Hydatidosis of the Pelvis: Six Cases and Review of the Literature
Received: 18-Mar-2019 / Accepted Date: 16-Apr-2019 / Published Date: 23-Apr-2019 DOI: 10.4172/2332-0877.1000399
Abstract
Bone hydatid disease is a rare, even in endemic areas like Morocco. There are no parallels between the often poor clinical and extensive anatomical lesions, thus explaining the delay in diagnosis. Our retrospective study of 6 cases of hydatid disease of the collected basin traumatology-orthopedic department at Ibn SINA hospital RABAT on 7 years duration, leads to a number of conclusions; these 6 cases illustrate the rarity of the disease, even in countries considered endemic. It is a disease of adults, given the clinical latency characteristic of this condition. The average age of our patients was 38 years with a male predominance. Paraclinical explorations have benefited from technological advances in 2 levels, the diagnosis with sero-immunological reactions increasingly sensitive and specific, a staging with the addition of ultrasound, CT and MRI. Diagnosis is difficult despite modern means of investigation and only the pathological examination to confirm the diagnosis. Treatment is primarily surgical. Given the delay in diagnosis and the difficulties of the radical surgical care, recurrences are common, and the prognosis is unfortunate. In the end, we must emphasize the role of a scheduled prophylaxis and organized nationally for the eradication of the disease.
Keywords: Hydatidosis; Pelvis; Diagnosis; Therapeutic approach
Keywords
Hydatidosis; Pelvis; Diagnosis; Therapeutic approach
Introduction
The hydatid disease, or bone hydatid disease, is a parasitic disease caused by the development in humans, accidental intermediate host for the larval form of Echinococcus granulosus, which lives as an adult in the intestine of dogs or other carnivores [1,2]. Bone involvement is rare, accounting for only 0.9 to 2.5% of maps; its frequency is much lower than that of liver maps (60 to 70%) and lung (20-30%) [3-5]. This location has many special features including scalable and pathological and remains asymptomatic long (15-40 years) and the first signs are late.
In the absence of specific clinical and radiological signs, diagnosis is often based on the pathological examination of a piece of surgical resection or percutaneous biopsy. Treatment is medical and surgical, is a complete excision of the lesions. The surgical procedure is often insufficient due to the difficulties to achieve complete excision, and association with treatment with benzimidazoles (albendazole) yielded encouraging results [6].
Case Series
We report in our work 6 cases of primary hydatid disease of the pelvic bones, collected in traumatology orthopaedic department in hospital Ibn SINA RABAT, over a period of 7 years from January 2011 to December 2018. Through this work we will, firstly, remember the epidemiological and clinical data of this disease, various radiological aspects. On the other hand, we will study the different treatment modalities and results. The results of our study will be compared with data from the literature.
Radiological examination included in all cases of plain radiographs, a CT scan in 5 cases. The magnetic resonance imaging was performed in 3 patients. The blood count was monitored for all patients. The hydatid serology, performed in all patients. The definitive diagnosis was always histological.
Our observations are in summary form, together with a summary table summarizing the clinical, biological, radiological, treatment and outcome (Table 1).
| Variables | Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 |
|---|---|---|---|---|---|---|
| Age | 27 | 37 | 25 | 47 | 42 | 30 |
| Origin | Rural | Urban | Urban | Rural | Rural | Rural |
| Antecedents | Contact with dogs | Contact with dogs, liver in KH brother | -- | Contact with dogs | Contact with dogs | -- |
| Clinical signs | Swelling right gluteal | Sciatica lameness fistula | Fixed buttock pain, lameness | Chance discovery during a basin Rx | Chronic pain facing the left iliac wing | Limping right with pain on exertion. |
| Rx basin | Bone loss | Bone loss | Bone loss | Bone loss | Bone loss | Bone loss |
| CT | Images Multi geodic sacrum and sacroiliac | Image Multi geodic extended the sacroiliac and soft tissue of the pelvis. | Important osteolysis of the acetabulum and the upper end of the femur | -- | Osteolysis of images associated with cystic hypodense collections of the left iliac wing | Pictures of osteolysis of the acetabular cup |
| MRI | Mass multi cystic iso signal T1, T2 hyperintensity | Multi cystic expansive process | -- | Multivesicular cystic pictures | -- | -- |
| Eosinophilia | 1% | 3% | 2% | 1% | 4% | 3% |
| VS mm/h | 40 | 120 | 25 | 60 | 10 | 90 |
| CRP mg/l | 40 | 188 | 30 | 5 | 6 | 8 |
| Hydatid serology | Negative | Positive | Positive | Negative | Positive | Positive |
| Maps | Sacrum and sacroiliac joints | Sacrum, sacroiliac joint soft parts | Acetabular cavity right femoral head | Left iliac wing | Left iliac wing | Acetabular cavity |
| Treatment | 1st time: curettage biopsy 2nd time: excision of the cyst | No indication for surgery (extensive lesions of the pelvis) Albendazole 800 mg/d | Biopsy-resection chirurgical- Albendazole 800 mg/d | Biopsy-resection chirurgical- Albendazole 800 mg/d | Albendazole 800 mg/d-denial of all surgical treatment | Biopsy-Albendazole 800 mg/d-denial of all surgical treatment |
| Evolution 2 years | Fistulisation chronic infection, amputation of the hemi-pelvis refused by the patient | Fistulisation, lesions without bone reconstruction stabilization sign | Ossifying abscess | Clinical improvement functional biological recurrence-No | Clinical improvement functional absence of biological recurrence | Decrease in pain with persistent radiological images. |
Table 1: Summary of six observations.
