Case Report Open Access
Febrile Syndrome as a First Clinical Manifestation of Wilson Disease
Marisol Galvez-Martínez, Alfredo I. Servín-Caamaño, Eduardo Pérez-Torres and Fátima Higuera-de la Tijera*
Liver Clinic from Gastroenterology Department, “Hospital General of México, Dr. Eduardo Liceaga”, Mexico City, Mexico
- *Corresponding Author:
- Fátima Higuera-de la Tijera
Liver Clinic from Gastroenterology Department
“Hospital General of México, Dr. Eduardo Liceaga”
Dr. Balmis 148, 06726, Mexico City, Mexico
Tel: 015527892000
Fax: 1358
E-mail: fatimahiguera@yahoo.com.mx
Received date: March 07, 2015; Accepted date: April 23, 2015; Published date: April 30, 2015
Citation: Galvez-Martínez M, Servín-Caamaño AI, Pérez-Torres E, Higuera-de la Tijera F (2015) Febrile Syndrome as a First Clinical Manifestation of Wilson Disease. J Gastrointest Dig Syst 5:282. doi:10.4172/2161-069X.1000282
Copyright: © 2015 Martinez MG, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Wilson disease (WD) is a rare autosomal recessive genetic disorder associated with copper metabolism. ATP7B protein function is reduced or absent. The classical clinical presentation with positivity for Kayser-Fleischer rings, neurological and hepatic manifestations is not the rule. About half of the patients presenting liver disease may have atypical clinical manifestations and do not possess two of the three classical criteria.
Presentation of case: A 36 year-old male with atypical WD clinical presentation characterized by febrile syndrome and jaundice as the predominant manifestations of the disease.
Keywords
Wilson disease; Febrile syndrome; Atypical clinical presentation
Introduction
Wilson disease (WD) is an autosomal recessive genetic disorder associated with copper metabolism. Absent or reduced function of ATP7B protein leads to decreased hepatocellular excretion of copper into bile. There are more than 200 mutations of the responsible gene ATP7B. The possibility of present the disorder is 1 in 3000 individuals, with a genetic variation of 0.3% and 0.7% [1,2]. Clinical hepatic manifestations are present almost in 42% of the cases, they are non-specific and may be present in several forms, ranging from mild elevation of aminotransferases in asymptomatic individuals, or as acute liver failure, or in some cases as chronic liver disease. Clinical neurological and hematological manifestations can be present in 34% and 12% respectively [3].
The characteristic laboratories findings are low serum ceruloplasmin even though it could be normal in 5-15% of the patients, increased urinary copper excretion and increased in the hepatic content of copper. The treatment is based on chelating agents [1].
Clinical Case
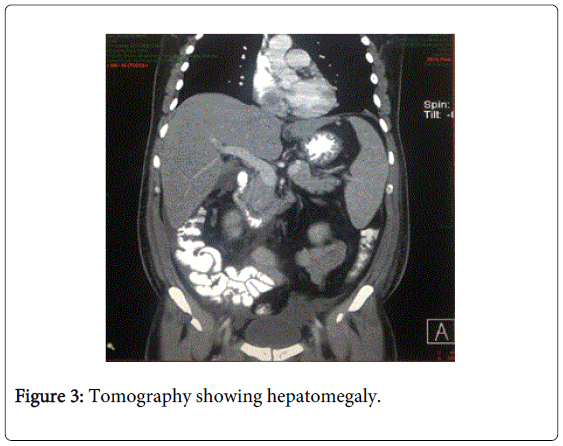
A 36 year-old male without significant medical history, previously known as a healthy subject, he had no history of alcohol or drugs consumption, neither herbal, medications nor any kind of supplements. His parents had type 2 diabetes, his brother was known as a healthy subject. Three months before his admission he started with gradual weight loss (15 Kg in three months), febrile syndrome with temperature between 38-39°C, diaphoresis, articular and muscular non-specific pain. Seven days before admission he noted jaundice and coluria. Remarkable at physical examination was the presence of non-tender hepatomegaly and jaundice, he had no ascites, neither clinical manifestations of psychiatric disorders nor clinical manifestations of hepatic encephalopathy, his body weight was 72 kg and his body mass index was 26 kg/m2.
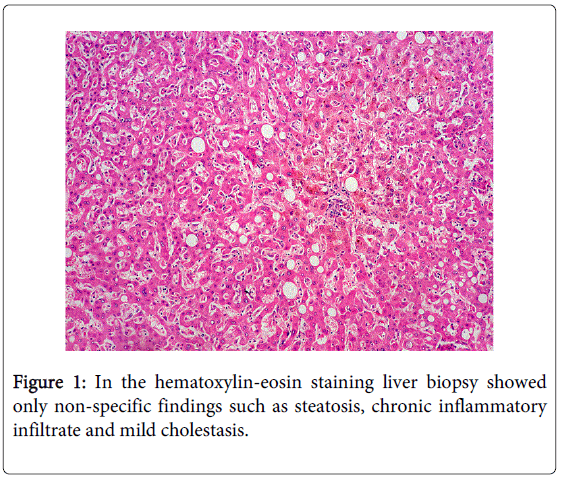
His most relevant laboratories were: Total bilirubin 11.4 mg/dL, direct bilirubin 6.1 mg/dL, indirect bilirubin 5.3 mg/dL, alkaline phosphatase 127 UI/L, gamma glutamyl transpeptidase 139 UI/L, aspartate aminotransferase 36 U/L, alanine aminotransferase 33 U/L, prothrombin time was normal (12.8 sec, 84.3%), hemoglobin 16.2 g/dL, leucocytes count 10.6 × 109/L, platelets count 111,000/mcL, immunoglobulin G 1537 mg/dL, immunoglobulin M 358 mg/dL, complement C3 125 mg/dL, complement C4 52 mg/dL. serum ceruloplasmin was normal (24 mg/dL), but copper urinary excretion was abnormal (359 mcg/24 hours). The Kayser-Fleischer rings were absent. Chest-X ray, blood, urine bone marrow and sputum cultures were negative. Viral infections, such as, hepatitis B, hepatitis C, acquired immunodeficiency syndrome, rubella virus, citomegalovirus, Epstein-Barr virus, other infections such as, leptospirosis in blood and urine, toxoplasmosis and tuberculosis were excluded. Immunologic markers (anti-nuclear, anti-mitochondrial, anti-smooth muscle, anti-liver kidney-1 antibodies) were negative (Figures 1-3).
