Research Article Open Access
Feasability of a Fine Needle Aspiration and Cytology for Cystic Lesions of the Pancreas During Echo-Endoscopy
Luiz Gustavo de Quadros1,2, Victor Cavaretti1, Roberto Luiz Kaiser Junior2, Josemberg Marins Campos3, Idiberto José Zotarelli Filho2,3*, Fernando Tadeu Vannucci Coimbra1, Rodrigo Tadeu Rodrigo Silvestre1, Mário Flamini Júnior2and Mikaell Alexandre Gouvea Faria21Santa Casa de Misericórdia Hospital, Department of Endoscopy - Education and Training Center of SOBED São Jose do Rio Preto SP Brazil
2Kaiser Clinic - Department of Surgery and Bariatric Endoscopy, São José do Rio Preto -SP -Brazil
3Federal University of Pernambuco, Bariatric Surgery Department, Pernambuco PE Brazil. State University of Sao Paulo-Ibilce-Unesp, Rua Cristovao Colombo 2265, Sao Jose do Rio Preto SP, Brazil
- *Corresponding Author:
- Prof. Dr. Idiberto Jose Zotarelli Filho
University of Sao Paulo- IBILCE-UNESP
Rua Cristovao Colombo 2265
Sao Jose do Rio Preto SP, Brazil
Tel: +55(17)-98166-6537
Fax: +55(17) 98803-7459
E-mail: m.zotarelli@gmail.com
Received date: July 15, 2015 Accepted date: August 5, 2015 Published date: August 13, 2015
Citation:de Quadros LG, Cavaretti V, Kaiser Junior RL, Campos JM, Zotarelli Filho IJ, et al. (2015) Faisability of a Fine Needle Aspiration and Cytology for Cystic Lesions of the Pancreas During Echo-Endoscopy. J Gastrointest Dig Syst 5: 318. doi:10.4172/2161-069X.1000318
Copyright: ©2015 de Quadros LG, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License; which permits unrestricted use; distribution; and reproduction in any medium; provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Background: Cystic pancreatic lesions (LCP) include inflammatory pseudocysts or mesenchymal and epithelial cystic neoplasms in 80-90% and 10-15% of cases, respectively. Other pancreatic cystic lesions include cysts alone, pancreatic policistose (von Hippel-Lindau syndrome), cystic hydatid cyst and metastasis. The prevalence of LCP is about 3.5%. Objective: Was to investigate the clinical application of Biopsy guided by endoscopic ultrasound in patients with pancreatic cystic lesion, considering demographic, endoscopic and cytological data. Methods: We retrospectively studied 24 patients with pancreatic cystic lesion, regardless of sex and race, from the region of São José do Rio Preto, SP, underwent biopsy puncture guided by endoscopic ultrasound. The ecoguide of the punctures were performed using only 22G needle, and the collection and processing of medical liability endoscopist material.
Abstract
Background: Cystic pancreatic lesions (LCP) include inflammatory pseudocysts or mesenchymal and epithelial cystic neoplasms in 80-90% and 10-15% of cases, respectively. Other pancreatic cystic lesions include cysts alone, pancreatic policistose (von Hippel-Lindau syndrome), cystic hydatid cyst and metastasis. The prevalence of LCP is about 3.5%.
Objective: Was to investigate the clinical application of Biopsy guided by endoscopic ultrasound in patients with pancreatic cystic lesion, considering demographic, endoscopic and cytological data.
Methods: We retrospectively studied 24 patients with pancreatic cystic lesion, regardless of sex and race, from the region of São José do Rio Preto, SP, underwent biopsy puncture guided by endoscopic ultrasound. The ecoguide of the punctures were performed using only 22G needle, and the collection and processing of medical liability endoscopist material.
Results: Of the total 24 patients, 11 (45%) were male and 13 (55%) female. The age range 41-78 years (60.3 ± 11.5 years). The endoscopic pancreatic cystic lesion location, the head was more frequent (45.8%), followed body (37.5%) and tail (16.7%). The average lesion area was 425 ± 618 mm2 (range 23-2740 mm2). The homogeneous structure of lesions was detected in 16 (66.7%) patients was identified as the heterogeneous 8 (33.3%).