Results
The average age of our patients was 38 years with extremes ranging from 27 to 47 years with male predominance 4 men and two women. The rural background and contact with dogs were the main contributing factors. Several bone lesions have been described by various authors (pelvis, spine, long bones) we focus on locating at the pool found in all patients. The average time of diagnosis was 18 months ± 9.2.
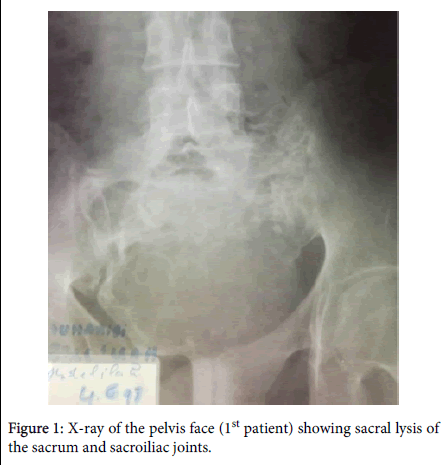
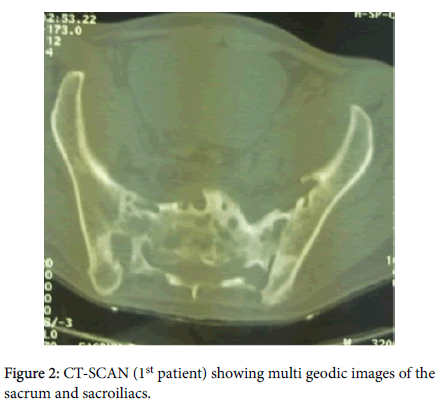
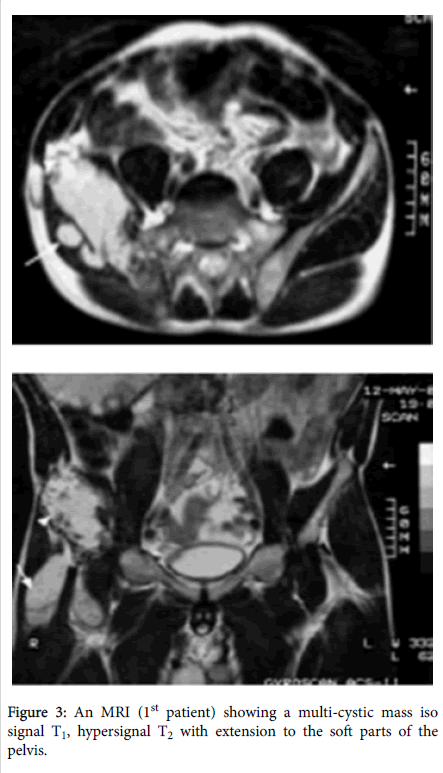
The tell-tale symptoms of bone hydatid cysts are very variable, usually uncharacteristic and appear only after breaking the cortical bone and soft tissue invasion, the general condition is still kept, apart from cases of superinfection. In most cases the call signs are represented by: buttock pain (2 cases), swelling (1 case), functional disability and lameness (1 case), discovered incidentally during a pelvic radiograph (1 case), radicular symptoms (1 case). The general condition was preserved in all cases. Plain radiographs were shown confluent gaps of varying size, poorly defined, multilocular often separated by internal partitions embodying the aspect "grape cluster" or "honeycomb" (Figure 1). CT was objectified bone lesions result in lacunar images hypodense of variable size and shape, limited, not undergoing change after injection (Figure 2). The abdominal pelvic ultrasound was done in none of our patients, has been replaced by MRI that showed cystic images hypo signal on T1-weighted images and hyper signal on T2-weighted images (Figure 3). The latter allows a better analysis of soft tissue showing girls vesicles and indicating the extent length of the lesion. No visceral localization was found in the general staging. The chest radiograph was normal in all cases. The erythrocyte sedimentation rate was accelerated in all cases. CRP was elevated in 3 cases and normal in 3 cases. The eosinophilia was normal in 4 cases. The hydatid serology was positive in 4 patients and negative in 2 patients.
The treatment was essentially surgical radical resection of the mass of most oncological as possible has been made for three patients, conservative curettage lesions for a patient. We refrained from operating on a patient because of the extensive damage to the sacroiliac region with significant expansion in nerve and arterial structures of the pelvis. One patient refused any surgery. Every patient received medical treatment 6 weeks before and after surgery by Albendazole 800 mg/d.
