He Awatea Hou: Improving Health Literacy and Health Outcomes for Bariatric Patients
Received: 23-May-2019 / Accepted Date: 21-Aug-2019 / Published Date: 30-Aug-2019 DOI: 10.4172/2165-7904.1000387
Abstract
Objective: This evaluation aimed to determine the effectiveness of a whānau health literacy pilot at two District Health Boards (DHBs) in Auckland, New Zealand. The pilot had two distinct components including: (i) A whānau/fanau programme to encourage healthy lifestyles and improve health literacy, and (ii) The provider/service programme to identify service barriers to health literacy and create an action plan for change at the service level.
Methods: The evaluation design was quasi-experimental with a mixed methods approach involving a comparison (N=33) and intervention group (N=32). Participant and whānau outcomes were captured through: audit of clinical indicators, qualitative interviewing and patient survey and support scale responses. Service outcomes were measured through service indicators and the completion of the Ministry of Health, Framework for Health Literacy Review.
Results: Participant feedback demonstrates a high level of acceptability and satisfaction with navigator support. Key strengths of navigator support identified included: Enhanced patient accountability for lifestyle behavioural change, availability and accessibility of holistic support, the provision of helpful information and resources, and genuine care (manaakitanga) for bariatric patients and their whānau/fanau. A key theme in the kōrero of all evaluation participants was an emphasis on the psychological aspects of both preparing for and recovering from bariatric surgery. A second key theme was that the bariatric journey is largely self and whaanau directed. Participants from one DHB (CM Health) supported by navigators achieved surgery sooner (p=0.01), and had shorter LOS for any post-surgery readmissions (within 20 days of surgery) (p<0.0001) and fewer readmissions following their last outpatient clinic (t=4.68, p<0.0001). There were no statistically significant differences between comparison and intervention group outcomes for Waitemata DHB participants. Organisational health literacy action plans were not implemented at either DHB. Key barriers to action plan implementation included: lack of supportive systems, lack of leadership and management buy-in and support, and health literacy not being understood and therefore undervalued by some staff.
Conclusion: It is essential to prepare participants for the psychological impact of bariatric surgery and the extensive level of self and whānau/fanau-directed care that is needed. Navigator support can improve outcomes for bariatric patients.
Keywords: Health literacy; Bariatrics; Navigator; Psychological supports; Intervention; Surgery; Family inclusive care; Service improvement
Introduction
In New Zealand, attrition from bariatric surgery programmes is highest amongst Māori and Pacific populations [1,2]. A recent study suggests that as many as 73 per cent of Pacific and 50 per cent of Māori who are accepted onto bariatric programmes drop out prior to achieving bariatric surgery (compared to 39 percent of NZ Europeans) [2]. These groups experience high levels of overweight and obesity and poorer health outcomes than NZ Europeans [3], and therefore have greater need for bariatric surgery. Like those in other OECD countries, New Zealanders, and especially Māori, have poor health literacy skills [4]. Improving health literacy and whānau participation is critical for improving equity of access and outcome for bariatric surgery.
He Awatea Hou was a whānau health literacy pilot delivered at Counties Manukau Health (CM Health) and Waitemata District Health Board (DHB) from Jan 2015 to March 2017 with two key programme components. (1) The whānau programme aimed to improve the health literacy of bariatric patients and their whānau, and reduce the health literacy demands created by bariatric services. Patient and whānau support was delivered through navigators who worked to build the skills and knowledge of individuals and their whānau from referral to surgery completion, and acted as a link to the service when health literacy barriers were identified. (2) The service or provider programme aimed to identify service barriers to health literacy and create an action plan to improve organisational health literacy. The pilot design reflects a commitment to addressing both consumer capacity (i.e., patient knowledge and skills) alongside the organisational systems, processes and services that support ease of consumer access and navigation [5].