Discussion: In this study, the endoscopic ultrasound puncture was not effective in obtaining material (high number of samples with unsatisfactory cells) in 41% of patients may be explained by the small size of some lesions, or be an examiner procedure dependent.
Conclusion: It was concluded that the biopsy puncture guided by endoscopic ultrasound in patients with pancreatic cystic lesion was useful in the differential diagnosis between benign and malignant lesions.
Keywords
Cystic pancreatic lesions; Echoendoscopy; Biopsy
Introduction
Cystic pancreatic lesions (LCP) include inflammatory pseudocysts or mesenchymal and epithelial cystic neoplasms in 80-90% and 10-15% of cases, respectively. Other pancreatic cystic lesions include cysts alone, pancreatic policistose (von Hippel-Lindau syndrome), cystic hydatid cyst and metastasis [1,2]. The prevalence of LCP is about 3.5% [1,3]. The diagnosis of these lesions increases with age, with a prevalence of approximately 1% in individuals younger than 40 years can reach 10% in people over 70 years [4].
Furthermore, serous cystic neoplasms represent about 30 % of pancreatic cystic neoplasms, most affecting women in senile phase with about 70 %. Most of these tumors are located in the head of the pancreas and their average size is 7.0 cm. Furthermore, mucinous cystic neoplasms represent about 50% of pancreatic cystic neoplasms, especially in women in pre-senile phase, being more common in the body and tail of the pancreas with an incidence of 80% [5,6].
The technological development of imaging methods as transabdominal ultrasonography (USG), computed tomography (CT), endoscopic retrograde pancreatic cholangiography (ERCP), magnetic resonance cholangiopancreatography (MRCP) and endoscopic ultrasound (EE) have made it possible to identify small pancreatic lesions when most patients are asymptomatic and do not report previous or present history of pancreatic disease [7,8].
In the evaluation of patients with abdominal pain, the diagnosis of LCP has increased due to the increasing use of these tests [9,10]. Digestive endoscopic ultrasound is a test that combines the ultrasound endoscopy and produces, by means of a high frequency transducer of high resolution images [11,12]. It is thin and flexible endoscope, especially equipped with a probe (transducer) miniature ultrasound that is coupled to the end of the apparatus, and enables the realization of ultrasound within the digestive tract [13].
According to the scanning method, this test is classified into radial or linear, and according to clinical indication, in diagnostic or therapeutic. Diagnostic indications include sub-epithelial abnormalities, cancer staging and evaluation of pancreatic and biliary diseases as therapeutic procedures involve as drainage of pancreatic pseudocyst and neurolysis of the celiac artery [14,8]. However, the main obstacle on imaging studies is that there are features that allow differentiation. In addition, despite the impact of the information obtained through this examination in the management of patients with LCP, endoscopic ultrasound is still restricted to a few and large centers in Brazil [15,13].
Studies have shown that isolated tests such as CT and MRI did not have accuracy in differentiating types of LCP [16]. The pancreas is well viewed by both techniques, radial or linear, due to the anatomical situation and direct apposition of the transducer in the gastric and duodenal wall immediately above or next to it [17]. EUS allows detailed study of the parenchyma and pancreatic duct to the fullest extent of the gland without bringing gas or abdominal fat, may identify previously undetected lesions and thereby clarify abnormalities detected by CT and MRI, and is currently considered the gold standard for evaluation of this organ [18,8].
This test is important in the study of these injuries, because the best image in the characterization of cyst morphology (presence of nodulation in the cyst wall, solid component associated) and because of the possibility of biopsy fine needle with collection of material for analysis [19,20]. The puncture of the LCP guided by endoscopic ultrasound with cytological analysis of the aspirate has been used to increase diagnostic accuracy; especially in differentiating adenoma macrocystic serous and mucinous adenoma [21].
