Case Report Open Access
Giant Choledochal Cysts in a 2 Year Old Child
Aida D*, Rabia Ben A, Malak B, Habib B, Youssef H, Youssef G and Nejib K
Department of Pediatric Surgery, Hopital Habib Thameur, Ali ebn Ayed montfleury, Tunisia
- *Corresponding Author:
- Aida D
Department of Pediatric surgery
Hopital Habib Thameur
Ali ebn Ayed montfleury, Tunisia
Tel: 0021697857899
E-mail: aidadaib@yahoo.fr
Received Date: October 23, 2016; Accepted Date: November 16, 2016; Published Date: November 23, 2016
Citation: Aida D, Rabia Ben A, Malak B, Habib B, Youssef H, et al. (2016) Giant Choledochal Cysts in a 2 Year Old Child. Neonat Pediatr Med 2: 116. doi: 10.4172/2572-4983.1000116
Copyright: © 2016 Aida D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Neonatal and Pediatric Medicine
Abstract
The cystic dilatation of the common bile duct is a rare pathology. It is the second surgical case of cholestasis icterus in infants after biliary duct atresia. It still poses problems of differential diagnosis and treatment. A girl aged 2 years has been admitted in our department for exploration of an abdominal distension. The physical examination has shown the presence of a large mass at the level of the hypochondria and the right flank arriving to the umbilicus associated with a discrete icterus without other signs. Laboratory tests have been without anomalies except a hyperbiluribinémie. Abdominal ultrasound revealed a hepatic cyst measuring 11.6 in the segment 4 and 5 of the liver. A computerized tomography concluded to a large hepatic cyst with an important part under the liver arriving to the pelvis. Magnetic resonance cholangio-pancreatography confirmed the diagnosis of a large cystic dilatation of the common bile duct type 4 of Todani. At laparotomy, a giant cystic dilatation of the common bile duct going from the liver extending into the right abdominal part. She had had a total excision of the cystic dilatation of the common bile duct, carrying away the cystic duct and the gallbladder, with a bilio-digestive bypass installing a jejunal loop in Y.
Keywords
Cystic dilatation of the bile duct; Child; Congenital
Introduction
The congenital cystic dilatation of the common bile duct is a rare malformation of the bile ducts [1,2]. It is more widespread in Far East, in Asian countries [3], with a clear female predominance [4]. An anomaly of the junction of biliopancreatic channels generating a reflux of the pancreatic liquid into the bile ducts seems to be the main etiological factor that predisposes the development of the congenital cystic dilatation of the common bile duct [5].
The diagnosis is frequently performed in childhood. However, the variability of clinical symptomology and the latency of the affection can explain its late discovery in some cases [6]. We describe a rare case of giant choledochal cysts in a 2 year old girl.
Case Report
A 2 year old girl presented for jaundice and abdominal mass appeared 1 month earlier without fever or abdominal pain.
The physical examination has shown the presence of a large mass at the level of the hypochondria and the right flank arriving to the umbilicus associated with a discrete icterus without other signs. Laboratory tests have been without anomalies except a hyperbiluribinemie conjugated.
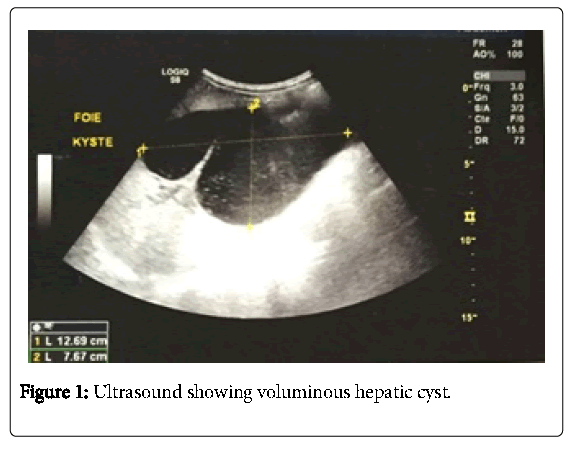
An abdominal ultrasound showed a large cystic mass measuring 11.6 centimeters in the 4 and 5 segments of the liver with dilation of the intra-liver bile duct (Figure 1).