Research Methodology
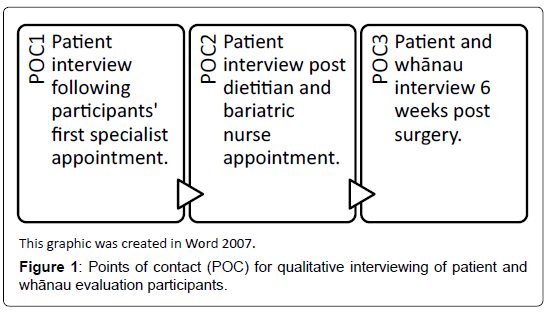
The evaluation design was quasi-experimental with a mixed methods approach, involving a comparison (N=33) and intervention group (N=32). Evaluation methods aimed to capture (i) patient and whānau outcomes and (ii) service outcomes. Patient and whānau outcomes were captured for both groups through clinical indicators, survey and support scale responses, and extensive semi-structured qualitative interviewing at three points of contact (POC) on the bariatric pathway (Figure 1). Typically, interviews were conducted face-to-face at health services or in participants’ homes. Some phone interviews were also conducted to minimise travel and time demands. Whānau were also invited to participate in interviews.
At the conclusion of all POC qualitative interviews, a survey was administered to patients which included a series of Likert statements exploring extent of patient agreement (or disagreement) with various aspects of the bariatric service (for example ‘The appointment was easy to find’, ‘I knew what to expect’, or ‘I felt comfortable asking questions’). Surveys also included other closed questions which ascertained if patients had attended with a support person, and how they would describe their relationship with the health professional they met. Surveys were informed by previous indicators published in The Health Literacy Umbrella better health model [6], which identified values and preferences, respect, plain language, clear dialogue, follow-up, technology, easy navigation, peer support, resources and education as determinants of health literacy. These surveys were completed by patients and whānau at POC3.
At POC3 a support scale was also completed by participants, which aimed to explore social and support networks available to bariatric patients. A rapid scan of existing family support scales in Medline, CINAHL, Google Scholar and the Cochrane Library with search terms ‘family support scale’, ‘social support scale’, ‘support scale and measurement’ was conducted. Of the seven published and accessible scales, none related to our demographic group or bariatric specialities, tending to focus more on caregiving relationships in families with children with disabilities. The selected scale for this study was adapted from the Family Support Scale [7], which has been extensively used to measure perceived helpfulness of both formal and informal supports available to families raising children, and demonstrates adequate face validity and internal consistency validity with this population [8]. This scale included a wide range of potential support across social networks, which was well attuned to concepts of whānau and extended familial groups.
The clinical indicators (Table 1) for participant outcomes collected through existing clinical information systems were defined by the Project Steering Group (PSG) in partnership with the evaluation team.
| Indicators | Description |
|---|---|
| Did not attend (DNA) rates | Total number of appointments attended, and total number of appointments scheduled but missed by patients. |
| Surgical outcome | How many evaluation participants completed bariatric surgery between July 2015 and July 5th 2017. |
| Length of stay (LOS) after surgery | The length of stay in hospital following surgery for participants who had surgery. |
| Time to theatre | Calculated from the first contact date to the operated date (inpatient admission) date, in days. This applied to only those participants who had surgery. |
| 30 day readmission after surgery | Whether the participant was readmitted within 30 days from operation. |
| Readmission length of stay (LOS) | For those participants who were readmitted into hospital within 30 days from operation, the length of the readmission event, in days. |
| 30 day readmission after last outpatient (OP) clinic | Whether the participant was been readmitted within 30 days from last OP clinic. |
| LOS for readmissions following OP clinic | Length of this readmission event, in days. |
| Mental health service admissions | Whether the participants was admitted within 1 year of operation date acutely to a mental health service. |
| Mortality | Whether the participant died within 30 days after operation. |
Table 1: Summary of patient outcomes indicators for analysis.
Service barriers to health literacy were identified using the framework outlined in Health literacy review: A guide [9]. The guide identifies six dimensions of health literacy:
i. Leadership and management
ii. Patient involvement
iii. Work-force
iv. Meeting needs of the population
v. Access and navigation and
vi. Communication
The service reviews were guided by a small working group (the Health Literacy Review Group, HLRG) at each DHB made up of members of the PSG and the project team. The HLRG included members of the project team (Toi Tangata, The Fono and Quigley and Watts), evaluators from Ko Awatea and staff from the service and DHB funding and planning teams.
Data for the service review were collected using a range of methods:
• Phone interviews with health professionals from the bariatric teams.
