Heterotopic Quadruplet Gestation after Uncontrolled Ovulation Induction: A Case Report
Abstract
A heterotopic pregnancy is a rare condition in which at least two simultaneous gestations occur at two different implantation sites. A high rate of suspicion can be crucial in timely diagnosis and appropriate interventions. We report the very rare case of a nulliparous woman presented to the emergency department with hemoperitoneum from a ruptured tubal pregnancy in a spontaneous conception after self-uncontrolled ovulation induction resulting in a quadruplet heterotopic pregnancy: A triplet intrauterine pregnancy and a single left tubal ectopic pregnancy. An heterotopic pregnancy is an obstetric complication of difficult clinically diagnose and in most cases, surgically confirmed. This early approach is indispensable especially when there are hemodynamic repercussions. The factors related to the higher risk of developing heterotopic pregnancy coincide with those associated with ectopic pregnancy. In this case the hyperovulation caused by uncontrolled ovulation inducers was the most likely factor in the genesis of this condition.
Keywords: Heterotopic pregnancy; Ectopic pregnancy; Ovulation induction
Case Report
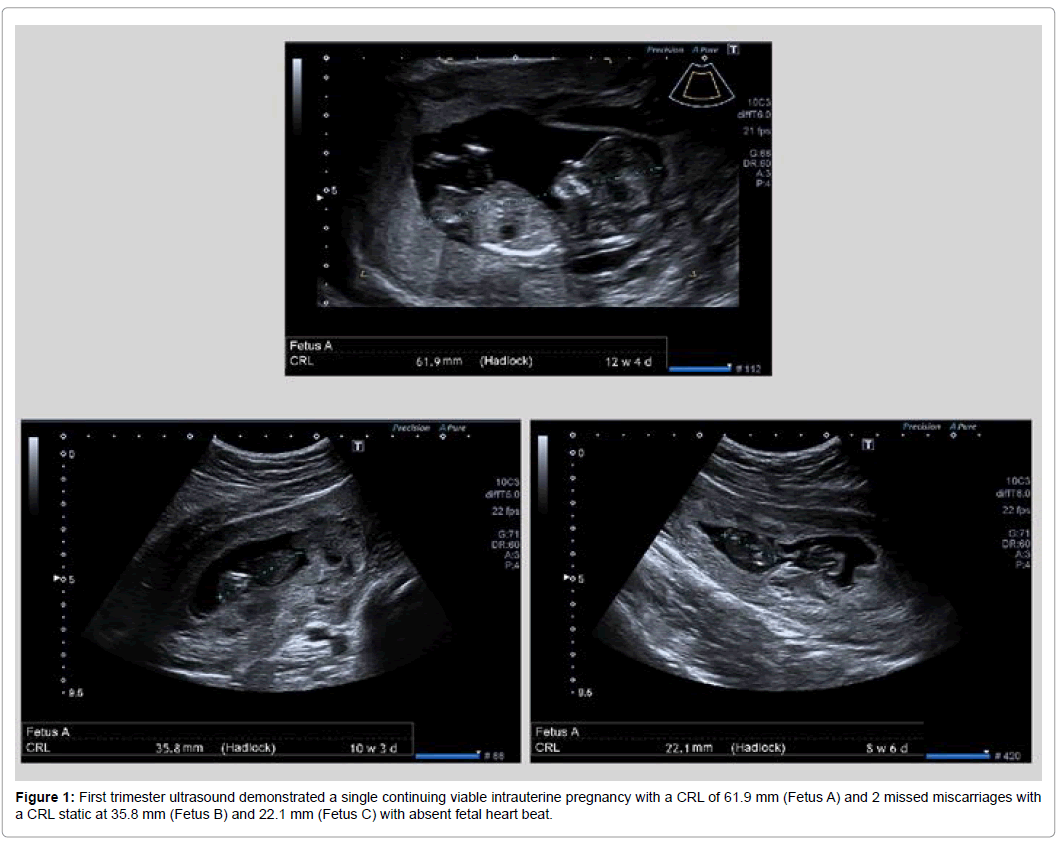
A 31 year old healthy nulliparous woman, diagnosed with primary infertility on waiting list for medically assisted procreation techniques in the Portuguese National Health Service is presented to the emergency department with a complaint of sudden onset of lower abdominal pain after self-uncontrolled ovulation induction, fact only known in the postoperative period. On physical examination, she was pale, hemodynamically unstable with a blood pressure of 69/31 mmHg and heart rate of 102 beats/min. A distended abdomen was showed at examination with diffuse abdominal tenderness. Transvaginal sonography demonstrated 3 intrauterine gestational sacs, 1 with positive embryocardium. Transabdominal ultrasound revealed a large amount of free fluid in the abdominal cavity. In analyzes taken at the emergency department, a 5.4 g/dL hemoglobin was found without other relevant changes. A transfusion with 3 units of red blood cells was performed and an exploratory laparotomy was decided. In the surgery was objectified a ruptured ectopic pregnancy in the left tubal ampulla with a large volume hemoperitoneum being submitted to a left salpingectomy without intercurrences. The histopathological examination confirmed an ectopic pregnancy. The postoperative period was uneventful and was discharged 2 days after surgery. First trimester ultrasound, 3 weeks postoperatively, demonstrated a single continuing viable intrauterine pregnancy with a CRL of 61.9 mm and 2 missed miscarriages with a CRL static at 35.8 mm and 22.1 mm with absent fetal heart beat (Figure 1).