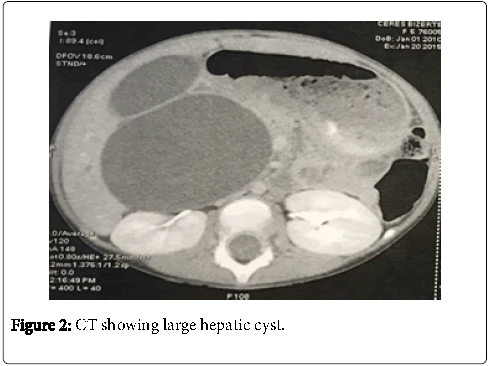
We completed by a computerized tomography, to clarify the diagnosis, which had concluded to a large hepatic cyst measuring 14 centimeters with an important part under the liver arriving to the pelvis(Figure 2).
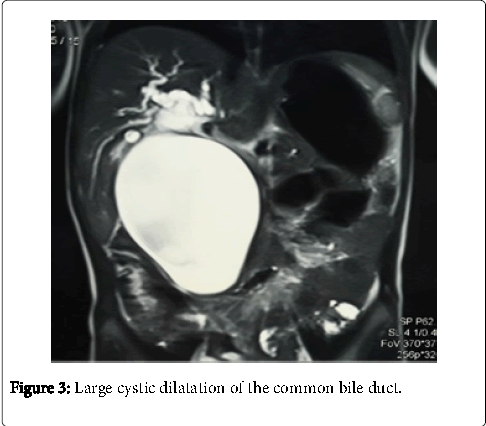
The cyst exerts a mass effect on the port’s bifurcation, the duodenum, the spléno-mésaraique trunk, the superior mesenteric artery and the head of the pancreas. The diagnosis still blurry. Magnetic resonance cholangiopancreatography confirmed the diagnosis of a large cystic dilatation of the common bile duct with a dilation of the right and the left hepatic duct type 4 of Todani (Figure 3).
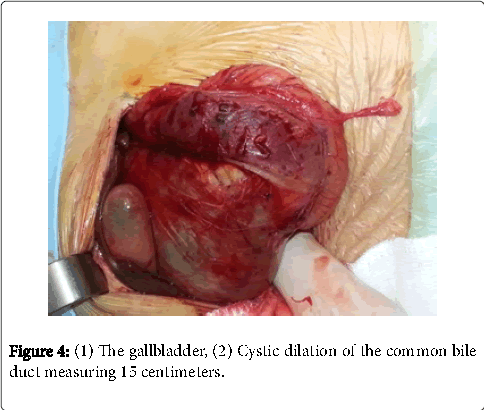
She has been operated. A laparotomy under rib right cage has been carried out. Surgical exploration has confirmed the presence of a Cystic dilation of the common bile duct measuring 15 centimeters (Figure 4).
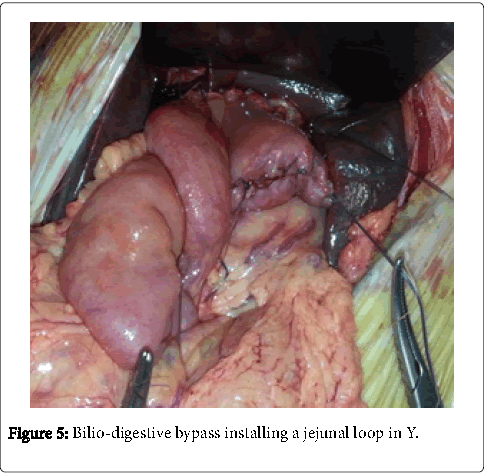
The intervention consisted in a total excision of the cystic dilatation of the common bile duct, carrying away the cystic duct and the gallbladder and confection of a bilio-digestive bypass installing a jejunal loop in Y (Figure 5).
We realized a liver biopsy and drainage of the under liver region. The evolution in postoperative was favorable on the clinical and biological side. We noted a disappearance of jaundice and regression of the cholestasis.
Discussion
The detection of a congenital cystic dilation of the common bile duct can be carried out at any age [5]. Some cysts may currently be diagnosed before birth, between the 15th and the 37th gestation week due to the better understanding of this malformation and to the ultrasound advancements [7,8]. However, the diagnosis is generally carried out before the age of 1 year in 20-30% of the cases, between 1 and 10 years in 50% and up to 10 years old in 10-20% of the cases [6]. The female prevalence is typically observed with an approximate ratio of 7-8 girls for a boy [4].
In a clinical viewpoint, the symptomatology is nonspecific. In fact, jaundice is a frequently observed symptom in infants [9]. In children, the abdominal pains are usually indicative of the anomaly [10] and are often considered to be secondary to the pancreatitis episodes [11]. The clinical triad consisting in jaundice, an abdominal mass and associated pain can be considered to be rare with a frequency of 15-25% of cases [4]. In our case, the girl presented a giant abdominal mass arriving to the pelvis.