Regarding the potential for malignancy, pancreatic cysts are extremely variable. Some are benign and can be handled conservatively while others are malignant or pre-malignant lesions often require surgical treatment [22,23]. Diameter greater than 3 cm and / or the presence of mural nodules appear to be the greatest indicators of malignant transformation [22,24].
Considering the importance of studies on the clinical application of Biopsy guided by endoscopic ultrasound in patients with pancreatic cystic lesion justifies this research because the national literature were not found work with this approach. In addition, the endoscopic point of view morphological characteristics of these injuries (area, location and shape) as well as the analysis of fluid extracted by biopsy puncture essential in defining conduct, which may be conservative or surgical [6].
The objective of this research was to investigate the clinical application of Biopsy guided by endoscopic ultrasound in patients with pancreatic cystic lesion, considering demographic, endoscopic and cytological data.
Study Design
We retrospectively studied 24 patients with pancreatic cystic lesion, regardless of sex and race, from the region of São José do Rio Preto, SP, underwent biopsy puncture guided by endoscopic ultrasound. The procedures were performed in the clinic Gastroimagem of São José do Rio Preto, from September/2013 to June/2014. They were considered as exclusion criteria patients with coagulopathy, pregnant women and those gastrectomized. The major difficulties were in relation to the size of the lesion (less than 0.1 cm). In addition, unsatisfactory samples showed the absence of cells and the volume of aspirated liquid, because the laboratory has difficulty in processing less than 0.1 ml of liquid. This study was approved by the Research Ethics Committee of the Portuguese Beneficent Hospital of São José do Rio Preto.
Methods
Before the exam to study and programming of the same consultation took place. All tests were performed after a minimum fasting for 8 hours. With the patient in the left lateral decubitus, intravenous sedation was performed with propofol and adequate cardiopulmonary monitoring during the examination. Then it was introduced echoendoscope Pentax EG-3630U (Pentax, Tokyo, Japan) by mouth. The pancreas was visualized by plotting the apparatus for evaluation of the duodenal bulb of the head of the pancreas and a large curve for evaluation of gastric and pancreatic body tail. The pancreatic duct was measured in the portion of the body and in the area of confluence after splenorenal image freeze on ultrasound. The images were transferred to processing Pentax EPM-3500 and ultrasound Hitachi EUB-525, coupled to computer drive containing the Ikap program (SS computer version 1:53, Porto Alegre, RS).
The ecoguide of the punctures were performed using only 22G needle, and the collection and processing of medical liability endoscopist material. There was no pathologist present in the procedure room for evaluation of the material during the examination. The material was sent to the pathology laboratory Lapat, São José do Rio Preto, SP on the same day of collection. All the collected material was evaluated for cytology.
Statistical Analysis
When the patient recovered his level of consciousness, it was released along with her companion. In assessing the ultrasound area because the area in mm² not follow Gaussian distribution according to the factors, it used the natural logarithm, and the analysis done on this scale, because then the variable has lognormal distribution. In the average data analysis were compared by t-test (two-sample t), when they were two categories in comparison, and analysis of variance (ANOVA one way) to a classification criterion. Associations were assessed in cross frequency tables using the chi-square test of Pearson, and the chi-square for distance Hellinger. The association between location of pancreatic cystic lesion and Pap result was obtained using the chi-square test by dependency analysis (Lamb, 1987). Significance level was admitted to value p=0.05. Data were analyzed using the program Minitab Statistical Software 12:22 (Minitab Inc, State College Pennsylvania, United States).
