Fast Track Surgery in Bariatric Surgery: Prospective Analysis of 80 Patients-A Randomized Controlled Trail
Received: 23-Apr-2018 / Accepted Date: 04-Jul-2018 / Published Date: 06-Jul-2018 DOI: 10.4172/2165-7904.1000369
Keywords: Bariatric surgery; Rapid rehabilitation surgery; Fast- Track surgery; Nutritional status; Postoperative complications
Abbreviations
T2DM: Type 2 Diabetes Mellitus; PCOS: Polycystic Ovarian Syndrome; OSAS: Obstructive Sleep Apnea Syndrome
Introduction
Fast track surgery (FTS) is an innovative concept of diagnosis and treatment put forward by Kehlet et al. to speed up patients’ recovery after surgery [1]. During decades of its development, the clinical safety and usefulness of FTS in gastric cancer and colon cancer have been constantly established by its wide application in multicenter clinical practice [2,3].
Weight loss-metabolic surgery, or more famously known as Bariatric surgery, has been in upward trend in recent years as to treat patients with morbid obesity and metabolic disorders [4]. Since the prevalence of obesity and type 2 diabetes is very high in China, bariatric surgery is getting more and more acknowledged and demanded. Laparoscopic Sleeve Gastrectomy (LSG) is the most commonly performed bariatric surgery in China, mainly due to its simplicity and less severe complications when compared to gastric bypass [5]. The guidelines for bariatric surgery in China differs than that of western counterparts. In China, bariatric surgery is indicated for patients with BMI ≥ 32.5 Kg/m2, or BMI ≥ 27.5 kg/m2 complicated with any obesity-related comorbidities or BMI 25.0-27.5 kg/m2 with T2DM whom personally electing to undergo bariatric surgery [6].
Where in western counterparts, patients with BMI ≥ 40 kg/m2 or BMI 35-40 kg/m2 with co-morbidities are indicated for bariatric surgery [7].
Bariatric patients have higher expectations regarding to their “postoperative life-quality improvements” than that of more debilitating patients (e.g. cancer). Hence, we felt the application of FTS protocol is very much suitable as to improve the postoperative recovery quality. The idea is that application of FTS protocol to patients receiving bariatric surgery may bring more benefits to their recovery.
This study prospectively divided the bariatric patients into those who received the FTS protocol with those who received the traditional non-FTS method. But since both bariatric surgery and FTS protocol are very much a fresh topic in the minds of Chinese “non-medical” individuals, some adjustment was needed.
Methods
Data collection
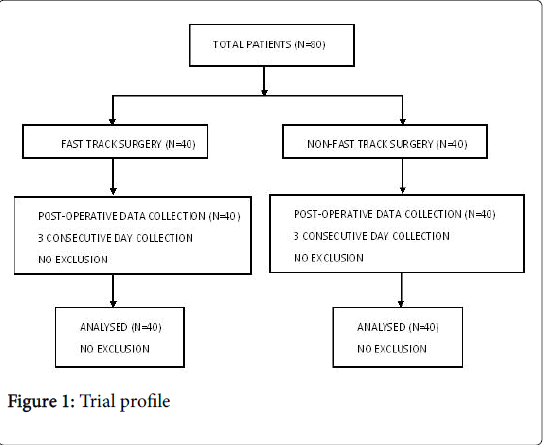
This study was performed at The Affiliated Hospital of Xuzhou Medical University, Department of Gastrointestinal Surgery, Jiangsu Province, China. 80 patients with morbid obesity and metabolic disorders receiving bariatric surgery (LSG, n=80) from September 2016 to September 2017 were selected. The patients were randomly divided into 2 equal groups, FTS group (40 patients) and non-FTS group (40 patients). A total of 40 males and 40 females, with an average age of 34.6 ± 10.2 years (range, 16-71 years) and a body mass index of 37.9 ± 6.6 Kg/m2 (26-59 Kg/m2). The patient's general information and co-metabolic disorders were recorded and analyzed.
