Glucagonoma Revealed by a Necrolytic Migratory Erythema
Received: 10-May-2021 / Accepted Date: 14-May-2021 / Published Date: 21-May-2021 DOI: 10.4172/2167-7964.1000330
Abstract
Glucagonoma is a rare pancreatic neuroendocrine tumor that usually develops in the body or tail of the pancreas. Both imaging features of a pancreatic tumor and elevated glucagon serum levels confirm the diagnosis. We report the case of a patient presenting with diffuse erythematous lesions consistent with necrolytic migratory erythema.
Text
Glucagonomas account for 1% of neuroendocrine tumors and less than 5% of primary pancreatic malignancies [1], arising from the alpha islet cells of Langerhans. Although it may appear to be a benign condition, 80% have malignant potential [2] with 50% of metastatic disease at the time of diagnosis the most common site being the liver [3,4].
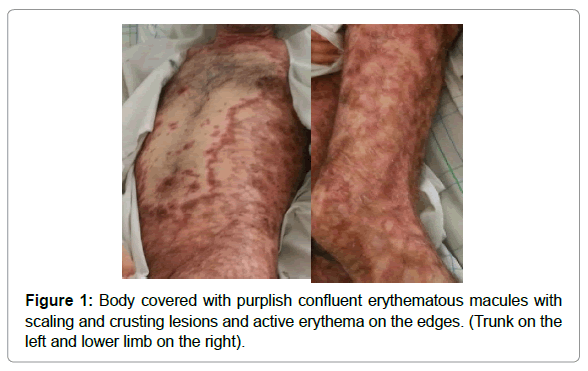
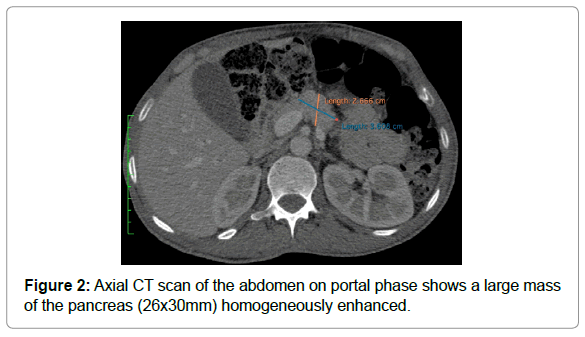
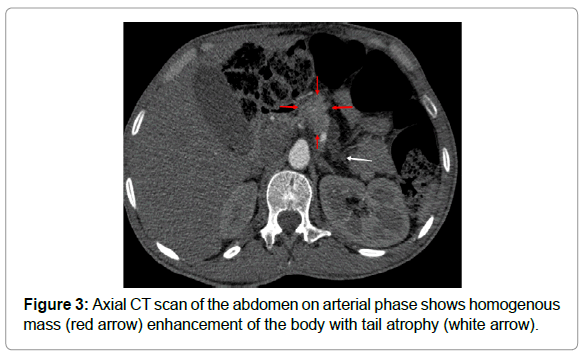
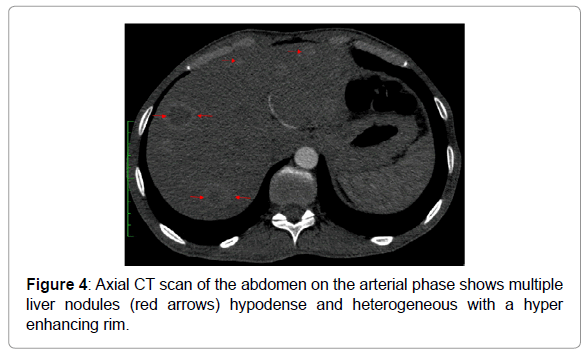
We report the case of a 53-year-old male with persistent painful diffuse erythematous skin lesions of the trunk, upper and lower limbs as well as on the perineum Figure 1, and had experienced weight loss. Laboratory analysis showed hyperglycemia and hyperglucagonemia. Computed tomography (CT), revealed a well-circumscribed corporeal pancreatic lesion, homogeneously enhanced Figure 2, with tail atrophy Figure 3, no calcification, no fat stranding, and no lymphadenopathy. Further investigation showed multiple hypodense liver nodules on the arterial phase Figure 4.