Results
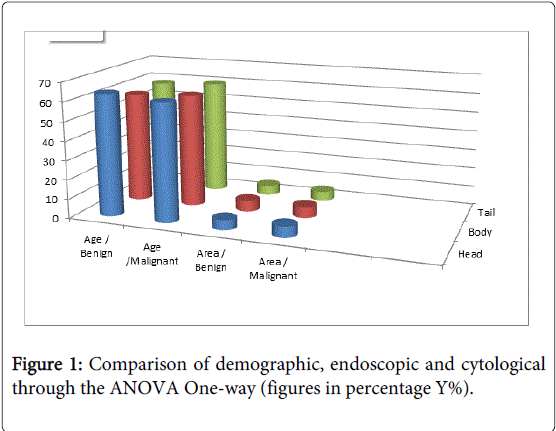
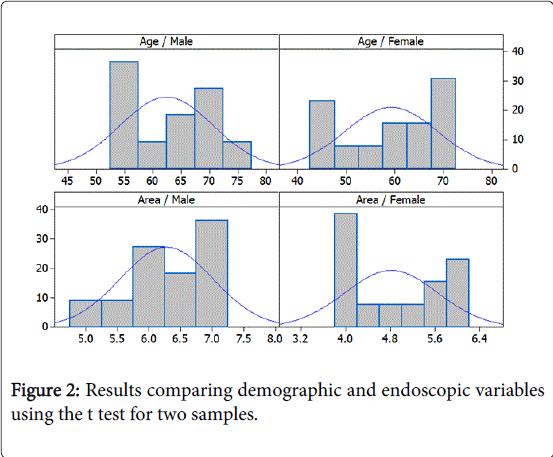
Of the total 24 patients, 11 (45%) were male and 13 (55%) female. The age range 41-78 years (60.3 ± 11.5 years). The endoscopic pancreatic cystic lesion location, the head was more frequent (45.8%), followed body (37.5%) and tail (16.7%) (Figure 1). The average lesion area was 425 ± 618 mm2 (range 23-2740 mm2). The homogeneous structure of lesions was detected in 16 (66.7%) patients was identified as the heterogeneous 8 (33.3%) (Figure 2). The liquid varied from 0.5 mL to 40.0 mL, according to the size of the lesion.
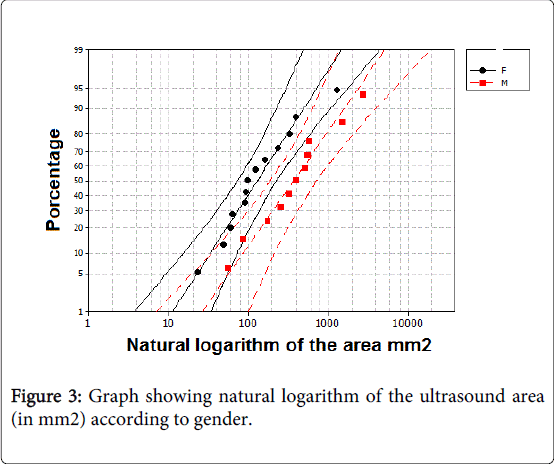
The results of the cytological diagnosis showed that 45.8% of patients in the lesion was benign, malignant 12.5% and 41.7% was unsatisfactory, i.e., the material collected was insufficient for cytopathological analysis (Figure 3) .
The average age of female patients was 57.8 ± 12 years while the male was 63.4 ± 10.6 years. Comparing age to gender using the t test for two samples did not present statistical significance (p=0.24).
The average age of patients with pancreatic cystic lesion was higher in those with benign lesion compared with malignant and unsatisfactory, with no significant difference (p=0.94) (Table 1).
| Comparation | variables | P | |||
| gender x cytopatologic | benign | malignant | unsatisfactory | Total | |
| male | 5 (45,5 %) | 1 (9,0%) | 5 (45,5%) | 11 (100%) | |
| female | 6(46,2%) | 2 (15,3%) | 5 (38,5%) | 13(100%) | 0.88 |
| Total | 11 (45,9%) | 3 (12,4%) | 10 (41,7%) | 24 (100%) | |
| gender x localization | Head | Body | Tail | Total | |
| Male | 4(36,4%) | 5 (45,5%) | 2 (18,1%) | 11(100%) | |
| Female | 7(53,9%) | 4 (30,8%) | 2 (15,3%) | 3 (100%) | 0.68 |
| Total | 11(45,8%) | 9 (37,5%) | 4 (16,7%) | 24 (100%) | |
| cytopatologic x local | Head | Body | Tail | Total | |
| Benign | 8 (72,7%) | 3 (27,3%) | 0 (0,0%) | 11(100%) | |
| Malignant | 0 (0,0%) | 1 (33,3%) | 2 (66,7%) | 3 (100%) | 0.001 |
| Unsatisfactory | 3 (30,0%) | 5 (50,0%) | 2 (20,0%) | 10(100%) | |
| Total | 11(45,8%) | 9 (37,6%) | 4 (16,6%) | 24(100%) |
Table 1: Comparison of results between demographic, endoscopic and cytopathologic using the chi-square test for distance Hellinger.
