth in East Africa, Adjusted by Weight for Gestational Age: Individual Participant Level Meta-Analysis. PLoS Med 9: e1001292.
- Seyom E, Abera M, Tesfaye M, Fentahun N (2015) Maternal and fetal outcome of pregnancy related hypertension in Mettu Karl Referral Hospital. J Ovarian Res 8: 10.
- Crump C, Sundquist K, Sundquist J, Winkleby MA (2011) Gestational age at birth and mortality in young adulthood. JAMA 306: 1233-1240.
- Crump C, Sundquist K, Winkleby MA, Sundquist J (2013) Early-term birth (37-38 weeks) and mortality in young adulthood. Epidemiology 24: 270-276.
- Beck S, Wojdyla D, Say L, Betran AP, Merialdi M, et al. (2010) The worldwide incidence of preterm birth: a systematic review of maternal mortality and morbidity. Bull World Health Organ 88: 31-38.
- Lee ACC, Katz J, Blencowe H, Cousens S, Kozuki N, et al. (2010) National and regional estimates of term and preterm babies born small for gestational age in 138 low-income and middle-income countries in 2010. Lancet Glob Health 1: e26-e36.
- Van den Broek N, Ntonya C, Kayira E, White S, Neilson JP (2011) Preterm birth in rural Malawi: high incidence in ultrasound-dated population. Hum Reprod 20: 3235-3237.
- http://www.europeristat.com/images/doc/EPHR/european-perinatal-health-report.pdf
- DeFranco EA, Lian M, Muglia LA, Schootman M (2008) Area-level poverty and preterm birth risk: A population-based multilevel analysis. BMC Public Health 8: 316.
- Blencowe H, Cousens S, Chou D, Oestergaard M, Say L, et al. (2013) Born Too Soon: The global epidemiology of 15 million preterm births. Reprod Healt 10: S2.
- Adane AA, Ayele TA, Ararsa LG, Bitew BD, Zeleke BM (2014) Adverse birth outcomes among deliveries at Gondar University Hospital, Northwest Ethiopia. BMC Pregnancy Childbirth 14: 90.
- Dalili H, Fallahi M, Moradi S, Nayeri F, Shariat M, et al. (2014) Clinical outcome and cost of treatment and care for neonates less than 1000 grams admitted to Vali-e ASR Hospital. Health Econ Rev 4: 21.
- Zack RM, Golan J, Aboud S, Msamanga G, Spiegelman D, et al. (2014) Risk Factors for Preterm Birth among HIV-Infected Tanzanian Women : A Prospective Study. Obstet Gynecol Int 2014: 261689.
- Kozuki N, Lee ACC, Silveira MF, Sania A, Vogel JP, et al. (2013) The associations of parity and maternal age with small-for-gestational-age, preterm, and neonatal and infant mortality: a meta-analysis. BMC Public Health 13: S2.
- Ndirangu J, Newell M, Bland RM, Thorne C (2012) Maternal HIV infection associated with small-for-gestational age infants but not preterm births: evidence from rural South Africa. Hum Reprod 27: 1846-1856.
- Kinney MV, Kerber KJ, Black RE, Cohen B, Nkrumah F, et al. (2010) Sub-Saharan Africa’s Mothers, Newborns, and Children: Where and Why Do They Die? PLoS Med 7: e1000294.
Citation: Deressa AT, Cherieb A, Negash BT (2018) Factors Associated with Induced Preterm Birth and Its Immediate Outcome in Addis Ababa Public Hospitals, Ethiopia. Neonat Pediatr Med 4: 170. DOI: 10.4172/2572-4983.1000170
Copyright: © 2018 Deressa AT, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4835
- [From(publication date): 0-2018 - Dec 21, 2025]
- Breakdown by view type
- HTML page views: 3941
- PDF downloads: 894