• Face-to-face interviews with 14 Māori or Pacific patients who had been through bariatric surgery and their whānau.
• Survey of health professionals in the bariatric surgical teams.
• Observations of bariatric information sessions, clinics and patient consultations (25 patients in total).
• Environmental observations of clinics and clinic settings.
• Review of all key bariatric surgical resources.
Clinical indicators were analysed quantitatively for frequency of distributions in time series. We compared the intervention and comparison groups across clinical outcomes and looked for statistically significant differences (t-test and Pearson correlation). Summary results are presented as counts and proportions for categories outcomes and mean with standard deviation (SD) for continuous outcomes. In order to determine statistically significant differences in the outcomes between the groups and to test for associations, two-sample t-tests and a chi-square test were used respectively. A significance level of less than five per cent was deemed as statistically significant.
Semi-structured interviews were audio recorded, transcribed and then thematically analysed with the aid of qualitative software package, NVivo. With scaled responses from patient and whānau health literacy surveys, we calculated the mean with standard deviation (SD) and the 95 per cent confidence intervals (CI) for scores. Effect size was used to quantify the size of the difference in the scale between the two groups, or the “magnitude of the difference between groups” [10]. Cohen defined d as the difference between the means, M1 - M2, divided by standard deviation, SD, of either group [11]. Cohen hesitantly defined effect sizes as “small d=0.2,” “medium d=0.5,” and “large d=0.8”. We also looked for correlation between ‘levels’ of support and indicators such as DNA and attrition rates.
Results
In total, 65 patients consented to participate in this evaluation, including 33 who participated prior to service changes and intervention (referred to as the comparison group) (Table 2), and 32 who were supported by navigators at Toi Tangata or Te Fono (intervention group) (Table 3). We were able to collate clinical indicators for 32 comparison group participants, and 29 intervention group participants. Five participants were excluded from the analysis of clinical indicators as their National Health Index (NHI) or other personal information was not able to be matched and validated with clinical records accessible to analysts at each DHB. In total, 128 patient interviews and 116 surveys were completed.
| Comparison group participants (N=32, 14 CM Health and 18 Waitemata DHB) | |||||
|---|---|---|---|---|---|
| Age group | Sex, N /% (0 d. p.) | Ethnicity N /% (0 d.p.) | |||
| 0 – 25 years | 2/6% | Female | 21/66% | Maori | 8/25% |
| 26 – 45 years | 18/56% | Male | 11/34% | Pacific Island | 5/16% |
| 46 – 65 years | 12/38% | - | - | European | 13/41% |
| 65 + | 0 | - | - | Asian | 0/0% |
| Unknown | 0 | - | - | Not stated | 1/3% |
| 0 | - | - | Other | 5/16% | |
Table 2: Demographic summary for evaluation participants in the comparison group.
| Intervention group participants (N=29, 18 CM Health and 11 Waitemata DHB) | |||||
|---|---|---|---|---|---|
| Age group | Sex | Ethnicity | |||
| 0 – 25 years | 1/3% | Female | 18/62% | Maori | 14/48% |
| 26 – 45 years | 15/52% | Male | 11/38% | Pacific Island | 7/24% |
| 46 – 65 years | 12/41% | - | - | European | 6/21% |
| 65 + | 0 | - | - | Asian | 1/3% |
| Unknown | 1/3% | - | - | Not stated | 0/0% |
Table 3: Demographic summary for evaluation participants in the group supported by navigators (intervention group)
CM Health participants supported by navigators achieved surgery sooner (p=0.01) and had shorter LOS for any post-surgery readmissions (within 20 days of surgery) (p<0.0001) and readmissions following their last outpatient clinic (t=4.68, p<0.0001) (Table 4). Though they did not reach statistical significance, indicative trends were also notable for the following indicators: LOS after surgery, readmission rates within 30 days of last outpatient clinical, and appointment DNA rate. Further research is needed to test for significance of these improvements with a larger sample size (Table 4).
