Case Report Open Access
Gastrojejunal Stenosis of Gastric Bypass in Laparoscopic Bariatric Surgery: Report of a Case
Julian Andres Tamayo Serrato*, Isabel Mateo Gavira, Francisco Javier Vilchez Lopez, Laura Larran Escandón, Manual Aguilar Diosdado, Maria Angeles Mayo Ossorio and Jose Pacheco GarcíaDepartment of Endocrinology & Nutrition, Puerta del Mar University Hospital, Cadiz, Spain
- *Corresponding Author:
- Isabel Mateo Gavira, MD, PhD
Department of Endocrinology & Nutrition
Puerta del Mar University Hospital, Cadiz, Spain
Tel: +34956003095
Fax: +34 956004600
E-mail: isamateogavira@gmail.com
Received date: March 25, 2015; Accepted date: March 30, 2015; Published date: April 10, 2015
Citation: Serrato JAT, Gavira IM, Lopez FJV, Escandón LL, Diosdado MA, et al. (2015) Gastrojejunal Stenosis of Gastric Bypass in Laparoscopic Bariatric Surgery: Report of a Case. J Gastrointest Dig Syst 5:275. doi:10.4172/2161-069X.1000275
Copyright: © 2015 Serrato JAT, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Obesity is a chronic multifactorial disease, which results from the interaction between the genotype and the environment. It has become a public health problem across the world, with significant physical and psychological complications that contribute to the deterioration of the quality and expectancy of life. Gastric bypass is the most effective treatment option for the management of morbid obesity. Surgical treatment of obesity could reduce excess body weight by 50%-70% when compared to behavioral and pharmacological therapies. However, Gastrojejunal stricture (GYS) is the most common complication after laparoscopic gastric bypass, being that the pathophysiological mechanism involved not well understood. Presentation of Case: A 37-year-old man presented with progressive oral intolerance, incoercible vomiting, and high weight lost 2 months after Roux-en-Y gastric bypass (RYGBP). A severe stenosis was detected, pneumatic dilation made, and enteral nutrition required for several weeks.
Abstract
Obesity is a chronic multifactorial disease, which results from the interaction between the genotype and the environment. It has become a public health problem across the world, with significant physical and psychological complications that contribute to the deterioration of the quality and expectancy of life. Gastric bypass is the most effective treatment option for the management of morbid obesity. Surgical treatment of obesity could reduce excess body weight by 50%-70% when compared to behavioral and pharmacological therapies. However, Gastrojejunal stricture (GYS) is the most common complication after laparoscopic gastric bypass, being that the pathophysiological mechanism involved not well understood. Presentation of Case: A 37-year-old man presented with progressive oral intolerance, incoercible vomiting, and high weight lost 2 months after Roux-en-Y gastric bypass (RYGBP). A severe stenosis was detected, pneumatic dilation made, and enteral nutrition required for several weeks.
Keywords
Bariatric surgery; Gastrojejunal structure; Ballon dilation; Morbid obesity; Esophagogastric barium transit
Introduction
Bariatric surgery has shown to be an effective therapeutic modality for morbid obesity (BMI ≥ 40 kg/m2). In Spain, as in other developed countries, the number of interventions has exponentially increased in recent years due to the progressive increment of obesity prevalence, failure of medical treatment and improvement in laparoscopic techniques. RYGBP, one of the most common surgical procedures, involves a small gastric pouch and a gastrojejunal anastomosis [1]. Laparoscopic approach offers clear advantages compared to open surgery, such as shorter hospital stay, shorter period of recovery, lower incidence of wound infections and less blood loss during surgery [2].