Inclusion criteria: According to the 2014 China’s guidelines for surgical treatment of obesity and type 2 diabetes, bariatric surgery is indicated for those whom BMI ≥ 32.5 Kg/m2, or BMI ≥ 27.5 Kg/m2 complicated with obesity-related comorbidities, or BMI 25.0-27.5 Kg/m2 with T2DM whom personally electing to undergo bariatric surgery [6]. Signed informed consent form.
Exclusion criteria: Patients’ refusal to cooperate (including not willing to sign the consent form). Severe cardiopulmonary disease cannot tolerate surgery. Serious psychological difficulties
This study was approved by the ethics committee of our hospital and signed consent formed by the patient was required.
Management scheme
Patients were diagnosed with morbid obesity alone or complicated with metabolic diseases, and the necessary laboratory and imaging examinations were performed to clarify the patient's condition and to exclude any surgical contraindications for bariatric surgery.
Both FTS and Non-FTS group received similar general anesthesia, equal dosage and duration of antibiotics were given (intraoperative and 1 day postoperatively), high-risk patients received low molecular weight heparin 6000 u as anticoagulant therapy [6], placement of one abdominal drainage (removed when there was no abnormality in the drained fluid’s color, and daily volume is less than 20 ml). Additionally, leak test was not performed for both groups.
FTS group: a) Pre-operative preparation allowed patients to begin fasting 6 hours before operation, orally ingest 250 ml of 5% glucose water 2 hours before operation (contraindicated in diabetic patients), and no bowel preparation was performed.
b) Intra-operatively limit the volume of fluids inflow (under 1500 ml), additional heat preservation using heater blanket and blower, and peritoneal rinsing using heated warm saline.
c) Post-operatively to allow water intake 6 hours after anesthesia recovery, advocate early feeding starting with liquid diet (without the normal routine of waiting for flatus or bowel movement), early ambulation (within 24 hours).
d) Additionally, nasogastric (NG) tube, together with the calibration bougie was placed immediately after anesthesia and removed as soon as the stomach was completely resected.
e) Postoperatively, analgesic pumps are not routinely used. For individual patients requiring analgesia, non-steroidal analgesics (flurbiprofen) may be given intravenously. High-risk patients received low molecular weight heparin 6000 u as anticoagulant therapy [6].
Non-FTS group: a) Pre-operative preparation allowed patients to begin fasting 12 hours before operation, prohibit water intake 4 hours before operation, and bowel preparation was performed one night before operation through take oral laxatives (Bowel preparation is given as a standard nursing regulation in our Gastrointestinal Surgery department).
b) Intra-operatively, volume of fluids inflow was not limited, additional heat preservation was not used.
c) Post-operatively to allow oral ingestion only after flatus.
d) Additionally, NG tube was placed preoperatively after anesthesia and removed when patients started flatus. This follows the routine traditional non-FTS method.
e) Postoperative analgesia with analgesia pump was routinely given, and similar antithrombotic regimen as with the FTS group was given to those at high risk of thrombosis.
All patients performed upper GI series before discharge.
The discharge criteria were: body temperature <37.3oC, no tachycardia, no signs of wound infection and no other complications. Forms of bariatric diet guidance and schedule for follow-up was given.
Observation index
The operation time, blood loss, postoperative hospital stay, hospitalization expenses, postoperative first flatus time, postoperative first time food intake, days of NG tube placement and complications were recorded. The pain score using NRS pain scale was recorded 1-3 days after operation [8]. Laboratory values such as albumin and Prealbumin were monitored before operation and 3 days after operation. The levels of stress indicators such as WBC count and neutrophil before operation and 3 days after operation were also recorded.
Statistics
Continuous data is recorded as mean ± standard deviation (SD). Differences between the groups were assessed by t-test and Mann- Whitney test. Classification data were analyzed using Fisher's exact test and Pearson's chi-square test. p-value less than 0.05 difference was statistically significant. Statistics using SPSS version 19.0 statistical software shown in Figure 1.
