Frequency of History of Hypertensive Disorders of Pregnancy in Patients Presenting with Acute Coronary Syndrome
Received: 25-Sep-2017 / Accepted Date: 17-Oct-2017 / Published Date: 23-Oct-2017 DOI: 10.4172/2376-127X.1000354
Abstract
Objective: The objective of the study is to determine frequency of history of hypertensive disorders of pregnancy (HDP) in patients presenting with acute coronary syndromes (ACS) and secondly to evaluate for the prevalence and concomitant association with hypertension, diabetes mellitus, chronic kidney disease (CKD) and cerebrovascular disease (stroke/TIA) in the above said patients. Methods: A cross sectional comparative study was conducted on 654 consecutive female patients presenting with ACS admitted to National Institute of Cardiovascular Diseases, Karachi between May to September 2013. A comprehensive questionnaire including details of obstetric history, history of HDP, ACS, cardiovascular risk factors and existing hypertension (HTN), diabetes mellitus and CKD was obtained. Patients with history of HDP (group 1) were compared with patients without history of HDP (group 2). Results: 654 female patients with ACS with mean age 55.5 ± 10.34 were included. 184 (28%) patients reported having history of HDP, i.e., history of gestational HTN, chronic HTN, pre-eclampsia/eclampsia was noted in 10.8%, 13.4% and 3.8%, respectively. Means of patient age, maternal age at 1st pregnancy and development of ACS (in years) after last pregnancy in patients with and without history of HDP were 53.8 ± 10.29 versus 56.8 ± 11.85 (p=0.003), 21.0 ± 5.89 versus 19.9 ± 5.39 (p=0.028) and 18.6 ± 8.0 versus 22.0 ± 10.0 (p=0.001), respectively. Existing hypertension in patients with history of HDP and without history of HDP were 88.0% versus 80.2% (p=0.018). Conclusion: History of HDP was present in almost one third of female patients presenting with ACS. Mean patient age, development of ACS (in years) after last pregnancy was less in patients with history of HDP. Existing hypertension was more frequent in this patient group.
Keywords: Hypertension; Pregnancy; Acute coronary syndrome
Introduction
Cardiovascular (CV) disease is the leading cause of death in both males and females’ globally [1]. A 50 year old woman has a lifetime risk of developing cardiovascular disease of about 39% and a lifetime mortality risk secondary to CV disease of approximately 26% [2-5].
HDP is a complex set of conditions that affects as many as 10% of all pregnant women. Besides causing high maternal and fetal morbidity, it also has long term adverse effects on women’s health and is associated with an increased risk for future cardiovascular disease, cerebrovascular disease, chronic kidney disease (CKD) and diabetes mellitus (DM) [6].
A spectrum of large western population based studies has suggested significant associations between HDP and risk of later development of CV diseases [6-8]. It was found that a range of different high blood- pressure conditions in pregnancy such as gestational hypertension and preeclampsia/eclampsia, predicted the onset of cardiovascular and cerebrovascular events, chronic kidney disease and diabetes over the subsequent decades, over an average of about 40 years. This was associated with triple the risk of fatal MI, almost twice the risk of CKD and 45-60% increased risks of ischemic heart disease, ischemic stroke and DM compared with women who remained normotensive during pregnancy.
The importance of a woman’s pregnancy history in the assessment of later CV risk was recognized following the 2011 update of the disease prevention guidelines for women by the American Heart Association [9]. Despite a significant association of HDP with the incidence of future CVD, such documentation is deficient in the heavily populated south Asian region and remains largely unrecognized.
The term ACS encompasses a variety of conditions ranging from Unstable Angina (UA), to ST-segment elevation MI and Non ST- segment elevation MI. ST-segment elevation MI as the name suggests presents with ST-segment elevation on the ECG and manifest as infarction of all the layers of the myocardium, whereas Non-ST segment elevated MI although devoid of ST-segment elevation on the ECG has severe ischemia and infarction of the sub-endocardium, Both of them present with elevated levels of cardiac enzyme i.e. Troponin and CK-MB which are the markers of MI and used for its diagnosis, unlike Unstable Angina (UA) in which there is no elevation of the cardiac enzymes and thus no MI despite the symptoms. The aim of this study was to determine the frequency of history of HDP admitted with the diagnosis of acute coronary syndrome (ACS) and secondly to determine association of existing current day hypertension, DM, CKD and Cerebrovascular disease in this group of patients [10,11].