| Indicators | Description | Results |
|---|---|---|
| Surgery | How many evaluation participants secured a surgical place and completed surgery from June 2015 to July 5th 2017. | 56% of intervention group received surgery and 43% of the comparison group. This difference is not statistically significant OR 0.76 (95% CI 0.23-2.5), p=0.65. |
| Length of stay (LOS) after surgery | The length of stay in hospital following surgery for participants who had surgery. | LOS was shorter in intervention group (1.9 days mean, range 1.19-2.3) compare to control group (2.43 mean, range 1.19-2.33). |
| Time to theatre | Time to theatre was calculated from the first contact date to the operation date (inpatient admission), in calendar days. This applied to only those participants who had surgery. | Average time to theatre was 213.5 days (range 157.7-291.7) in the intervention group, and 310.8 days in the comparison group (range 214-433.7). This difference was statistically significant (p=0.01). |
| 30 day readmission after surgery | Whether the participant was readmitted within 30 days from operation | 30 day readmission after surgery was double in the comparison group than the intervention (43% versus 22%). This difference is not statistically significant OR=2.1 (95%CI 0.50-8.75) p=0.30. |
| Readmission length of stay (LOS) | For those participants who were readmitted into hospital within 30 days from operation, the length of the readmission event, in days. | LOS for readmissions was less than half in the intervention group at 3.1 days on average for the intervention group (range 2.1-4.2) and 7.9 days on average in the comparison group (range 0.2-38.8). This result was statistically significant (p<0.0001). |
| 30 day readmission after last outpatient (OP) clinic | Whether the participant was readmitted within 30 days from their last OP clinic. | 30 day readmission after last OP clinic was higher in the comparison group than the intervention (57% versus 44%). This difference was not statistically significant OR=1.24 (95% CI 0.39-3.97), p=0.71. |
| LOS for readmissions following OP clinic | Length of this readmission event, in days. | The LOS was halved in the intervention group (3.01 days on average, range 0.4-5.0) when compared to the comparison group (6.35 days on average, range 0.8-32.8). This result was statistically significant (t=4.68, p<0.0001). |
| Mental Health Service admissions | Whether the participant was admitted within 1 year of operation date acutely to the Mental Health Service. | No patients (including comparison and intervention groups) were admitted to the Mental Health Service within a year after surgery. Note that it has not been a year since surgery for all patients. |
| Did not attend rate (DNA) | Number of scheduled clinical appointments with the Bariatric Service not attended by participants. | Patient DNA rate was lower in the intervention group (0.67 appointments per patient on average) when compared with the control group (0.86 appointments per patient on average). |
| Mortality | Whether the participant died within 30 days after operation. | There were no patient deaths in the study group. |
Table 4: Clinical outcome indicators for control and intervention groups at CM Health.
There were no statistically significant differences between comparison and intervention group outcomes for Waitemata DHB participants. Non-significant indicative trends for Waitemata DHB participants suggest that fewer patients achieved bariatric surgery, and average time to theatre was longer in the intervention group (Table 5).
| Indicators | Description | Results |
|---|---|---|
| Surgery | How many evaluation participants secured a surgical place and completed surgery between June 2015 to July 5th 2017. | 28% of the intervention and 71% of the comparison group achieved surgery. This difference was not statistically significant OR=2.44 (95%CI 0.56-10.64), p=0.23. |
| Length of stay (LOS) after surgery | The length of stay in hospital following surgery for participants who had surgery. | Average LOS was shorter in the intervention group (2.75 days mean, range 2-5) and 3.1 days in the comparison group (range 2-5). |
| Time to theatre | Time to theatre was calculated from the first contact date to the operated date (inpatient admission) date, in days. This applied to only those participants who had surgery. | Average time to theatre was 353 days intervention group who received surgery (N=4, range 177-457) and 278 days in the comparison group (N=10, range 128-421). |
| 30 day readmission after surgery | Whether the participant was been readmitted within 30 days from operation | There were no readmissions within thirty days of surgery in the intervention group and only one (5.5%) in the comparison group. |
| Readmission length of stay (LOS) | For those participants who were readmitted into hospital within 30 days from operation, the length of the readmission event, in days. | N/A |
| 30 day readmission after last outpatient (OP) clinic | Whether the participant was been readmitted within 30 days from Last OP clinic. | There were no readmissions for Waitemata patients. |
| LOS for readmissions following OP clinic | Length of this readmission event, in days | N/A |
| Mental Health Service admissions | Whether the participants was admitted within 1 year of operation date acutely the Mental Health Service. | No patients (including comparison and intervention groups) were admitted to the Mental Health Service within a year after surgery. Note that it has not been a year since surgery for all patients. |
| Did not attend rate (DNA) | Number of scheduled clinical appointments with the Bariatric Service not attended by participants. | Patient DNA was lower in the comparison group (0.3 appointments per patient on average) than in the intervention group (0.43 appointments on average). |
| Mortality | Whether the participant died within 30 days after operation | There were no patient deaths in the study group. |
Table 5: Clinical outcome indicators for control and intervention groups at Waitemata DHB.