Result
Pre-operative data of two groups of patients
From September 2016 to September 2017, a total of 80 patients with morbid obesity and metabolic disorders underwent bariatric surgery (LSG, n=80). The patients were divided into FTS group (40 cases) and non-FTS group (40 cases). A total of 40 males and 40 females, with an average age of 35.2 ± 10.3 (16-71 years) and body mass index of 37.9 ± 6.6 Kg/m2 (26-59 Kg/m2) underwent bariatric surgery. Patients with metabolic disorders include: hypertension, type II diabetes, hyperthyroidism, sleep apnea syndrome, muscle and joint pain. There were no significant differences in age, sex, BMI and metabolic disorder (Table 1).
| Value | Age (year) | Sex (M/F) | BMI (kg/m2) | Comorbidities (%) | |||
|---|---|---|---|---|---|---|---|
| T2DM | Hypertension | PCOS | OSAS | ||||
| FTS (n=40) | 34.6 ± 10.2 | 21/19 | 38.7 ± 6.4 | 5(12.5) | 4(10) | 2(5) | 15(37.5) |
| Non-FTS (n=40) | 34.8 ± 10.1 | 19/21 | 37.2 ± 6.9 | 8(20) | 6(15) | 1(2.5) | 19(47.5) |
| Statistical value | 0.012 | 0.2 | 1.086 | 0.827 | 0.457 | --- | 0.818 |
| P-value | 0.913 | 0.655 | 0.0.301 | 0.361 | 0.498 | 0.553 | 0.365 |
Table 1: Pre-operative data of two groups of patients
Surgical data and postoperative recovery status comparison
The operation information and postoperative recovery of the two groups were compared. The FTS group was significantly shorter in postoperative hospital stay than in the Non-FTS group, also in postoperative first flatus, postoperative first food intake time, NG tube time. There was no significant difference in the surgical methods and operation time, bleeding volume and the incidence of postoperative complications (Table 2).
| Parameters | FTS(n=40) | Non-FTS(n=40) | P value |
|---|---|---|---|
| Surgical methods (LSG) | 40 | 40 | --- |
| Operation time (min) | 163.0 ± 46.5 | 171.9 ± 38.4 | 0.352 |
| Bleeding volume (ml) | 42.3 ± 31.3 | 44.0 ± 35.4 | 0.815 |
| Postoperative hospital stay (d) | 3.3 ± 1.2 | 5.0 ± 2.4 | 0 |
| Hospital expenses (CNY) | 61261.01 ± 3812.2 | 63386.8 ± 7018.9 | 0.096 |
| First flatus (d) | 1.88 ± 0.69 | 2.50 ± 0.72 | 0 |
| First postoperative food intake (d) | 1.73 ± 0.56 | 2.55 ± 0.68 | 0 |
| Gastric tube indwelling duration (d) | 0.05 ± 0.22 | 1.18 ± 0.59 | 0 |
Table 2: Surgical data and postoperative recovery status comparison
Postoperative complications
There was no significant difference in postoperative complications (bleeding, leakage, sepsis) between the two groups (P>0.05) (Table 3).
| Parameters | Bleeding (%) | Leakage | Sepsis |
|---|---|---|---|
| FTS (n=40) | 0 | 0 | 0 |
| Non-FTS (n=40) | 1 (2.5) | 0 | 0 |
| P-value | 1 | --- | --- |
Table 3: Comparison of postoperative complications between the FTS group and the Non-FTS group.
Postoperative bleeding occurred in 1 case of non-FTS group, which was improved after conservative treatment using hemostatic drugs.
Pain score and stress indicators comparison
Pain score record for 3 consecutive post-operative days shows no significant difference between the two groups. The FTS group postoperative 3 day stress response was less than the non-FTS group, although this difference was not statistically significant (Table 4).
| Value | Pain Score | WBC (109/L) | Neutrophil (109/L) | ||||
|---|---|---|---|---|---|---|---|
| POD 1 | POD 2 | POD 3 | Pre-operation | POD 3 | Pre-operation | POD 3 | |
| FTS (n=40) | 5.00 ± 1.04 | 2.93 ± 1.00 | 1.38 ± 0.54 | 8.0 ± 2.2 | 10.9 ± 2.1 | 4.9 ± 1.6 | 8.6 ± 2.1 |
| Non-FTS (n=40) | 4.85 ± 0.95 | 2.73 ± 0.78 | 1.43 ± 0.50 | 8.5 ± 2.5 | 13.0 ± 2.5 | 5.2 ± 2.2 | 10.00 ± 2.3 |
| Statistical value | 0.455 | 0.994 | 0.184 | 0.852 | 15.247 | 0.564 | 8.096 |
| P-value | 0.502 | 0.322 | 0.669 | 0.259 | 0 | 0.455 | 0.006 |
Table 4: Pain score and stress indicators comparison.
