Holospinal Epidural Abscess – A Surgical Perspective
Received: 04-Jun-2019 / Accepted Date: 15-Jul-2019 / Published Date: 01-Aug-2019 DOI: 10.4172/2314-7326.1000289
Abstract
Holospinal epidural abscesses (HEAs) are exceedingly rare, with very few documented cases in the literature. It is a condition in which spinal epidural abscesses extend from the cervical to the sacral spine. Despite the increasing prevalence of spinal infections, the subcategory of HEAs is extremely infrequent and requires unique management. Holospinal imaging modern aggressive antibiotic therapy, and prompt surgical intervention remain the standard of care for all spinal axis infections including HEAs. However, the surgical decision making on timing and extent of the procedure still remain ill-defined for HEAs. We report a patient who presented with rapidly progressive quadriparesis secondary to HEA. He underwent urgent surgical decompression with abscess drainage and arrest of further neurological deterioration. We discuss the surgical management strategies and briefly review the literature regarding HEA.
Keywords: Epidural abscess; Spinal infection; Skip laminectomy; Holospinal epidural abscess
Introduction
Spinal epidural abscess can rarely form throughout the entire spinal canal, an entity known as a holospinal epidural abscess (HEA). HEA can lead to extensive spinal cord compression and devastating neurological consequences if prompt therapies are not provided [1]. Only a limited number of patients with HEA extending from the cervical to the lumbar spine have been reported [2-8]. We describe a patient with HEA that highlight the importance of urgent surgical decompression and discuss the rationale for extent of laminectomy and adjunctive treatment modalities.
Case Report
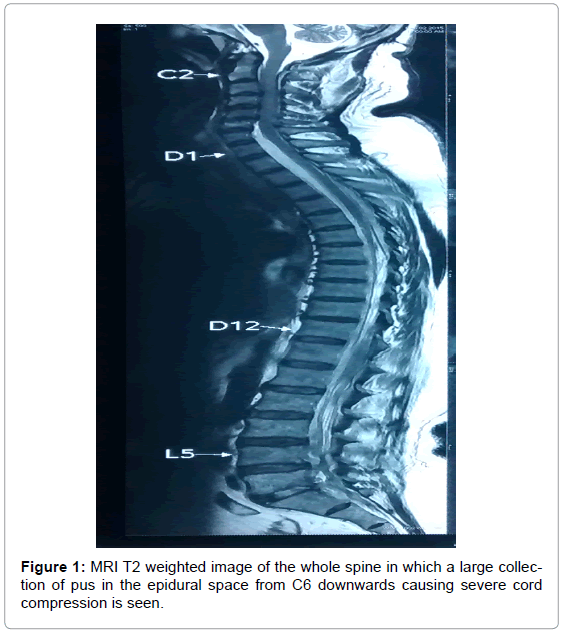
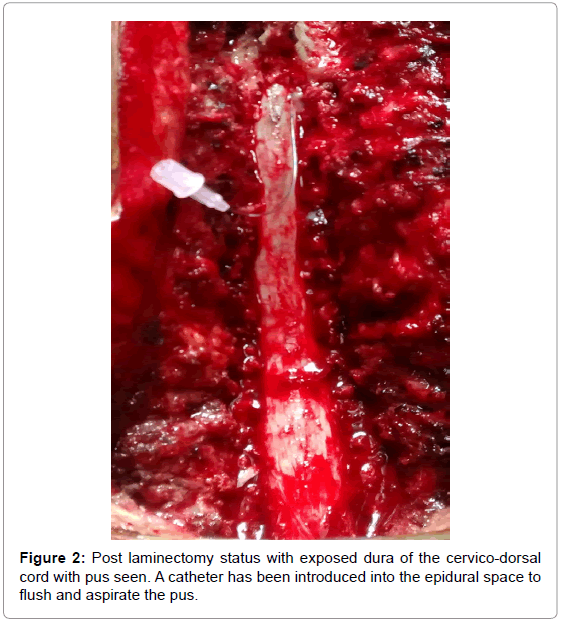
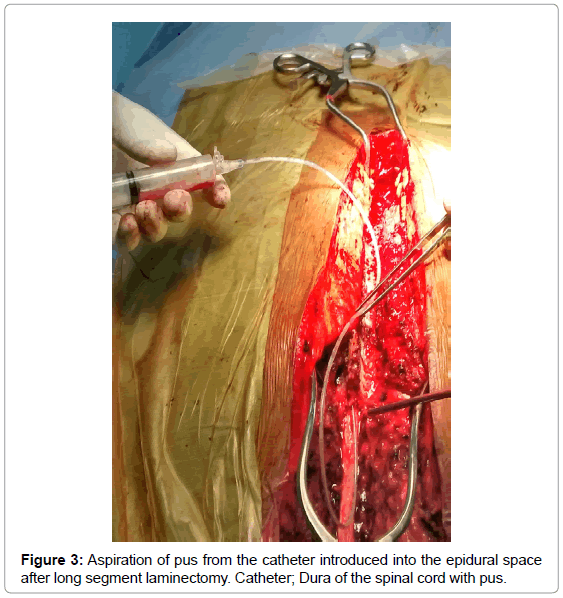
A 50-year-old man, a businessman by profession presented with severe neck and back pain, and rapidly progressing limb weakness in a span of 5 days. He was retroviral (HIV) positive and a diabetic on poor control. Physical examination revealed normal sensorium and flaccid quadriparesis of 1/5 in the proximal and 3/5 in the distal group of muscles in the upper limbs and 1/5 power in both lower extremities. Blood picture revealed leukocytosis and MRI showed HEA extending from C2 to S1 (Figure 1). Spinal cord compression was most severe from C6 to D7 circumferentially. The patient was started on broad spectrum Antibiotics (Meropenam 1 gm thrice daily and Vancomycin 750 mg thrice daily) and underwent urgent surgical decompression with abscess drainage by C2 to D2 cervicodorsal laminectomy and fenestration at L1 unilaterally. There was a granulation noted at cervical level and thick yellowish pus was let out circumferentially from the upper dorsal level through gentle probing all around. 5Fr infant feeding tube was guided downwards from D2 level till L1 and separately from L1 fenestrated site downwards towards the sacrum without any resistance and slowly flushed with gentamycin saline. (Figures 2 and 3) Intraoperative cultures were positive for methicillin-sensitive Staphylococcus aureus (MSSA). He was treated with appropriate antibiotics with 6 weeks of intravenous. There were no complications although no significant improvement immediately. He was gradually weaned off ventilator and started on physiotherapy. After 4 months post-operative follows up, he had good improvement of power up to 4/5 and was ambulant without support (Figures 4a and 4b).