Participant feedback demonstrates a high level of patient acceptability and satisfaction with navigator support. Key strengths of navigator support that were identified by participants included enhanced accountability for lifestyle behavioural change, availability and accessibility of holistic support, the provision of helpful information and resources, and genuine care (manākitanga) for bariatric patients and their family or whānau.
Although they did not reach statistical significance, whānau/fanau supported by navigators indicated moderate to large improvement on the following indicators:
• Finding the doctors and nurses friendly and welcoming (d=0.5)
• Feeling well informed (d=0.5)
• Feeling helpful supporting their whānau to reach their presurgery goals (d=0.5)
• Taking care of their whānau following surgery (d=0.67)
Intervention group participants also reported moderate to large improvement in:
• Pre-surgery preparation support from patients ‘brothers and sisters’ (d=0.69), ‘other people in my household’ (d=0.65), ‘other’ supports (d=1.37)
• Post-surgery supports, including ‘my partners parents’ (d=- 0.54), the ‘dietitian’ (d=-0.79), and ‘my brothers or sisters’ (d=0.96).
A large effect size which favoured the comparison group was also calculated for ‘my children’ and ‘my partner’ both pre- and postsurgery, perhaps resulting from the introduction of navigator support which reportedly reduced burden of care on family or whānau.
From qualitative interviews, we derived two key themes as follows:
(1) ‘The psychological journey is a central part of the bariatric experience’ and
(2) ‘The journey is largely self and whānau directed’.
A key theme in the kōrero of all evaluation participants was an emphasis on the psychological aspects of both preparing for and recovering from bariatric surgery. Inherent in this preparation and recovery were patients’ efforts to get in the right ‘mind set’ for changing and maintaining lifestyle behaviours, embracing their new (or renewed) identity, coping and support seeking, and fundamentally changing their relationships with food:
“It’s your head. Your head has to be in the right place and you can have a million support workers, you can have millions of dollars but if your head is not in the right place you’re not going to do it . . . It’s a huge part of it and I think that’s why people end up failing at the other end. You have to be mentally prepared and you have to have the focus of why you want to do it and what you expect to get out of it and your long term goals. I wasn’t ready for any of that before but I am now” (Intervention group participant).
We found that bariatric surgery and associated changes in lifestyle behaviours may challenge the roles and cultural norms that comprise a patient’s social identity [12] – requiring significant psychological or emotional support that was largely delivered by family/whānau/ fanau. Participants identified gaps in the availability of psychological and emotional support provided by bariatric services at both DHBs. Intervention group participants also received this support from navigators; reportedly reducing the burden of care on family/whānau.
A second key theme was that the bariatric journey is largely self and whānau directed. Participant narratives of the bariatric experience highlight their autonomy and sometimes isolation on the bariatric pathway as they (i) navigate the bariatric pathway, (ii) seek information and peer support, and (iii) make decisions about their health and care. Amongst participants who achieved surgery, the bariatric pathway from the information session to surgery completion ranged between 128 and 457 days; an average of 24.5 or 26.4 days between appointments at CM Health and Waitemata DHB respectively. Between appointments, participants depended largely on family and social support networks for support and advice. People who had previously undertaken bariatric surgery were identified as particularly helpful.
Fourteen evaluation participants (22%) reported a lack of oversight of the service pathway. There were limited opportunities for DHBfacilitated networking or interaction between patients. Existing group appointments (such as the information sessions) lacked opportunities for patients to connect and be introduced to each other.