Nutritional status comparison
The FTS group and Non-FTS group in terms of post-operative nutritional status, we compared the pre-operative and post-operative 3rd day albumin and pre-albumin values. There were no significant differences in pre-operative albumin and pre-albumin between the FTS group and Non-FTS group, while also noting that the FTS group levels of albumin and pre-albumin were higher than those of the Non- FTS group on the post-operative 3rd day (Table 5).
| Value | Albumin (g/L) | Pre-albumin (g/L) | ||
|---|---|---|---|---|
| Pre-operation | POD 3 | Pre-operation | POD 3 | |
| FTS (n=40) | 45.3 ± 2.7 | 38.3 ± 3.7 | 0.29 ± 0.07 | 0.24 ± 0.05 |
| FTS (n=40) | 45.6 ± 3.9 | 35.7 ± 4.0 | 0.27 ± 0.07 | 0.20 ± 0.05 |
| Statistical value | 0.127 | 9.031 | 1.105 | 9.797 |
| P-value | 0.723 | 0.004 | 0.296 | 0.002 |
Table 5: Nutritional status comparison.
Discussion
FTS is a surgical concept that aims to reduce surgical pre-operative stress, reduce the incidence of post-operative complications and therefore speed-up the post-operative recovery process [1]. The concept of FTS was first used in colorectal surgery [2]. In its development and continual standardization, multicenter clinical results show that FTS can reduce post-operative morbidity and post-operative stress status [9]. Since 2015, our center has introduced the concept of FTS to carry out the work of bariatric surgery, and has achieved good results in clinical practice compared with the traditional surgical procedures.
We conclude that the key points of FTS in bariatric surgery are as follows: (a) pre-operatively to inform the patient about the surgical plan and the rapid rehabilitation of the surgical procedure, and to assess whether the psychological state of the patient can complete the diagnosis and treatment process. Furthermore, no longer emphasize the pre-operative 12-hour meal fasting and 4-hour water fasting and that supplementing clear liquid 2 hours before surgery will not increase the risk of anesthesia aspiration [10-13]. Studies have also shown that pre-operative food intake can also reduce post-operative insulin resistance [14-16]. (b) Intra-operative: Intra-operative attention to patient insulation. During general anesthesia, tracheal intubation, mechanical irritation and postoperative throat discomfort are reduced by spraying anesthesia on the catheter surface. NG tube were routinely placed after anesthesia as to decompress the gastric and removed as soon as the stomach is transected. In terms of the placement of the abdominal drainage, although placement of abdominal drainage is not recommended in FTS protocol [17], we still placed a single drainage and removed it the day the patient was to be discharged. The reason is that bariatric patients have higher expectations (as they are not burdened by debilitating diseases such as cancer) and should be treated carefully. Furthermore, we felt that placement of single small abdominal drainage can act as a safety measure, in case complications such as bleeding or leakage occurs. In one of the case that occurred bleeding complications, the abdominal drain prevented the formation of hematomas and allowed us to manage the patients conservatively. (c) Post-operatively to recommend early post-operative oral feeding, starting with liquid diet. Encourage patients for early ambulation. Long-term bed rest will not only reduce muscle strength, but also increase the risk of pneumonia, lower extremity thrombosis (DVT). Only provide analgesic medications if needed. It should be noted that all the procedures should be carried out under the premise of surgical safety.
Difficulties in the clinical implementation process are: (a) the patient's understanding and coordination; (b) fear of surgery, that is some patients find it difficult to accept the early feeding and early ambulation; (c) furthermore, some patients were not willing for early discharge. While most countries that follows FTS protocol discharged their patients 1 day postoperatively, in China it was not the case. Although we allow them to be discharged early, the patients themselves were not willing, as they felt they would be much safer and healthier to stay admitted for few days more. Such shows the need for more communication and education about FTS to the patients in China.