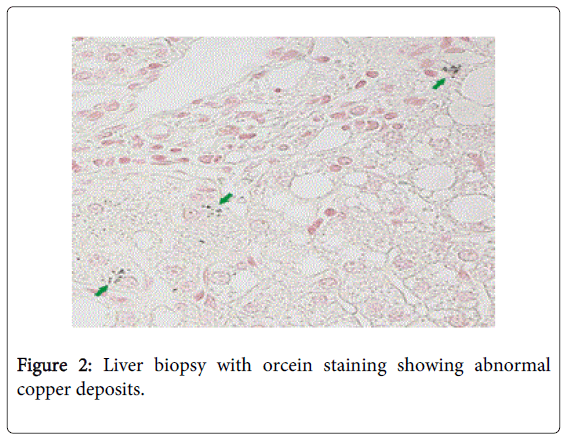
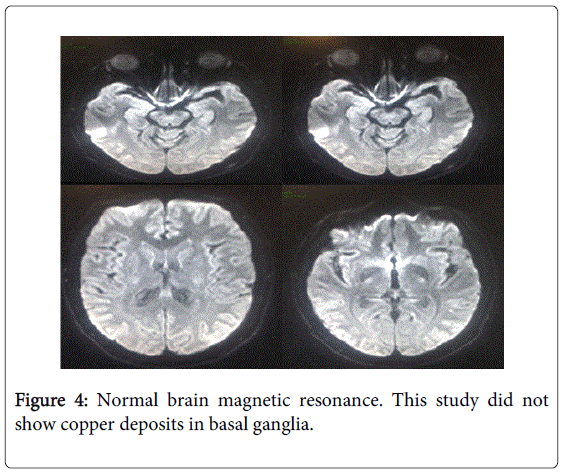
Tumor markers (alfafetoprotein, carcinoembrionic antigen, Ca 19-9, beta-2-microglobulin) were negative. Bone marrow aspirate was normal. The tomography showed hepatomegaly. Transferrin, ferritin, serum iron were normal. To exclude copper deposits in basal ganglia we performed a brain magnetic resonance, nevertheless this study was normal. In the hematoxylin-eosin staining liver biopsy showed only non-specific findings such as steatosis, chronic inflammatory infiltrate and mild cholestasis. Additionally liver biopsy showed positivity for orcein staining.
To confirm the diagnosis of Wilson disease, the quantification of copper in liver tissue was performed, resulting in 350 mcg/g dry weight. Our patient started treatment with D-penicillamine with gradual improvement of his signs and symptoms and resolution of jaundice and febrile syndrome, as well as normalization of biochemical tests (Figure 4).
Conclusions
WD is a rare hereditary disorder. Although in patients with the classical manifestations described by Kinnear Wilson in 1912 characterized by Kayser-Fleischer rings, neurological and hepatic symptoms the diagnosis seems to be easy [1,4], it is a challenge in those patients with atypical manifestations [5,6], such as our patient. The clinical manifestations are varied so the diagnostic is often difficult and delayed.
A low serum ceruloplasmin level (<20 mg/dL) is a criteria for the diagnosis of WD, nevertheless, since this is an acute phase reactant protein, 5-15% of the cases can have normal serum levels of ceruloplasmin [1], as our patient, in cases like this, an abnormal urinary copper excretion and the liver biopsy with orcein staining are tests which confirm the diagnosis [1,3].
References
- Roberts EA, Schilsky ML, American Association for Study of Liver Diseases (AASLD) (2008) Diagnosis and treatment of Wilson disease: an update.Hepatology 47: 2089-2111.
- Kim BE, Nevitt T, Thiele DJ (2008) Mechanisms for copper acquisition, distribution and regulation.Nat Chem Biol 4: 176-185.
- Kitzberger R, Madl C, Ferenci P (2005) Wilson disease.Metab Brain Dis 20: 295-302.
- Langner C, Denk H (2004) Wilson disease.Virchows Arch 445: 111-118.
- Wadera S, Magid MS, McOmber M, Carpentieri D, Miloh T (2011) Atypical presentation of Wilson disease.Semin Liver Dis 31: 319-326.
- Dabrowska E, Jablonska-Kaszewska I, Ozieblowski A, Falkiewicz B. (2001) Acute haemolytic syndrome and liver failure as the first manifestations of Wilson's disease.Med Sci Monit 7(1): 246-251.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 14406
- [From(publication date):
June-2015 - Aug 29, 2025] - Breakdown by view type
- HTML page views : 9814
- PDF downloads : 4592