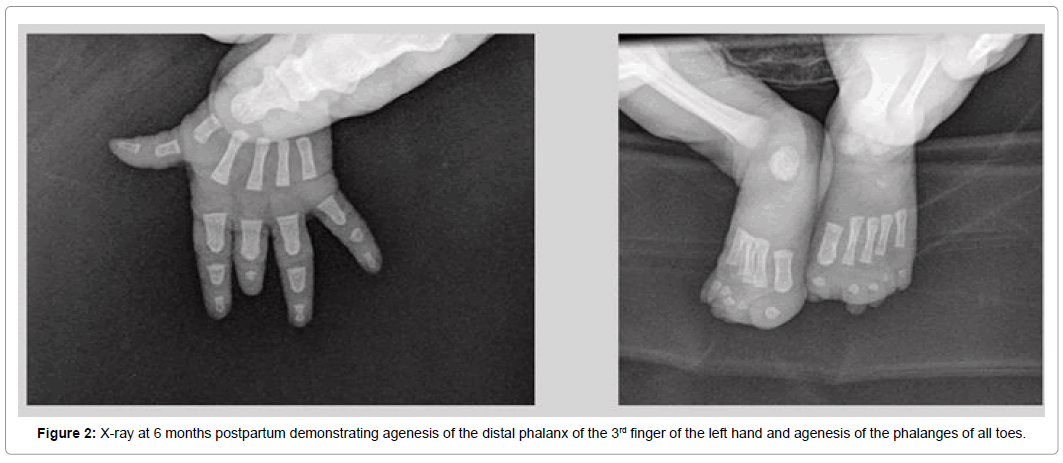
Gestation progressed to term with the birth of a newborn female, weighing 2285 g, with agenesis of the distal phalanx of the 3rd finger of the left hand and agenesis of the phalanges of all toes. Follow-up at 6 months did not show any changes other than malformations detected at birth (Figure 2).
Discussion
Heterotopic pregnancy consists of the presence of at least two simultaneous pregnancies at different sites of implantation, most often a combination of intrauterine and ectopic pregnancies. The vast majority of ectopic pregnancies occur in the fallopian tube but may also occur in other places such as the cervix, ovary, interstitial (cornual) tubular segment as well as anywhere in the abdominal cavity [1,2].
The incidence of heterotopic pregnancy, initially estimated at 1 in 30.000 pregnancies, is thought to be currently around 1 in 7.000 due to the proliferation of medically assisted reproduction techniques [3,4]. Obviously, a heterotopic quadruplet gestation is an even rarer event.
The increased incidence in this type of pregnancy may be due to a higher rate of tubal disease in this population, high levels of estradiol and progesterone as well as the transfer of more than one embryo [5,6]. The hydrostatic forces generated during embryo transfer may also contribute to the increased risk [1,2]. Other risk factors that may predispose to this pathology include for example endometriosis, pelvic inflammatory disease, a previous tubal surgery as well as smoking [7,9].
In most cases, a heterotopic pregnancy is diagnosed between 5 and 8 weeks of gestation, although the diagnostic window is much wider [10]. The clinical presentation of heterotopic pregnancies is in every way similar to a threat of abortion or ectopic pregnancy. As a rule, these patients present with abdominal pain, adnexal mass and eventual peritoneal irritation in the presence, most of the time, of an intrauterine gestation. Since the diagnosis is very difficult to perform, there is a high incidence of rupture complicated with acute abdomen and/or hemodynamic shock in this pathology [11,12].
In the presence of an intrauterine pregnancy, sudden and intense abdominal pain should have as obstetrical differential diagnoses the threat of abortion, heterotopic pregnancy and rupture of the corpus luteum. Appendicitis, nephrolithiasis and urinary tract infection may also mimic the clinic of a heterotopic pregnancy, so the suspicion for this pathology should be high, especially in the presence of risk factors.
The treatment of ectopic pregnancy should be directed to the site of implantation. Early diagnosis allows to consider non-surgical options for its resolution, always with the objective of preserving the concomitant intrauterine pregnancy [13]. Medical therapy with methotrexate is contraindicated in the presence of an evolutionary intrauterine pregnancy as in this case [14].
Surgical exploration continues to play a crucial role in the diagnosis of this pathology. In hemodynamically stable patients exploratory laparoscopy is the preferred approach, offering a faster recovery and a lower rate of postoperative infection limiting the adverse effects on a possible intrauterine pregnancy. The salpingectomy is the standard surgical procedure of a coexistent tubal pregnancy [15].