There is no biological diagnostic value. However, biological analysis allows primarily determining the cholestasis degree, appreciating the impact of the malformation on liver function and detecting associated pancreatitis [4].
The diagnosis of cystic dilatation of the bile ducts is heavily based on imaging [12]. Abdominal ultrasound is the first examination required in the situation of a suspicion of a cystic dilatation of the common bile duct. It is easy to carry out the diagnosis by showing a sub-hepatic cystic image linked with the bile duct, with a sensitivity approaching 100% [12]. It can be associated with a dilatation of the intrahepatic bile duct [13].
Computed tomography provides little additional information in comparison with ultrasound. Its interest lies in the ability to explore the relationships between the cyst and the nearby organs in the case of a gaseous digestive distension inconvenient for the ultrasound examination [13,14].
The magnetic resonance cholangiopancreatography has several advantages. Indeed, it is a non-intrusive exploration technique, not only for intra and extra-hepatic biliary ducts, but also for pancreatic ducts. In addition, it requires less than five minutes for acquisition. On one hand, it helps to confirm the diagnosis. On the other hand, it allows having the mapping of all bile ducts which can be examined in many planes. The surgeon can then prepare properly his gesture. The technique has a sensitivity exceeding 95%, but it has limitations like the examination of fine bile ducts which remains difficult especially in infants [3,14,15]. In our patient, the voluminous mass neither ultrasound neither tomography evocated diagnosis, only the magnetic resonance cholangiography confirmed related the mass to a congenital cystic dilation of the common bile.
Many morphological classifications have been proposed in clinical practice [11]. The classification of Todani, proposed in 1977, is currently used by most authors. It distinguishes between five types according to the dilatation aspect and topography. The type I represents the most common form [13,16,17].
The spontaneous course of congenital cystic dilation of the common bile duct leads more or less early to mechanical and septic complications [5]. We may be dealing with a severe pancreatitis and with cholangitis which are rare complications, often associated with biliary and pancreatic lithiasises. Angiocholitis may require an urgent external drainage if the antibiotherapy is unsuccessful [5,9,18]. The perforation associated with a biliary peritonitis is a rare complication, but it is not exceptional in infants. The inflammation and the distention may result in the cracking of the bile duct associated with a peritonitis which can be quite serious [19,20].
The surgical treatment, whether by laparotomy or by laparoscopy, aims to restore the normal bile flow and to limit the risk of degeneration. Therefore, the total resection of the cystic wall which may degenerate should be performed with a hepaticojejunal anastomosis on a Y loop of 40 cm long [5]. The dilated bile duct is released in the top until the convergence and in the bottom until the end of the cyst wall with an attention to avoid leaving a bottom coquetier which can be the site of a subsequent degeneration. However, the dissection of the entire cyst should not be systematically performed in the pancreatic tissue because of the important risk of injuring the pancreatic duct [5]. The Wirsung duct can in fact be very close to the cystic dilatation and cannot be seen in intra-pancreatic. The hepaticoduodenostomy using an interposed jejunal loop is another repair technique which allows avoiding the occurrence of secondary peptic complications [5]. Chinese authors developed a spur valve creating a non-return effect, to mitigate the risk of the reflux of the duodenal content [5]. The consequences of the intervention are usually simple. The long-term monitoring reveals no specific complications. But the evolution can be characterized by some complications which depend on the surgical technique and the care period [5]. Indeed, postoperative complications like the stenosis of hepaticojejunal anastomosis and the lithiasis of the intrahepatic bile ducts can be encountered. The mortality rate is currently close to zero due to a better understanding of the disease, to the early prenatal diagnosis which is becoming more common, to a better knowledge of the evolutionary complications and to an improved mastery of the surgical technique [21].
Conclusion
The congenital cystic dilatation of the biliary tract is a rare disease. Its symptomatology is not specific and varies according the age. The diagnosis of such malformation is based on ultrasound and magnetic resonance cholangiopancreatography. The early diagnosis which is more and more achievable in utero would prevent the development of the secondary biliary cirrhosis and the malignant degeneration. Our case is the first in the literature with a very giant mass.
Conflict of Interest
None
References
- Davenport M, Betalli P, D’Antiga L (2003) The spectrum of Jaundice in Infancy. Journal of pediatric Surgery 38: 1471-1479.
- Casaccia G, Bilancioni E, Trucchi A (2002) Cystic anomalies of biliary tree in the fetus: is it possible to make a more specific prenatal diagnosis? Journal of pediatric surgery 37: 1191-1194.