The age range of patients whose anatomical location of pancreatic cystic lesion was head of the pancreas was higher compared to body and tail, with no statistically significant difference (p=0.49) (Table 1).
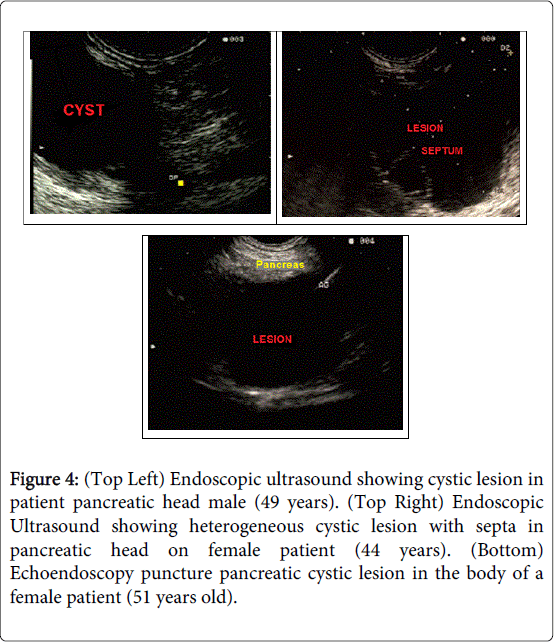
Comparing the area of pancreatic cystic lesion depending on the location, there was a larger area in the body over the head and tail, not being a significant difference (p=0.20) (Table 1). The result of the comparison between area and cytological results showed larger area in malignant lesions, with no significant difference (p=0.20) (Table 1). The analysis of age by sex showed that males have a higher age (p=0.24) and significantly higher average natural logarithm of the ultrasound area (p=0.029) than females. Because of the log is increasing function it follows that if there is evidence of the arithmetic mean of the logarithm be higher in men (Figure 4).
Figure 4: (Top Left) Endoscopic ultrasound showing cystic lesion in patient pancreatic head male (49 years). (Top Right) Endoscopic Ultrasound showing heterogeneous cystic lesion with septa in pancreatic head on female patient (44 years). (Bottom) Echoendoscopy puncture pancreatic cystic lesion in the body of a female patient (51 years old).
Comparing cytological findings and gender x location there was no significant difference (Table 1). Comparing cytological findings x location note a significant association between benign lesions and pancreatic head (p = 0.001). The dependency analysis shows a positive association between head and gentleness, with poor body and tail with malignancy. The diagram shows 98% of the association structure. The first factor explains 88% of total dependence and order kindness, unsatisfactoriness and malignancy, while laying in the same order head, body and tail, hence the positive association described before; The second factor explains 10% of total dependence and yet its share in total dependence is small he also "sees" the same dichotomy that factor 1: head and kindness very close in a quadrant 'against' the pairs of Pap and local next one probably closer than the other, namely body with unsatisfactoriness and tail with malignancy.
Discussion
Pancreatic cysts can be classified as "true" when there epithelium coating the injury or pseudocyst, which is surrounded by an isolated collection of granulation tissue and fibrosis, usually the result of acute or chronic pancreatitis [6]. These cysts are usually divided into mucinous cystic neoplasms, intraductal papillary mucinous neoplasms, serous cystadenoma and solid tumor pseudopapillary (Frantz tumor) [25].
With the development of imaging methods and better access to them by patients, there was an increase in the diagnosis of cystic pancreatic lesions [1,26]. The endoscopic ultrasound with fine needle assists and complements the diagnosis, revolutionizing the approach, today the gold standard in the study of these lesions. Thanks to endoscopic ultrasound, injuries that were addressed surgically, due to lack of definitive diagnosis can currently be treated endoscopically or be accompanied periodically, depending on their characteristics [27,28].