Glucagonomas are typically revealed by the glucagonoma syndrome triad characterized by a Para neoplastic syndrome associating the presence of a pancreatic mass, diabetes mellitus, and necrolytic migratory erythema (NME) [5]. Sometimes, the various clinical presentations can be misleading, but the presence of a painful scaly erythematous rash (Figure 1) is one of the first signs of onset. NME is in fact the most specific and hallmark clinical sign present in 70% of cases [2].
The diagnosis is confirmed by both laboratory tests with elevated levels of glucagon and imaging features of a pancreatic neuroendocrine tumor.
On CT scan it appears as a large (2 to 5cm of diameter), well-defined mass (Figure 2), of the body or the tail of the pancreas. After contrast injection, during the arterial phase, they tend to be homogeneous or inhomogeneous hypodense, generally well despicable with respect to the adjacent parenchyma, and hypodense or are Odense during the portal phase, due to their vascularization Figure 3. [6]
The presence of peripheral calcifications, cystic or necrotic changes along with lymphadenopathies are suggestive of the malignant potential [7].
The CT investigation should also look for any vessel involvement and assess for liver metastasis [8]. These appear to be hypodense nodules with arterial phase enhancement and tend to overall resemble the imaging features of the primary tumor [9,10] Figure 4.
Surgical resection is the optimal strategy for the treatment of glucagonoma [9] with the disappearance of skin lesions and normalization of glucagon levels shortly after surgery. Patients who undergo resection have longer median survival than patients who did not receive surgery, even when diagnosed with later stages of the disease because of its slow growth [11].
References
- Lv WF, Han JK, Liu X, Wang SC, Pan BO, et al (2015) Imaging features of glucagonoma syndrome: A case report and review of the literature. Oncol Lett 9(4):1579-1582.
- Drematcheff S, Lalande Champetier de Ribes T, Marty C, Sans N, Railhac JJ (2004) Érythème nécro lytique migrateur et tumeur pancréatique: le glucagonome. J Radiol 85(3):329-331.
- Hellman P, Andersson M, Rastad J, Juhlin C, Sadettin Karacagil (2000) Surgical strategy for large or malignant endocrine pancreatic tumors. World J Surg 24(11):1353-1360.
- James C. Yao, Eisner MP, Leary C, Dagohoy C, Phan A, et al. (2007) Population-based study of islet cell carcinoma. Ann Surg Oncol 14(12):3492- 3500.
- Mallinson CN, Bloom SR, Warin AP (1979) A glucagonoma syndrome. Lancet 7871;(304):1-5.
- D Onofrio M, Capelli P, Pederzoli P (2015) editors. Imaging and pathology of pancreatic neoplasms. A pictorial atlas. Milan: Springer.
- Yao JC, Eisner MP, Leary C, Dagohoy C, Phan A, et al. (2007) Populationbased study of islet cell carcinoma. Ann Surg Oncol 14(12):3492-3500.
- Tamm EP, Bhosale P, Lee JH, Rohren EM (2016) State-of-the-art Imaging of Pancreatic Neuroendocrine Tumors. Surg Oncol Clin N Am 25(2):375-400. 9. Horton KM, Hruban RH, Yeo C, Fishman EK (2006) Multi-detector row CT of pancreatic islet cell tumors. Radiographic 26 ( 2):453-464.
- Papavramidis T, Papavramidis S (2005) Solid pseudo papillary tumors of the pancreas review of 718 patients reported in English literature. J Am Coll Surg 200(6): 965-972.
- Cardoso, Daniel Cardoso A, Filho F (2017) pancreatic glucagonoma associated with necrolytic migratory erythema: case report and clinical review. European Journal of Cancer 72; S151.
Citation: Khouchoua S, Onka B, Yehouenou TR, Amalik S, Jerguigue H, et al. (2021) Glucagonoma Revealed by a Necrolytic Migratory Erythema. OMICS J Radiol 10: 330. DOI: 10.4172/2167-7964.1000330
Copyright: © 2021 Khouchoua S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 3692
- [From(publication date): 0-2021 - Dec 20, 2025]
- Breakdown by view type
- HTML page views: 2820
- PDF downloads: 872