Discussion
Spinal axis infections are increasing in prevalence secondary to increasing numbers of spinal surgeries around the world [9-17]. Modern aggressive antibiotic therapy and supportive care have improved outcomes in certain patient populations who have an epidural spinal infection [15,18,19] spinal epidural abscesses were first reported by Morgagni in 1761. Fewer than 25 case reports of HEA have been published in the past 25 years [20,21]. Spinal infections are a serious health care dilemma occurring in patients with immunodeficiencies, ongoing known infections, and intravenous drug abuse [16]. Epidural abscesses are especially high-risk infections because neurological deterioration can occur rapidly. Nearly 30% of spinal epidural abscesses do not have a specific source; however, studies estimate that nearly half are from hematogenous seeding, whereas 10% to 20% originate from osteomyelitis, hematoma, or soft-tissue infection, and 20% are iatrogenic [18,19]. In these cases, arteritis, venous thrombosis, or septic thrombophlebitis leading to spinal cord infarction have been found post-mortem, representing the most likely causative mechanism for neurological deterioration [22] HEA affects patients of all ages [3,7,8] and should be suspected in high risk patients with back pain, fever, and/ or neurological deficits [12]. Our patient had underlying risk factors for HEA (age and retroviral positive). The most important aspect in deciding a role for surgery is the neurological examination. Nearly 20% were treated successfully with medical therapy alone if neurologically intact. None of the reported cases had an associated cranial infection with HEA, because the dural adhesion around the foramen magnum prevented rostral spread of infection. Traditionally a posterior approach to the epidural space with irrigation is performed, unless an extensive focal ventral collection is causing cord compression. Surgical intervention for HEA should be an adjuvant treatment strategy for all acutely deteriorating patients, whereas aspiration of other infected sites like a psoas abscess can determine an infective pathogen, and appropriate antibiotic treatment may avoid surgical intervention in the neurologically intact patient. Timely diagnosis and proper treatment of HEA are critical in preventing catastrophic neurological consequences from spinal cord compression. Whole spine MRI with contrast should be obtained if HEA is suspected; CT imaging is unreliable [13] Homogeneous enhancement on T1- weighted sequences obtained with Gd, and hyper intensity throughout the lesion on T2-weighted sequences is more consistent with granulation, whereas bright rim enhancement with a hypointense core on T1-weighted images is suggestive of liquid pus. Blood cultures are essential in early pathogen identification and are positive in up to 60% of cases [3]. Extensive psoas abscesses and contiguous soft-tissue infections are also well described. In most cases HEAs are associated with S. aureus infections, with no predisposition for age or an immunocompromised state. Broad-spectrum intravenous antibiotic is the standard treatment for spinal epidural abscesses, but in the setting of a deteriorating neurological examination surgical intervention is warranted. In the deteriorating patient with HEA, steroids remain controversial, and further research is necessary to elucidate their efficacy [3]. The two principal decompresive methods to treat HEAs are segmental laminectomies with catheter irrigation [7,12] or radical laminectomy of the entire spinal column [9]. We performed segmental cervicodorsal laminectomy with a small fenestration on the left side at L1 followed by catheter irrigation. There are no clear data regarding whether or not implants should be used in the setting of active infections. However, we decided not to use implants at this stage as it would prolong the duration of surgery, blood loss and add to the risk of already existing clinical status. HEA can result in rapid neurological decline and even death. Simpson et al. describe a patient in which a C2–S2 HEA resulted in death; as the patient was being prepared for surgery, he rapidly became quadriplegic, deteriorated, and died of cardiopulmonary arrest [22]. Actually, similar episode happened to our patient when he was admitted in another hospital before and hence the surgery was deferred. However, most patients with significant preoperative neurological deficits have good outcomes with proper management [7,8,12].
Conclusion
HEA can result in rapid permanent neurological injury and even death. Timely diagnosis and treatment are essential. HEAs of the spinal axis lesion or signs of inflammation such as spinal cord signal changes or edema on MRI studies are red flags, and early surgical evacuation should be considered regardless of neurological status. In the presence of a deteriorating neurological exam, surgical decompression via posterior segmental laminectomies and catheter irrigation of the epidural space is efficacious, safe and outcomes are promising.
Citation: Ganapathy S, Venugopal S (2019) Holospinal Epidural Abscess – A Surgical Perspective. J Neuroinfect Dis 10: 289. DOI: 10.4172/2314-7326.1000289
Copyright: © 2019 Ganapathy S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3045
- [From(publication date): 0-2019 - Sep 04, 2025]
- Breakdown by view type
- HTML page views: 2224
- PDF downloads: 821