Patients And Methods
A cross sectional study was performed on 654 consecutive female patients admitted to all medical units (including coronary care units) of the National Institute of cardiovascular diseases, Karachi, between May 2013 and September 2013 with the diagnosis of ACS. After approval of the National Institute of Cardiovascular Diseases Ethical Review Board, verbal consent was taken from each patient.
Inclusion criteria was patients of ≥ 18 years of age and first ever admission to the hospital with the diagnosis of ACS. Patients who had previous admission with ACS and current diagnosis other than ACS, mentally disabled and women who never conceived were excluded from the study.
Patients were questioned in detail as having HDP in any of their past pregnancies. Information was given by the patient herself or taken from close attendant available, in case of language barrier. The diagnosis of HDP was based on the guidelines of the National Heart, Lung and Blood Institute [12].
Participants were interviewed with the help of designed questionnaire which was sectioned into five different domains. Variables of demographic profile included name, age, marital status of the patient, number of children, ethnicity, years of education and blood pressure. Variables for menstrual history of patient were pre-menopause or menopause, age of menarche, age of menopause, cycle, number of pregnancies, last pregnancy, maternal age at time of last pregnancy and place of last delivery. History of pregnancy was also sectioned separately which include use of contraception, number of low birth weight babies, premature delivery, number of miscarriage, number of still birth, history of gestational hypertension, CV risk factors, chronic hypertension, pre-eclampsia, eclampsia, gestational diabetes, cerebrovascular disease and chronic kidney disease. Variables for present coronary risk factors included diabetes mellitus, hypertension, dyslipidemia, smoking and family history of ischemic heart diseases. The last section of questionnaire include the clinical presentation of patient, variables for which were unstable angina, non-ST elevation myocardial infarction (NSTEMI), ST elevation myocardial infarction (STEMI), raised biomarkers, blood sugar levels and serum creatinine levels.
Patients presenting with ACS who had history of HDP (group 1) were compared with patients with ACS without history of HDP (group 2) in terms of STEMI, NSTEMI, unstable angina, age, duration of last pregnancy and the current ACS and the association with the presence or absence of existing HTN, DM, CKD and history of stroke and TIA.
The data was entered and analyzed by the SPSS software version 19.0. Statistical comparison was performed by using student t-test for quantitative/continuous variables and Chi-square test for qualitative/ categorical variables. All p-value <0.05 were considered statistically significant.
Results
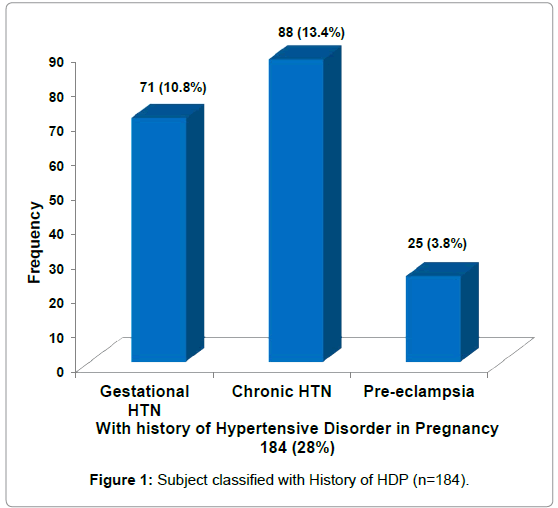
A total of 654 female patients with ACS were included. Mean ± S.D age was 55.5 ± 10.34 years. 395 (60.4%) patients had admission diagnosis of AMI and 259 (39.6%) had unstable angina. 440 patients (67%) did not have formal education. 392 (60%) babies were delivered at primary or tertiary care centers and 262 (40%) were delivered at home. 184 (28%) patients reported having positive history of HDP. Gestational HTN, chronic HTN and pre-eclampsia/eclampsia occurred in 10.8%, 13.4% and 3.8%, respectively in patients reported as having HDP.
Graphical representation of frequency of patients presented with the history of HDP is given in Figure 1. It was observed that most number of females presented with chronic hypertension followed by gestational hypertension and pre-eclampsia respectively (Figure 1).