The service review successfully identified barriers to health literacy within each service and developed a plan with goals and actions to address the barriers. The barriers identified across the two DHBs were similar:
• Health literacy is not understood by all staff and therefore not effectively prioritised.
• Understanding and use of the universal precautions approach to build patient health literacy is low amongst staff.
• There are few formal policies or processes focused on health literacy.
• There are limited opportunities for patient and whānau involvement in the design and delivery of bariatric surgical services.
• Not all patients were able to access the support they needed from the service or their family to achieve successful outcomes.
• The quality (action-ability and readability) of written resources varied greatly.
• Effective communication strategies were not consistently utilised by all health professionals.
The service component of the pilot had minimal impact on the delivery of bariatric surgical services at either DHB because neither service was able to implement the action plan. A small number of interventions identified within the action plan were actioned by members of the PSGs at both DHBs. For example, changes to chairs at the information session and consent processes at CM Health, and patient nutrition resources at Waitemata DHB. Other actions that were arguably more important were not implemented. Key barriers to action plan implementation included: lack of supportive systems, lack of leadership and management buy-in and support, and health literacy not being understood by all staff and therefore not effectively prioritised.
Discussion
This evaluation explored the effectiveness of a whānau health literacy pilot project (He Awatea Hou) in regards to patient and whānau health literacy, health outcomes, and delivery of bariatric surgery services at CM Health and Waitemata DHB. This initiative was designed in response to evidence which suggests that to increase the effectiveness of health literacy interventions, they should take a wholeof- systems approach. Such approaches embed a socio-ecological or socio-cultural theory of change that emphasises the social contexts in which people live [13].
Evaluation findings highlight that the psychological (i.e., emotional and social) impact of bariatric surgery is a central part of preparing for and making sense of bariatric surgery, and the extensive level of self- and whānau-directed care that is undertaken on the bariatric pathway. These findings emphasise the importance of supports (such as those provided by navigators) that address the emotional and social aspects of care, in the day-to-day context of long term commitments to lifestyle behaviour change. Navigator support for intervention group participants proved to be an integral provider of this psychological support, and further, between appointment care and accountability. This could be further enhanced through increased opportunities for DHB facilitated peer networking and support, for example, patient support groups and/or expert patients to support new patients pre- and post-surgery.
Nieves-Khouw et al. have highlighted that a patient’s weight loss pathway through bariatric surgery is a long process in which commitment, persistence and focus from the patient are needed, so that lifestyle changes are implemented and weight loss is maintained [14]. Amongst other strategies Nieves-Khouw and colleagues suggest using psychological methods like individual or group therapy as well as standard patient education approaches to achieve this. Further, they recommend “informational content should address psychological issues that are critical in the bariatric patient’s ability to comply with the dietary and behavioural changes required to achieve the successful outcome of bariatric surgery” [14].
That neither service was able to fully implement action plans is a crucial finding relating to future efforts to improve health literacy in the New Zealand healthcare system. Identified barriers to health literacy were similar across CM Health and Waitemata DHB, many of which are also consistent with existing literature. For example, lack of awareness, including not knowing or understanding what health literacy is [15,16] or believing that there isn’t a problem with health literacy in the organisation [17]. Lack of buy-in from medical professionals [18] and staff attitudes were also identified as barriers in existing literature (e.g. health literacy is ‘not my job’, ‘there’s nothing we can do about it’, ‘it is the patient’s fault’ [18], ‘it’s not important enough compared to other priorities’ [19]).
Despite the strategic focus of health literacy at both CM Health and Waitemata DHB, lack of progress with action plans at both DHBs has highlighted the importance of supportive systems, leadership and management in becoming a health literate organisation. Our findings are consistent with previous studies which have highlighted lack of leadership support [19] lack of formal policies and role ambiguity [16] and real or perceived lack of time allocated for staff to carry out health literacy activities [20].
Conclusion
Persistent organisational barriers to becoming a health literate organisation undermine service improvement efforts, and indicate the need for proper consideration of how health literacy is prioritised, enacted and resourced. It is essential to prepare participants for the psychological impact of bariatric surgery and the extensive level of self and whānau/fanau-directed care that is needed. Navigator support can improve outcomes for bariatric patients.