Case Report
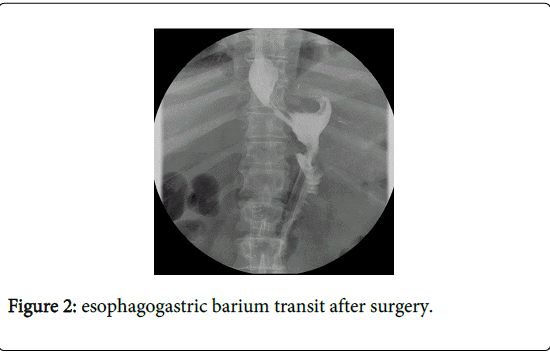
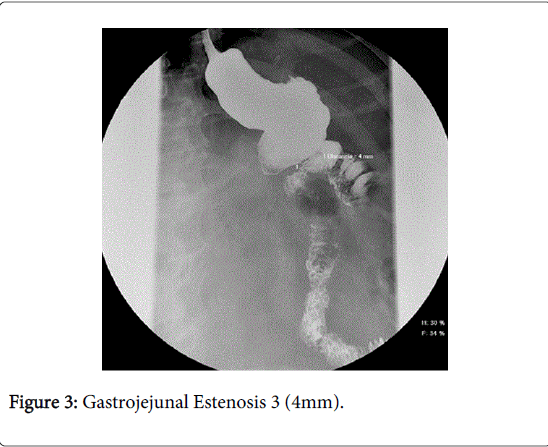
A 37-year-old man presented with 1 month of intermitent epigastric pain and abdominal bloating, progressive nausea and incoercible vomiting. He had a previous history of Roux-in-Y Gastric bypass 2 months before due to morbid obesity with a maximum weight of 140 kg (BMI 45 kg/m2) and gastroesophageal reflux disease and hypertension as comorbidities. Post-operatively, barium transit had not shown anastomotic leakage (Figures 1 and 2), and he started with initial liquid diet and semi-solid diet thereafter. He later developed progressive oral intolerance, accelerating his weight loss to 92.8 kg (BMI 28 kg/m2). He had no vitamin or hydroelectolityc disturbance, and the abdominal X-Ray was normal. An endoscopy was carried out, which showed a severe stenosis (<4 mm) with esophagogastric dilation and delayed gastric emptying (Figure 3). We performed a pneumatic dilation (3 sessions) every 3 days with progressive balloon diameter (6-8-10 mm). The long-term outcome was excellent without complications or failure. He started enteral nutrition, and a liquid diet was kept for several weeks.
In the two-subsequent year evaluations, comorbidities have disappeared. Patient did not any longer require other treatments for hypertension or hypertriglyceridemia. Patient reached a weight loss of 53.4 kg due to a procedure with a constant BMI of 26.8 kg/m 2 and a weight of 86.6 kg.
The mean percentage of excess wieght loss (%EWL) was 78.83% with a GOOD result on BAROS. No other complication was shown during the following-up, and oral diet was re-started in patient, who has not required any other endoscopic dilatation.
Discussion
Gastrojejunal stricture is the most common late complication following laparoscopic gastric bypass. However, the pathophysiological mechanisms involved in the formation of stenosis are not well understood. Although, situations such as ischemia of the suture, stomal ulcer, reflux or retraction of the scar may contribute to its appearance. Nguyen et al. have demonstrated that this complication is more common after laparoscopyc RYGBP (11.4%) than after open RYGBP (2.6%) [3,4]. In our series 27.2% of the patients had presented late complications (>1 month): eventration (12.2%), severe malnutrition (6.8%) and (4%) of GYS.
The clinical presentation of these lesions after the first post-operative month is due to the fact that during the first 4-6 weeks the patients only receive a liquid diet followed by semi-solid foods thereafter.
Symptoms include epigastric pain and solid-undigested postprandial vomiting. Vomiting can cause malnutrition with vitamin deficiency, especially thiamine deficiency, which can occur within weeks and develop neurological problems such as vision and gait disturbance, severe peripheral neuropathy, Wernicke encephalopathy, or even death. Prolonged gastric reservoir obstruction may precipitate abnormal gastroesophageal reflux and esophagitis.
The performance of an esophagogastric barium transit (EBT) is a diagnostic technique whereas endoscopy is both diagnostic and therapeutic. EBT is useful as a first screening study when compatible symptoms occur, although if there is a high suspicion of stenosis, an endoscopy as a diagnostic/therapeutic method will always be necessary.
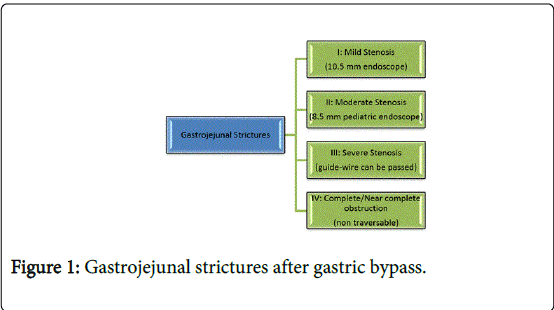
Gastrojejunal strictures can be classified based on time of onset, mechanism of formation, and endoscopic aspect (anastomotic diameter) into four groups [5] (Figure 1).
The two main treatment alternatives for stomal stricture are: endoscopic dilation (balloon or bougienage), and surgical revision (open or laparoscopic). Both techniques of dilation, through-the-scope (TTS) balloon dilators and bougienage dilators are considered safe and effective. TTS balloon dilators provide gradual expansion and radial dilation, thus preventing excessive pain and minimizing the appearance of perforation. The balloons could be inflated with water, saline solution, or water-soluble contrast medium. The need for reconstructive surgery of a GYS surgery is extremely rare (0.4%) [6] and is usually reserved for patients who are unable to achieve optimal dilation after four consecutive sessions, with a significant increase in morbidity. In our patient, we made three dilations until an adequate stoma was reached during the sharp stage. Patient did not require subsequent procedures or surgery.