In this study, the endoscopic ultrasound puncture was not effective in obtaining material (high number of samples with unsatisfactory cells) in 41% of patients may be explained by the small size of some lesions, or be an examiner procedure dependent. Perhaps only by the sonographic features as morphology, shape and content of these injuries could be followed conservatively by conducting regular reviews.
The statistical significance found among larger area of injury in males may have association with the further development of these male injury or delay in seeking medical monitoring. The finding of as many cystic lesions in women is consistent with the [29] literature. The same applies to the age of diagnosis of lesions around the seventh decade of life [4].
Conclusion
It was concluded that the biopsy puncture guided by endoscopic ultrasound in patients with pancreatic cystic lesion was useful in the differential diagnosis between benign and malignant lesions. As a corollary, pancreatic cystic lesion was more frequent in female patients between sixth and seventh decades of life and the geometric mean area of lesions was statistically higher in male patients. There was also a significant association between benign lesions located in the head of the pancreas and malignant lesions located in the tail.
Research Ethics Committee
This study was approved by the Ethics Research Committee of the Portuguese Beneficent Hospital of Sao Jose do Rio Preto under the case number 836 411 of 10/17/2014.
Acknowledgements
We appreciate all patients who agreed to Cooperate with this study, and we thank the doctors and staff of the Kaiser Clinic of São Jose do Rio Preto SP and the entire endoscopy team at Santa Casa de Misericordia Hospital of Sao Jose do Rio Preto SP.
References
- (2015) OMS- Organização Mundial de Saúde. Disponível em: Acesso em: 30 de março de.
- IBGE- Instituto Brasileiro de Geografia e Estatística. Disponível em.
- de Jong K, Nio CY, Hermans JJ, Dijkgraaf MG, Gouma DJ, et al. (2010) High prevalence of pancreatic cysts detected by screening magnetic resonance imaging examinations. Clin Gastroenterol Hepatol 8: 806-811.
- de Jong K, Poley JW, van Hooft JE, Visser M, Bruno MJ, et al. (2011) Endoscopic ultrasound-guided fine-needle aspiration of pancreatic cystic lesions provides inadequate material for cytology and laboratory analysis: initial results from a prospective study. Endoscopy 43: 585-590.
- Lee LS (2014) Incidental Cystic Lesions in the Pancreas: Resect? EUS? Follow? Curr Treat Options Gastroenterol 12: 333-349.
- Clores MJ, Thosani A1, Buscaglia JM1 (2014) Multidisciplinary diagnostic and therapeutic approaches to pancreatic cystic lesions. J Multidiscip Healthc 7: 81-91.
- Layfield LJ, Ehya H, Filie AC, Hruban RH, Jhala N, et al. (2014) . Utilization of ancillary studies in the cytologic diagnosis of biliary and pancreatic lesions: the Papanicolaou Society of Cytopathology guidelines for pancreatobiliary cytology. Diagn Cytopathol 42: 351-362.
- Guaraldi S, Sá E, Romano S, Carvalho ACP (2005) O papel da ecoendoscopia no diagnóstico das neoplasias císticas primárias do pâncreas. Radiol Bras 38: 451-458.
- Lee KH, Lee SJ, Lee JK, Ryu JK, Kim EY, et al. (2014) Prediction of malignancy with endoscopic ultrasonography in patients with branch duct-type intraductal papillary mucinous neoplasm. Pancreas 43: 1306-1311.
- Wright GP, Morrow JB, Shaheen M, Goslin BJ, Baatenburg L, et al. (2014) Accuracy of endoscopic ultrasound in the evaluation of cystic pancreatic neoplasms: a community hospital experience. Pancreas 43: 465-469.
- Chebib I, Yaeger K, Mino-Kenudson M, Pitman MB (2014) The role of cytopathology and cyst fluid analysis in the preoperative diagnosis and management of pancreatic cysts >3 cm. Cancer Cytopathol 122: 804-809.