One in three coexisting intrauterine pregnancies end up spontaneously abort after resolution of the acute condition, a higher rate compared to that of a single intrauterine pregnancy [16]. In heterotopic pregnancies, maternal mortality is due to complications that may occur with the ectopic pregnancy. The estimated death related to ectopic pregnancy is 31.9 per 100.000 pregnancies, being that the majority of mortalities is due to intraperitoneal bleeding of ruptured ectopic pregnancy [17]. The fertility rates after treatment of ectopic pregnancy with salpingostomy, salpingectomy or methotrexate are similar. Women with a previous heterotopic pregnancy are more likely to develop an ectopic gestation in the future [18].
Conclusion
The heterotopic gestation is an obstetric complication difficult to diagnose clinically and, in most cases, surgically confirmed. This early approach is indispensable especially when there are hemodynamic repercussions. In this case, an exploratory laparotomy was chosen because of the patient's hemodynamic instability. The factors related to the higher risk of developing heterotopic pregnancy coincide with those associated with ectopic pregnancy. In this case the hyperovulation caused by uncontrolled ovulation inducers was the most likely factor in the genesis of this condition.
References
- Rojansky N, Schenker JG (1996) Heterotopic pregnancy and assisted reproduction-an update. J Assist Reprod Genet 13: 594-601.
- Pisarska MD, Carson SA (1999) Incidence and risk factors for ectopic pregnancy. Clin Obstet Gynecol 42: 2-8.
- Lyons EA, Levi CS, Sidney M (1998) In: Rumak CM, Wilson SR, Charboneau WK (Eds), Dashefsky in diagnostic ultrasound, 2nd edition. 2: 999.
- Glassner MJ, Aron E, Eskin BA (1990) Ovulation induction with clomiphene and the rise in heterotopic pregnancies: A report of two cases. J Reprod Med 35: 175-178.
- Tal J, Haddad S, Gordon N, Timor-Tritsch I (1996) Heterotopic pregnancy after ovulation induction and assisted reproductive technologies: A literature review from 1971 to 1993. Fertil Steril 66: 1-12.
- Clayton HB, Schieve LA, Peterson HB, Jamieson DJ, Reynolds MA, et al. (2007) A comparison of heterotopic and intrauterine-only pregnancy outcomes after assisted reproductive technologies in the United States from 1999 to 2002. Fertil Steril 87: 303-309.
- Simsek T, Dogan A, Simsek M, Pestereli E (2008) Heterotopic triplet pregnancy (twin tubal) in a natural cycle with tubal rupture: Case report and review of literature. J Obstet Gynaecol Res 34: 759-762.
- Inion I, Gerris J, Joostens M, Vree BD, Kockx M, et al. (1998) An unsuspected triplet heterotopic pregnancy after replacement of two embryos. Hum Reprod 13: 1999-2001.
- Strandell A, Thornburn J, Hamberger L (1999) Risk factors for ectopic pregnancy in assisted reproduction. Fertil Steril 71: 282-286.
- Talbot K, Simpson R, Price N, Jackson SR (2011) Heterotopic pregnancy. J Obstet Gynaecol 31: 7-12.
- Cheng PJ, Chueh HY, Qiu JT (2004) Heterotopic pregnancy in a natural conception cycle presenting as hematometra. Obstet Gynecol 104: 1195-1198.
- Barrenetxea G, Barinaga-Rementeria L, De-Larruzea AL, Agirregoikoa JA, Mandiola M, et al. (2007) Heterotopic pregnancy: Two cases and a comparative review. Fertil Steril 87: 417.e9-15.
- Li XH, Ouyang Y, Lu GX (2013) Value of transvaginal sonography in diagnosing heterotopic pregnancy after in-vitro fertilisation with embryo transfer. Ultrasound Obset Gynecol 41: 563-569.
- Louis-Sylvestre C, Morice P, Chapron C, Dubuisson JB (1997) The role of laparoscopy in the diagnosis and management of heterotopic pregnancies. Hum Reprod 12: 1100-1102.
- Goldstein JS, Ratts VS, Philpott T, Dahan MH (2006) Risk of surgery after use of potassium chloride for treatment of tubal heterotopic pregnancy. Obstet Gynecol 107: 506-508.
- Grimes DA (2006) Estimation of pregnancy-related mortality risk by pregnancy outcome, United States, 1991 to 1999. Am J Obstet Gynecol 194: 92-94.
- Mol F, Mol BW, Ankum WM, Veen FVD, Hajenius PJ (2008) Current evidence on surgery, systemic methotrexate and expectant management in the treatment of tubal ectopic pregnancy: A systematic review and meta-analysis. Hum Reprod Update 14: 309-319.
- Sohinee B, David J, Amanda JL, Siladitya B (2012) Reproductive Outcomes following ectopic pregnancy: Register-based retrospective cohort study. PLoS Med 9: e1001243.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 3639
- [From(publication date): 0-2019 - Dec 17, 2025]
- Breakdown by view type
- HTML page views: 2738
- PDF downloads: 901