The endpoint for GYS dilation is yet to be established. While the immediate goal is to provide symptomatic relief, a narrow stomal outlet must be maintained so that long-term weight loss is achieved. Lee et al. [2] recommend dilation that obtains a stoma > 11 mm in diameter, but not excessively large (above 15-18 mm), in order to maintain the restrictive integrity of the bypass surgery, ensuring continued weight loss and minimizing the risk of complications such as dumping [7].
The literature commonly indicates that the average number of dilations needed is between one and two. A systematic review by Campos et al. [8] shows 1,298 dilations in 760 patients, with an average of 1.7 dilations per patient. This was consistent with the data reported by Caro et al. (1.8 dilations per patients) [7].
The success rate ranges from 77%-100%, and for the majority of patients it is achieved in the first or second session. Complications are rare. Cases of perforation are generally managed conservatively without surgical revision.
The Bariatric Analysis and Reporting Outcome System (BAROS) evaluates the results of obesity treatments by analyzing three domains: weight loss, changes in co-morbidities, and quality of life. Up to 3 points are allowed for each, and points are deducted for complications and reoperations. The final score classifies the results in five outcome groups, providing an objective definition of success or failure. BAROS is very useful for evaluating and reporting the results of obesity treatments. It can be used to measure the outcomes of one or more operations and to compare the results among different surgeons, regardless of their location [9]. The system has been used in many countries since the late 1990s.
Bariactric surgery is considered an alternative to medical treatment, and it is more effective in patients with morbid obesity, in particular in related co-morbidities, according to literature. Bariatric surgery also improves the patients’ quality of life.
Conclusion
In morbidly obese patients (BMI ≥35), bariatric surgery is considered the most effective durable weight-loss therapy. Laparoscopic Roux-en-Y gastric bypass is associated with risks of nutritional deficiencies and gastrojejunal stricture and should be suspected when patients show signs of dysphagia, nausea and vomiting. The recommended treatment is dilation of stomal stenosis through balloon dilators, with an average of 2 sessions. Endoscopic dilation of GJS is an effective treatment with minimal risk. Surgical laparoscopic treatment should be considered when balloon dilation does not achieve an adequate stoma (12-15 mm) after four sessions, with a higher prevalence of complications.
References
- Mateo Gavira I, Vílchez López FJ, Cayón Blanco M3, García Valero A2, Escobar Jiménez L2, et al. (2014) [Effect of gastric bypass on the cardiovascular risk and quality of life in morbid obese patients]. Nutr Hosp 29: 508-512.
- Lee JK, Van Dam J, Morton JM, Curet M, Banerjee S (2009) Endoscopy is accurate, safe, and effective in the assessment and management of complications following gastric bypass surgery. Am J Gastroenterol 104: 575-582.
- Nguyen NT, Goldman C, Rosenquist CJ, Arango A, Cole CJ, et al. (2001) Laparoscopic versus open gastric bypass: a randomized study of outcomes, quality of life, and costs. Ann Surg 234: 279-289.
- Nguyen NT, Stevens CM, Wolfe BM (2003) Incidence and outcome of anastomotic stricture after laparoscopic gastric bypass. J Gastrointest Surg 7: 997-1003.
- Goitein D, Papasavas PK, Gagné D, Ahmad S, Caushaj PF (2005) Gastrojejunal strictures following laparoscopic Roux-en-Y gastric bypass for morbid obesity. Surg Endosc 19: 628-632.
- Livingston EH, Huerta S, Arthur D, Lee S, De Shields S, et al. (2002) Male gender is a predictor of morbidity and age a predictor of mortality for patients undergoing gastric bypass surgery. Ann Surg 236: 576-582.
- Caro L, Sánchez C, Rodríguez P, Bosch J (2008) Endoscopic balloon dilation of anastomotic strictures occurring after laparoscopic gastric bypass for morbid obesity. Dig Dis 26: 314-317.
- Campos JM, Mello FS, Ferraz AA, Brito JN, Nassif PA, et al. (2012) Endoscopic dilation of gastrojejunal anastomosis after gastric bypass. Arq Bras Cir Dig 25: 283-289.
- Oria HE, Moorehead MK (2009) Updated Bariatric Analysis and Reporting Outcome System (BAROS). Surg Obes Relat Dis 5: 60-66.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 15345
- [From(publication date):
April-2015 - Aug 03, 2025] - Breakdown by view type
- HTML page views : 10766
- PDF downloads : 4579