- Sahani DV, Kambadakone A, Macari M, Takahashi N, Chari S, et al. (2013) Diagnosis and management of cystic pancreatic lesions. AJR Am J Roentgenol 200: 343-354.
- Maluf-Filho F, Dotti CM, Farias AQ, Kupski C, Chaves DM, et al. (2007) [I Brazilian consensus of endoscopic ultrasonography]. Arq Gastroenterol 44: 353-358.
- Gardner TB, Glass LM, Smith KD, Ripple GH, Barth RJ, et al. (2013) Pancreatic cyst prevalence and the risk of mucin-producing adenocarcinoma in US adults. Am J Gastroenterol 108: 1546-1550.
- Morris-Stiff G, Falk GA, Chalikonda S, Walsh RM (2013) Natural history of asymptomatic pancreatic cystic neoplasms. HPB (Oxford) 15: 175-181.
- Chung JW, Chung MJ, Park JY, Bang S, Song SY, et al. (2013) Clinicopathologic features and outcomes of pancreatic cysts during a 12-year period. Pancreas 42: 230-238.
- Ardengh JC, Goldman SM, Lima-Filho ÉR (2011) Papel atual dos métodos de imagem no diagnóstico das neoplasias císticas e sólidas do pâncreas: 1ª parte. Rev Col Bras Cir 38:133-138.
- Farrell JJ, Fernández-del Castillo C (2013) Pancreatic cystic neoplasms: management and unanswered questions. Gastroenterology 144: 1303-1315.
- Hawes RH, Clancy J, Hasan MK (2012) Endoscopic ultrasound-guided fine needle aspiration in cystic pancreatic lesions. Clin Endosc 45: 128-131.
- Vilmann P, Jacobsen GK, Henriksen FW, Hancke S (1992) Endoscopic ultrasonography with guided fine needle aspiration biopsy in pancreatic disease. Gastrointest Endosc 38: 172-173.
- de Jong K, Nio CY, Hermans JJ, Dijkgraaf MG, Gouma DJ, et al. (2010) High prevalence of pancreatic cysts detected by screening magnetic resonance imaging examinations. Clin Gastroenterol Hepatol 8: 806-811.
- Tanaka M, Fernández-del Castillo C, Adsay V, Chari S, Falconi M, et al. (2012) International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology 12: 183-197.
- Valsangkar NP, Morales-Oyarvide V, Thayer SP, Ferrone CR, Wargo JA, et al. (2012) 851 resected cystic tumors of the pancreas: a 33-year experience at the Massachusetts General Hospital. Surgery 152: S4-12.
- Tanaka M, Chari S, Adsay V, Fernandez-del Castillo C, Falconi M, et al. (2006) International consensus guidelines for management of intraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreas. Pancreatology 6: 17-32.
- Zamboni G, Klöppel G, Hruban RH, Longnecker DS, Adler G (2000) Mucinous cystic neoplasms of pancreas. In: Aaltonen LA, Hamilton, SR, eds. World Health Organization Classification of Tumours. Pathology and genetics of tumours of the digestive system. Lyon: IARC Press; 2000: 234.
- Cordeiro JA (1987) Analysis of dependency. Relatório Técnico 48/87. Instituto de Matemática - Unicamp. Campinas.
- Compagno J, Oertel JE (1978) Mucinous cystic neoplasms of the pancreas with overt and latent malignancy (cystadenocarcinoma and cystadenoma). A clinicopathologic study of 41 cases. Am J Clin Pathol 69: 573-580.
- Compagno J, Oertel JE (1978) Microcystic adenomas of the pancreas (glycogen-rich cystadenomas): a clinicopathologic study of 34 cases. Am J Clin Pathol 69: 289-298.
- Valsangkar NP, Morales-Oyarvide V, Thayer SP, Ferrone CR, Wargo JA, et al. (2012) 851 resected cystic tumors of the pancreas: a 33-year experience at the Massachusetts General Hospital. Surgery 152: S4-12.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 14775
- [From(publication date):
August-2015 - Aug 30, 2025] - Breakdown by view type
- HTML page views : 10141
- PDF downloads : 4634