- Anglade E, Aubé C, Lebigot J.Bilan (2000) Pré thérapeutique d’une dilatation congénitale de la voie biliaire principale par cholangio-pancréatographie-IRM. Arch Péditr 7: 49-53.
- Wong-Hoi S, Chung HY, Lan LCL, Wong KKY, Saing H et.al, (2009) Management of choledochal cyst: 30 years of experience and results in a single center. Journal of Pediatric Surgery 44: 2307-2311.
- Branchereau S, Valayer J (2002) Malformations kystiques de la voie biliaire chez l’enfant : dilatation congénitale de la voie biliaire principale. Traitement chirurgical. Encycl. Méd. Chir. Techniques chirurgicales-Appareil digestif. 976-986.
- Erlinger S (2000) Dilatation kystiques des voies biliaires. La revue du praticien 50: 2136-2141.
- Shroeder D, Smith L, Prain H (1989) Antenatal diagnosis of choledochal cyst at 15 weeks gestation: etiologic implications and management. Journal of pediatric surgery 24: 936-939.
- MacKenzie TC, Howell LJ, Flake AW (2001) The management of prenatally diagnosed choledochal cysts. Journal of pediatric surgery 36: 1241-1243.
- Khmekhem R, Zitouni H, Ben Ahmed Y (2012) Traitement chirurgical des dilatations kystiques de la voie biliaire chez l’enfant. Résultats d’une série de 16 observations. Journal de pédiatrie et de puériculture 25: 199-205.
- Vries JS, Vries S, Aronson DC (2002) Choledochal cysts: Age of presentation, symptoms, and late complications related to Todani’s classification. Journal of pediatric surgery 37: 1568-1573.
- Okada T., Sasaki F., Ueki S (2004) Postnatal management for prenatally diagnosed choledochal cysts. Journal of pediatric surgery 39: 1055-1058.
- Seifarth FG (2013) Concordance of imaging modalities and cost minimization in the diagnosis of pediatric choledochal cysts. Journal of pediatric surgery 48: 472.
- Levy AD, Rohramann CA (2003) Biliary cystic disease. Curr probl Diagn. Radiol 32: 233-263.
- Wax BN, Durie NM, Khullar P, Price AP, Coren CV et.al, (2007) Radiology–pathology conference: choledochal cyst. Clinical Imaging 31: 269-272.
- Nakamura H, Katayose Y, Rikiyama T, Onogawa T, Yamamoto K, et al. (2008) Advanced bile duct carcinoma in a 15-year-old patient with pancreaticobiliary maljunction and congenital biliary cystic disease. J Hepatobiliary pancreat Surg 15: 554-559.
- Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K (1977) Congenital bile duct cysts. Classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg 134: 263-269.
- Yoon JH (2011) Magnetic resonance cholangiopancreatography diagnosis of choledochal cyst involving the cystic duct: report of three cases. The british journal of radiology 84: 18-22.
- Cussenot O, Valayer J, Gauthier F (1987) Dilatation congénitale de da voie biliaire. Chir Pédiatr 28: 8-19.
- Harper L, Lavrand F, Pietrera P (2006) Rupture spontanée d’un kyste du cholédoque chez un enfant de 11 mois. Archives de pédiatries 13: 156-158.
- Fumino S, Iwai N, Deguchi E, Ono S, Shimadera S, et al. (2006) Spontaneous rupture of choledochal cyst with pseudocyst formation. Report on 2 cases and literature review. Journal of pediatric surgery 41: 19-21.
- Khiari A, Gharbi A, Ghariani B (1999) Les malformations kystiques des voies biliaires: attitude diagnostique et thérapeutique. A propos de 13 cas. Tunisie chirurgicale 4: 164-170.
Relevant Topics
- About the Journal
- Birth Complications
- Breastfeeding
- Bronchopulmonary Dysplasia
- Feeding Disorders
- Gestational diabetes
- Neonatal Anemia
- Neonatal Breastfeeding
- Neonatal Care
- Neonatal Disease
- Neonatal Drugs
- Neonatal Health
- Neonatal Infections
- Neonatal Intensive Care
- Neonatal Seizure
- Neonatal Sepsis
- Neonatal Stroke
- Newborn Jaundice
- Newborns Screening
- Premature Infants
- Sepsis in Neonatal
- Vaccines and Immunity for Newborns
Recommended Journals
Article Tools
Article Usage
- Total views: 5179
- [From(publication date):
December-2016 - Aug 19, 2025] - Breakdown by view type
- HTML page views : 4229
- PDF downloads : 950