The application of the FTS in bariatric surgery is more beneficial than the traditional model. This prospective study illustrates by comparative analysis under the premise that there was no difference in general data and metabolic disorders in the two groups of patients: The first food intake time and first flatus time in the FTS group were earlier than those in the non-FTS group (P<0.05). The FTS group had earlier removal of the NG tube to relieve discomforts. In non-FTS group, following the traditional method, NG tube was removed routinely on postoperative day 1. Postoperative hospitalization time between the two groups showed similar results comparing to J. Perine study [7], FTS group is 3.3 ± 1.2 d, earlier than the non-FTS group 5.0 ± 2.4 d (P<0.05). The postoperative hospitalization time of bariatric patients in China is still longer than the average discharge time in other countries [18], indicating for a room of improvement in bariatric surgery in China.
Patients in the FTS group did not use analgesia pump for postoperative analgesia and intravenous analgesics (dezocine/flurbiprofen axetil injection) were given only on demand. However, there was no significant difference in pain scores between the two groups after 3 days post-operatively. The reason may be that the bariatric surgery is “surgically” less invasive than that of the more radical cancer surgery. The WBC counts and neutrophil counts of FTS group were lower than those of non-FTS group 3 days postoperatively, which further indicate that the concept of FTS could reduce post-operative stress and promote recovery.
One of the most important differences between the two groups was the postoperative values of albumin and pre-albumin in the FTS group (38.3 ± 3.7 g/L and 0.24 ± 0.05 g/L, respectively), all higher than (35.7 ± 4.0 g/L and 0.20 ± 0.05 g/L, respectively) in non-FTS group (p<0.05). FTS group recommended earlier feeding and early ambulation, promoting postoperative digestive tract function recovery. Studies have shown that early oral feeding can reduce catabolism and reduce the risk of infection without increasing the incidence of leakage [19].
FTS is used nowadays in many centers and achieved good results. FTS, or also known as Rapid Rehabilitation Surgery, has been consistently demonstrated shorter hospital stays and lower rates of complications without increasing the risk of surgery itself. However, whether FTS will increase the rate of re-hospitalization may very well be different [18,20]. In our study, one patient in the control group had postoperative bleeding (1/80) after operation. The patient drainage bag revealed bloody fluid on the first day after operation, hemostatic drugs were then given to the patient and recovered well. The remaining patients had no serious complications. There was no new postoperative complication in patients who were followed up for 1 month. This shows that the application of FTS for bariatric patients can be performed safely and does not interfere with the surgery itself or promoting early complications.
Currently there is a lack of thorough FTS standard for bariatric patients [21]. We recommend that high-risk patients should be excluded from the FTS model, waiting for a higher level of clinical evidence which may improve the current treatment protocols. Due to the limited number of patients in our study, further multicenter randomized controlled trials are needed to confirm the safety and efficacy of FTS in bariatric surgery.
Conclusion
The use of FTS concept in patients undergoing bariatric surgery is safe and reliable, shortened post-operative hospital stay, reduces stress and speed up post-operative nutrition recovery, should be recommended in bariatric surgery practice.
References
- Kehlet H (1997) Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth 78: 606-617.
- Anderson AD, McNaught CE, MacFie J, Tring I, Barker P, et al. (2003) Randomized clinical trial of multimodal optimization and standard perioperative surgical care. Br J Surg 90: 1497-1504.
- Tanaka R, Lee SW, Kawai M, Tashiro K, Kawashima S, et al. (2017) Protocol for enhanced recovery after surgery improves short-term outcomes for patients with gastric cancer: A randomized clinical trial. Gastric Cancer 20: 861-871.
- Mazzarella M (2017) Erratum to: Abstracts from the 22nd World Congress of the International Federation for the Surgery of Obesity & Metabolic Disorders (IFSO), London, 29 August-2 September 2017. Obes Surg 27: 2779-2779.