Baseline characteristics of the two groups (Groups 1 and 2) are shown in Table 1. Mean age was significantly lower in group 1 than in group 2 (P-value<0.01). Mean maternal age at time of first pregnancy was significantly higher in group 1 (P<0.05). Conventional CV diseases risk factors, i.e., chronic HTN 162 (88.0%) were significantly high (p<0.05) in groups 1 as compared to group 2 (80.2%). No significant difference was noted as regards to the type of ACS between the two groups (Table 1).
| Variables | GROUP-1 (With HDP) (n=184) |
GROUP-2 (Without HDP) (n=470) |
P-value |
|---|---|---|---|
| Age (mean ± SD) | 53.8 ± 10.29 | 56.8 ± 11.85 | 0.003 |
| Obstetric and Gynaecological History | |||
| Premenopausal | 37 (20.1%) | 82 (17.4%) | 0.428 |
| Post-menopausal | 147 (79.9%) | 388 (82.6%) | |
| Maternal age at 1st pregnancy (Mean ± S.D) |
21.0 ± 5.89 | 19.9 ± 5.39 | 0.028 |
| Pregnancy to ACS in years (after last pregnancy) (Mean ± S.D) |
18.6 ± 8.0 | 22.0 ± 10.0 | 0.001 |
| Acute Coronary Syndrome (ACS) | |||
| ST-elevation MI | 44 (23.9%) | 113 (24.0%) | 0.722 |
| Non-ST elevation MI | 63 (34.3%) | 175 (37.2%) | |
| Unstable angina | 77 (41.8%) | 182 (38.7%) | |
| Coronary Risk Factors | |||
| Cigarette smoking | 53 (18.0%) | 88 (18.7%) | 0.815 |
| F/H of IHD | 74 (40.4%) | 173 (37.7%) | 0.545 |
| Outcome/existing | |||
| Hypertension | 162 (88.0%) | 377 (80.2%) | 0.018 |
| Diabetes mellitus | 83 (45.1%) | 230 (48.9%) | 0.366 |
| Cerebrovascular diseases (Stroke/TIA) | 23 (12.5%) | 41 (8.7%) | 0.143 |
| Chronic Kidney Disease (CKD) | 25 (16.6%) out of 151 |
42 (10.5%) out of 401 |
0.051 |
GROUP-1 (With HDP): With history of hypertensive disorder of pregnancy GROUP-2 (Without HDP): Without history of hypertensive disorder of pregnancy .
Table 1: Comparison between groups of patients with and without HDP.
Association of history of HDP with current HTN, DM, CKD and cerebrovascular disease is shown in Table 2. It shows that existing HTN and TIA/stroke occurred significantly more in patients reported having chronic HTN in their past pregnancies (p value<0.05). Similarly, prevalence of current CKD was significantly higher in patients who reported having gestational HTN in the past (p value<0.05). Multivariate analysis of qualitative and quantitative variables in our study showed that Age of patient (p=0.001) and history of hypertension (p=0.021) are good predictors of HDP. The details of multivariate analysis of quantitative and qualitative variables are given in Tables 3 and 4, respectively (Tables 2-4).
| With HDP (n=184) |
Without HDP (n=470) |
|||
|---|---|---|---|---|
| Present Outcome | Gestational HTN (n=71) |
Chronic HTN (n=88) |
Pre-eclampsia (n=25) |
|
| Current HTN | 59 (83.1%) | 83 (94.3%)*? | 20 (80.0%) | 377 (80.2%) |
| Diabetes mellitus | 35 (49.3%) | 35 (39.8%) | 13 (52.0%) | 230 (48.9%) |
| Cerebrovascular diseases (Stroke/TIA) | 6 (8.4%) | 14 (15.9%)* | 3 (12.0%) | 41 (8.7%) |
| Chronic Kidney Disease (CKD) | 12 (16.9%)* | 12 (13.6%) | 1 (4.0%) | 42 (8.9%) |
* Significantly high as compared to Without HDP (p<0.05)
? Significantly high as compared to Gestational HTN (p<0.05).
Table 2: Comparison of present outcome in patients with and without HDP.
| Coefficientsa | ||||||
|---|---|---|---|---|---|---|
| Model | Unstandardized Coefficients | Standardized Coefficients | T | Sig. | ||
| B | Std. Error | Beta | ||||
| Age in years | 0.006 | 0.002 | 0.152 | 3.460 | 0.001 | |
| Maternal age at 1st pregnancy | -0.006 | 0.003 | -0.076 | -1.920 | 0.055 | |
| Pregnancy to ACS after last pregnancy | -0.018 | 0.020 | -0.040 | -0.896 | 0.371 | |
a Dependent variable: Grouping HDP.