Compliance with Ethical Standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the New Zealand Health and Disability Ethics Committee, (Reference: #15/CEN/37) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Acknowledgements
The work was funded by the Ministry of Health and was awarded from a contestable tender process. The project team included Quigley and Watts, Toi Tangata and The Fono working in partnership with Counties Manukau Health (CM Health) and Waitemata District Health Board (Waitemata DHB). We extend our deep appreciation to all of the evaluation participants who have so courageously shared their experience of elective bariatric surgery services with us to better support future patients of these services and their whānau/fanau or family.
References
- Taylor T, Wang Y, Rogerson W, Bavin L, Sharon C, et al. (2018) Attrition after acceptance onto a publicly funded bariatric surgery program. Obesity surgery 28: 2500-2507.
- Rahiri JL, Lauti M, Harwood M, MacCormick AD, Hill AG (2018) Ethnic disparities in rates of publicly funded bariatric surgery in New Zealand (2009–2014). ANZ J Surgery 88: E366-E369.
- Ministry of Health (2015b) Understanding excess body weight: New Zealand Health Survey.
- Ministry of Health (2010) KÅrero MÄrama: Health literacy and mÄori. Results from the 2006 Adult Literacy and Life Skills Survey.
- Ministry of Health (2015) A framework for health literacy. Wellington, NZ.
- Davis C, McQuillen K, Rootman O, Gadbsy L, Walker L, et al. (2009 Impact BC and the health literacy in communities prototype facility.Â
- Dunst CJ (1984) The family support scale: Reliability and validity. J Individual, Family Commu Wellness 1: 45-52.
- Littlewood K, Swanke JR, Strozier A, Kondrat D (2012) Measuring social support among kinship caregivers: Validity and reliability of the family support scale. Child Welfare. 91: 59-78.
- Ministry of Health (2015) Health literacy review: A guide. Wellington, NZ.
- Sullivan GM, Feinn R (2012) Using effect size or why the P value is not enough. J graduate med edu 4: 279-282.
- Cohen J (1988) Statistical power analysis for the behavioral sciences (2nd edn.). Hillsdale, NJ: Lawrence Earlbaum Associates, USA.
- Tajfel H, Turner JC (1979) An integrative theory of intergroup conflict. The social psychology of intergroup relations 4: 33-37.
- Scott P (2017) Global panel on agriculture and food systems for nutrition: Food systems and diets: Facing the challenges of the 21st century.
- Nieves-Khouw F, Welton R, Muchow N (2009) Bariatric surgery: Beyond informed consent. Bariatric Nursing and Surgical Patient Care 4: 191-202.
- Rootman I, Gordon-El-Bihbety D (2008) A vision for a health literate Canada. Ottawa, ON: Canadian Public Health Association.
- Weaver NL, Wray RJ, Zellin S, Gautam K, Jupka K (2012) Advancing organizational health literacy in health care organizations serving high-needs populations: A case study. J Health Commun 17: 55-66.
- Abrams MA, Sabrina KR, Riffenburgh A, Savage BA (2014) Building health literate organizations: A guidebook to achieving organizational change. Wes Des Moines, Iowa: Unity Point Health.
- French M, Hernandez LM (2013) Organizational change to improve health literacy: Workshop summary. National Academies Press.
- Shoemaker SJ, Staub-DeLong L, Wasserman M, Spranca M (2013) Factors affecting adoption and implementation of AHRQ health literacy tools in pharmacies. Res Social Adm Pharm 9: 553-563.
- Lambert V, Keogh D (2014) Health literacy and its importance for effective communication. Part 1. Nurs Child Young People 26: 31-37.
Citation: Hayward B, Watts C, Villa L, MacCormick A, Atkinson M, et al. (2019) He Awatea Hou: Improving Health Literacy and Health Outcomes for Bariatric Patients. J Obes Weight Loss Ther 9:387. DOI: 10.4172/2165-7904.1000387
Copyright: © 2019 Hayward B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3842
- [From(publication date): 0-2019 - Dec 06, 2025]
- Breakdown by view type
- HTML page views: 2932
- PDF downloads: 910