- Bischoff JM, Enghuus C, Werner MU, Kehlet H (2013) Long-term follow-up after mesh removal and selective neurectomy for persistent inguinal postherniorrhaphy pain. Hernia 17: 339-345.
- Liu JG (2014) China's guidelines for surgical treatment of obesity and type 2 diabetes (2014). Chin J Prac Surg 11: 1005-2208.
- Fried M, Yumuk V, Oppert JM, Scopinaro N, Torres A, et al. (2014) Interdisciplinary European guidelines on metabolic and bariatric surgery. Obes Surg 24: 42-55.
- Caprini JA (2005)Thrombosis risk assessment as a guide to quality patient care. Dis Mon 51: 70-78.
- Varadhan KK, Neal KR, Dejong CH, Fearon KC, Ljungqvist O, et al. (2010) The enhanced recovery after surgery (ERAS) pathway for patients undergoing major elective open colorectal surgery: A meta-analysis of randomized controlled trials. Clin Nutrit 29: 434-440.
- Perinel J, Adham M (2016) ERAS and pancreatic surgery: A review. Updates in Surgery 68: 253-255.
- Pimenta GP, Nascimento JEA (2014) Prolonged preoperative fasting in elective surgical patients: why should we reduce it? Nutr Clin Pract 29: 22-28.
- Maltby JR (2006) Fasting from midnight-the history behind the dogma. Best Pract Res Clin Anaesthesiol 20: 363-378.
- American Society of Anesthesiologists Committee (2011) Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: Application to healthy patients undergoing elective procedures: An updated report by the American Society of Anesthesiologists Committee on standards and practice parameters. Anesthesiology 114: 495-511.
- Ljungqvist O, Nygren J, Thorell A (2000) Insulin resistance and elective surgery. Surgery 128: 757-760
- Awad S, Varadhan KK, Ljungqvist O, Lobo DN (2013) A meta-analysis of randomised controlled trials on preoperative oral carbohydrate treatment in elective surgery. Clin Nutr 32: 34-44.
- Scott MJ, Baldini G, Fearon KCH, Feldheiser A, Feldman LS, et al. (2015) Enhanced Recovery After Surgery (ERAS) for gastrointestinal surgery, part 1: Pathophysiological considerations. Acta Anaesthesiol Scand 59: 1212-1231.
- Gustafsson UO, Scott MJ, Schwenk W, Demartines N, Roulin D, et al. (2013) Guidelines for perioperative care in elective colonic surgery: Enhanced Recovery After Surgery (ERAS) Society recommendations. World J Surg 37: 259-284.
- Blanchet MC, Gignoux B, Matussière Y, Vulliez A, Lanz T, et al. (2017) Experience with an Enhanced Recovery After Surgery (ERAS) program for bariatric surgery: Comparison of MGB and LSG in 374 patients. Obes Surg 27:1896-1900.
- Lewis SJ, Egger M, Sylvester PA, Thomas S (2001) Early enteral feeding versus "nil by mouth" after gastrointestinal surgery: Systematic review and meta-analysis of controlled trials. BMJ 323: 773-776.
- Henriksen MG, Jensen MB, Hansen HV, Jespersen TW, Hessov I (2002) Enforced mobilization, early oral feeding, and balanced analgesia improve convalescence after colorectal surgery. Nutrition 18: 147-152.
- Thorell A, MacCormick AD, Awad S, Reynolds N, Roulin D, et al. (2016) Guidelines for perioperative care in bariatric surgery: Enhanced recovery after surgery (ERAS) society recommendations. World J Surg 40: 2065-2083.
Citation: Zhang Q, Widjaja J, Yao L, Li C, Wang H, et al. (2018) Fast Track Surgery in Bariatric Surgery: Prospective Analysis of 80 Patients-A Randomized Controlled Trail . J Obes Weight Loss Ther 8: 369. DOI: 10.4172/2165-7904.1000369
Copyright: © 2018 Zhang Q, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 6295
- [From(publication date): 0-2018 - Dec 08, 2025]
- Breakdown by view type
- HTML page views: 5271
- PDF downloads: 1024