Table 3: Multivariate analysis of quantitative variables.
| Variables in the equation | |||||||
|---|---|---|---|---|---|---|---|
| B | S.E. | Wald | df | Sig. | Exp (B) | ||
| Hypertension | -0.599 | 0.259 | 5.361 | 1 | 0.021 | 0.549 | |
| Diabetes mellitus | 0.227 | 0.178 | 1.628 | 1 | 0.202 | 1.255 | |
| STEMI | 0.041 | 0.228 | 0.032 | 1 | 0.857 | 1.042 | |
| Non STEMI | 0.113 | 0.202 | 0.311 | 1 | 0.577 | 1.120 | |
| Unstable | -0.130 | 0.177 | 0.539 | 1 | 0.463 | 0.878 | |
| CVA_TIA | -0.344 | 0.281 | 1.496 | 1 | 0.221 | 0.709 | |
| CKD | -0.491 | 0.274 | 3.223 | 1 | 0.073 | 0.612 | |
Table 4: Multivariate analysis of qualitative variables.
Discussion
The results of our study support the association between HDP and the future risk of developing ACS [13,14]. HDP is a spectrum of diseases. The occurrence of its different categories in our study were gestational HTN, preeclampsia/eclampsia and chronic HTN in 10.8%, 3.8% and 13.4%, respectively which is consistent with the prevalence documented in western literature [5,6].
Cardiovascular disease (CVD) is the leading cause of death in both males and females globally [1,3]. The proportion of pregnancies complicated with hypertension is increasing [15].
Large, population based studies and systematic reviews of cohort studies have demonstrated that HDP (i.e., preeclampsia and gestational hypertension) are markers for future risk of cardiovascular disease [7,8,15-17]. Comparison between the two groups in our study on present day ACS suggested that women with history of preeclampsia advanced to developing ACS earlier in their life at 17.0 ± 7.3 years, making preeclampsia a dominant risk factor the occurrence of ACS. This is consistent with the results of other studies [12]. In a meta- analysis of observational studies, McDonald et.al found that women with a history of preeclampsia had a relative risk of 2.33 for developing CVD, although the prevalence of all forms of CVD in women aged 45 to 54 is around 2% [8,16-19].
Pre-eclampsia confers about 3.4 folds increment in risk of developing subsequent hypertension [8]. The results of our study however, showed that patients who already had chronic HTN during their pregnancies had significant association of developing subsequent HTN in contrast to a history of pre-eclampsia. In a cohort study by Mannisto et al., collected data from the large population of Northern Finland. Total 39 years of follow up demonstrated that any history of hypertension during pregnancy was associated with a higher risk of subsequent arterial hypertension [6]. Women with history of HDP tend to develop hypertension at a relatively younger age later on in their lives. Our study extends these findings by showing that women with HDP have a younger age of onset of HTN later in their life [8].
There is also an increased risk of developing type 2 DM in later life and pre-eclampsia can confer a 1.8 fold increased lifetime risk of DM [8,19]. Compared with women with normotensive pregnancies, women with a history of preeclampsia were much more likely to have developed DM at follow-up. This has been demonstrated by Carr et al. [20]. However, our study reported no significant association of history of HDP and future risk of DM.
We found significant association between HDP and CKD where 16.9% of the women with history of gestational HTN had incident CKD. Mannisto et al., in their study showed that new onset gestational hypertension was associated with significantly increased risk of kidney disease later in life with hazards risk of 1.91 [6]. Vikse et al. found that although the absolute risk of end stage renal disease in women who have had preeclampsia is low, the association was stronger if the preeclamptic pregnancy resulted in a low-birth-weight or preterm infant [21].
Pregnant women with HDP have an increased risk of subsequent stroke. Wilson and colleagues have demonstrated a 3.6-fold elevated risk of mortality from cerebrovascular disease in women with preeclampsia [14]. Preterm delivery and older maternal age increase the risk of subsequent stroke as has been seen in our study. Another followup study found that women with history of preeclampsia and preterm delivery had a 5.08-fold higher risk of cerebrovascular mortality [22,23]. In contrast chronic HTN during pregnancy was significantly associated with stroke in our study than preeclampsia as has been seen in one study [6].
In a meta-analysis of observational studies, McDonald et.al found that women with a history of preeclampsia had an RR of 2.33 of developing future CVD. But no significant association was noted with preeclampsia/eclampsia as regard the current outcomes like chronic HTN, CKD and T.I.A/stroke in our patients [8].
Increased awareness of the risk factors for CV disease with special emphasis on preventive strategies has been associated with a significant decline in mortality rates from CVD. Since 1980, with such measures the mortality rate from CVD has fallen by almost 44% in the United States [24]. In the present study we found significant association of history of HDP to future occurrence of ACS, chronic HTN, CKD and T.I.A./stroke. In this context, a crucial point would be to identify, target, counsel and manage these high-risk women for early detection and potential intervention which may translate into reducing a proportion of the morbidity and mortality from such diseases [25].
Limitation
Limitations of our study include the fact that the design of our designated questionnaire required patient recall of distant past pregnancy events and the authenticity of obstetric history given by patient could not be verified due to the low literacy level of our sample population and lack of access to patient’s obstetric medical records, in the future we would recommend that all information should be directly accessed from the patient’s medical records rather than relying on the recall of the patient which could be subject to bias. Also, almost 40% of deliveries took place at homes without proper antenatal care facilities, consequently there may have been a possibility of under or over reporting of HDP in these patients. The study does not address the possible contribution of raised body mass index to the subsequent development of ACS as documented in large cohort studies done in the West. Being an observational study, the possible role of uncontrolled confounding factors may also have been a limitation.
It has been suggested that there is a gap in knowledge related to cardiovascular disease prevention and disease management among women and obstetricians [26]. Education of patients and health care providers about this increased CVD risk is a logical initial step. Reducing modifiable risk factors for CVD such as improving the diet and lifestyle, regular physical exercise and smoking cessation is prudent for this group of at risk women with a history of HDP. Early referral of these patients with HDP by obstetricians to cardiologists would also be important for early screening, treatment and follow-up as they would play an important role in primary prevention of cardiovascular disease. Women should also be educated regarding the hazards of domiciliary delivery. In conclusion, cardiologists evaluating a middle aged woman’s risk for CVD should include history of HDP as part of the comprehensive clinical evaluation and should not restrict themselves on inquiring about the presence or absence of traditional CVD risk factors.
Conclusion
HDP seem to be associated in later life with diseases related to hypertension. Any history of hypertension during pregnancy merits comprehensive cardiovascular risk assessment during later life. Future large scale studies on this topic, especially in the heavily populated south Asian region are warranted and will provide further insight into the important link of HDP and future CVD risk. Medical record keeping and data bases should be organized in the developing countries like Pakistan for pregnancy outcomes to provide basis for future research, including presence and type of HDP.
Acknowledgement
- Murray CJL, Lopez AD (1997) Alternative projections of mortality and disability by cause 1990-2020: Global burden of disease study. Lancet 349: 1498-1504.
- Intapad S, Alexander BT (2013) Future cardiovascular risk. Circulation 127: 668-669.
- D'Agostino RB, Vasan RS, Pencina MJ, Wolf PA, Cobain M, et al. (2008) General cardiovascular risk profile for use in primary care: The Framingham heart study. Circulation 117: 743-753.
- Berry JD, Dyer A, Cai X, Garside DB, Ning H, et al. (2012) Lifetime risks of cardiovascular disease. N Engl J Med 366: 321-329.
- Ananth CV, Cleary KL (2013) Pre-eclampsia and cardiovascular disease: More questions than answers? BJOG: Int J Obstet Gynaecol 120: 920-923.
- Männistö T, Mendola P, Vääräsmäki M, Järvelin MR, Hartikainen AL, et al. (2013) Elevated blood pressure in pregnancy and subsequent chronic disease risk. Circulation 127: 681-690.
- Valdiviezo C, Garovic VD, Ouyang P (2012) Preeclampsia and hypertensive disease in pregnancy: Their contributions to cardiovascular risk. Clin cardiol 35: 160-165.
- McDonald SD, Malinowski A, Zhou Q, Yusuf S, Devereaux PJ (2008) Cardiovascular sequelae of preeclampsia/eclampsia: A systematic review and meta-analyses. Am Heart J 156: 918-930.
- Mosca L, Benjamin EJ, Berra K, Bezanson JL, Dolor RJ, et al. (2011) Effectiveness-based guidelines for the prevention of cardiovascular disease in women-2011 update: A guideline from the American heart association. Circulation 123: 1243-1262.
- Kumar A, Cannon CP (2009) Acute coronary syndromes: Diagnosis and management, part I. Mayo Clinic Proceedings, Elsevier.
- Ortega-Gil J, Parez-Cardona JM (2008) Unstable angina and non ST elevation acute coronary syndromes. Puerto Rico Health Sci J.
- National High Blood Pressure Education Program (NHBPEP) (2000) Report of the national high blood pressure education program working group on high blood pressure in pregnancy. Am J Obstet Gynecol 183: S1-S22.
- Wikström AK, Haglund B, Olovsson M, Lindeberg SN (2005) The risk of maternal ischaemic heart disease after gestational hypertensive disease. BJOG: Int J Obstet Gynaecol 112: 1486-1491.
- Lin YS, Tang CH, Yang CY, Wu LS, Hung ST, et al. (2011) Effect of pre-eclampsia-eclampsia on major cardiovascular events among peripartum women in Taiwan. Am J cardiol 107: 325-330.
- Wallis AB, Saftlas AF, Hsia J, Atrash HK (2008) Secular trends in the rates of preeclampsia, eclampsia and gestational hypertension, United States, 1987-2004. Am J Hypertens 21: 521-526.
- Magnussen EB, Vatten LJ, Smith GD, Romundstad PR (2009) Hypertensive disorders in pregnancy and subsequently measured cardiovascular risk factors. Obstet Gynecol 114: 961-970.
- Bellamy L, Casas JP, Hingorani AD, Williams DJ (2007) Pre-eclampsia and risk of cardiovascular disease and cancer in later life: Systematic review and meta-analysis. BMJ 335: 974.
- Wilson BJ, Watson MS, Prescott GJ, Sunderland S, Campbell DM, et al. (2003) Hypertensive diseases of pregnancy and risk of hypertension and stroke in later life: Results from cohort study. BMJ 326: 845.
- Lykke JA, Langhoff-Roos J, Sibai BM, Funai EF, Triche EW, et al. (2009) Hypertensive pregnancy disorders and subsequent cardiovascular morbidity and type 2 diabetes mellitus in the mother. Hypertension 53: 944-951.
- Carr DB, Newton KM, Utzschneider KM, Tong J, Gerchman F, et al. (2009) Preeclampsia and risk of developing subsequent diabetes. Hypertens Pregnancy 28: 435-447.
- Vikse BE, Irgens LM, Leivestad T, Skjerven R, Iversen BM (2008) Preeclampsia and the risk of end-stage renal disease. N Engl J Med 359: 800-809.
- Wang IK, Chang SN, Liao CC, Liang CC, Chang CT, et al. (2011) Hypertensive disorders in pregnancy and preterm delivery and subsequent stroke in Asian women: A retrospective cohort study. Stroke 42: 716-721.
- Irgens HU, Roberts JM, Reiseter L, Irgens LM, Lie RT, et al. (2001) Long term mortality of mothers and fathers after pre-eclampsia: Population based cohort study. Pre-eclampsia and cardiovascular disease later in life: Who is at risk? BMJ 323: 1213-1217.
- Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, et al. (2007) Explaining the decrease in US deaths from coronary disease, 1980-2000. N Engl J Med 356: 2388-2398.
- Sattar N, Greer IA (2002) Pregnancy complications and maternal cardiovascular risk: Opportunities for intervention and screening? BMJ 325: 157.
- Pilote L, Dasgupta K, Guru V, Humphries KH, McGrath J, et al. (2007) A comprehensive view of sex-specific issues related to cardiovascular disease. Can Med Assoc J 176: S1-S44.
Citation: Habib S, Qadir F, Bareeqa SB, Ziauddeen, Tariq QD, et al. (2017) Frequency of History of Hypertensive Disorders of Pregnancy in Patients Presenting with Acute Coronary Syndrome. J Preg Child Health 4: 354. DOI: 10.4172/2376-127X.1000354
Copyright: © 2017 Habib S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5430
- [From(publication date): 0-2017 - Dec 06, 2025]
- Breakdown by view type
- HTML page views: 4497
- PDF downloads: 933