At a mean of 2 years, the outcome was favourable in 2 patients treated radically, marked clinical improvement, organic and functional. This trend was also embroiled with complications and recurrences. Recurrence fistulising and suppuration in a patient whose lesions had spread and whose resection could not be oncological, the response time was 8 months. The appearance of an abscess ossifying in the patient treated by curettage. A decrease in pain with persistent radiological images.
Discussion
Hydatid disease affects all organs but predominant liver and lung. It is favored by poor sanitation and promiscuity with the dog and sheep [7-10]. It is endemic state especially in South America, Australia but also in the Mediterranean basin and in Central Europe. It essentially rampant in rural areas. The rural origin is found in 4 of our patients. However, Bone location of this condition is rare; it represents 0.9 to 2.5% of all hydatid maps. It is recognized that this location is primitive and not of continuity or spread [2,8,9]. Because of its slow evolution, it is the most common among adults. The incidence rate was 10.7 per 100,000 men, and Morocco is among the countries that have a very high prevalence of hydatid 7.2 per 100,000. The literature reports the notion of adulthood in the bone hydatid disease patients; with an average that varies between 30 to 35 years. This is true of all our patients who have an average age of 38 years with extremes of 27 and 47 years. There appears to be no sex predominance in the literature. Our results predominantly male. Conventionally predominates to the vertebral level above all dorsal [7], exceptionally cervical [11-14]. In most cases, it remains isolated, not joining in about 30% cases of hydatid cysts of other organs [12,15-18]. In our series, no patient had associated visceral localization.
Bone echinococcosis is characterized by its clinical latency. Some authors have shown that a dozen years of evolution were necessary for bone disease manifests itself, which explains the importance of the lesions and the frequency of complications at diagnosis. The tell-tale symptoms of bone hydatid cysts are very variable (pain, local swelling, pathological fracture), usually uncharacteristic and appear only after breaking the cortical bone and soft tissue invasion, the general condition is still kept in apart from cases of superinfection [11,12].
Biological methods are of great importance and can quickly direct the diagnosis, and these reactions allow postoperative surveillance Negativity of these examinations do not eliminate the diagnosis [1]. The hyper eosinophilia is neither specific nor constant presence towards a parasitic disease, it is often moderate in the third case, it is less than 5% [3]. It is of interest only when the rate is greater than 7%, and this in all locations [16]. An ascent of eosinophilia reflects the cracking or breaking of the cyst, while its disappearance demonstrates its superinfection or its calcification [1,3]. Its absence does not eliminate the diagnosis. Immunology whether to target cell (casoni intradermal reaction) or humoral (revealing immune-electrophoresis arcs characteristics, particularly arc 5, the reaction of hemagglutination, immunofluorescence) is a great extra but often defect [3]. These immunological tests are also useful in the postoperative surveillance. Diagnosis of the disease is often difficult and only the histological examination of a piece of surgical resection or percutaneous biopsy can confirm [1].
Hydatid disease seat usually the iliac wing and translates radiologically by multiple clear geodes of variable size, sometimes circular or oval containing receivers and separated by spans, they tend to coalesce. Rarely in less advanced forms a single gap can be seen, worm-eaten, less evocative isolated. The hip disease is three times more common than the iliac-sacral and pubic rami. Branches or iliac ischio-pubic, typical image can be seen in "honeycomb" The image of osteolysis is the most characteristic of the bone hydatid picture in our study this is found in patients [13-15].
The results of a bone hydatid disease must have at present in addition to the ultrasound research other hydatid lesions, direct ultrasound lesions, it can help to positive and topographic diagnosis when the anatomical conditions permit, it can show a collection of fluid appearance pure or mixed multi partitioned recall a visceral hydatid cyst [5]. The ultrasound diagnosis is difficult when the cysts contain loose debris or that their content is thick, purulent. The absence of fluid structure does not formally exclude the diagnosis. Merkle [18] emphasizes the value of this technique, not only for diagnosis, but also in the damage balance sheet expansion in the soft parts and in monitoring disease progression postoperatively.
The CT is the examination of choice because it offers the advantage of its safety and accuracy of the information it provides. This technique has greatly changed the management of patients, indicating bone damage. These bone lesions result in patchy hypodense images of variable size and shape, more or less limited, not undergoing change after injection. MRI is complementary to CT scan. It is the examination of choice, especially for spinal and pelvic locations. It shows cystic images hypo signal on T1-weighted images and hyperintense on T2-weighted images. It allows better analysis of soft tissue showing girls vesicles and indicating the extent length of the lesion (1.16).
Surgical treatment should be almost oncologic because tapeworm an evolution that is reminiscent of a malignant tumor is invasive [19]. But surgery is usually incomplete, which explains the almost constant relapse. Therefore, some authors stress the interest iterative interventions practiced systematically before any signs of clinical or radiological progressive recovery (1.9). Sterilization of the parasite and the protection of the operative field are obtained by the use of a scolicide such as formalin, hypertonic saline and hydrogen peroxide. This has multiple benefits, steady and rapid efficiency on scolex, Ease of Use, Low Cost, High availability. These advantages make the hydrogen peroxide scolicide choice. Postoperative monitoring must be rigorous and extended to detect any recurrence (30 to 40% of cases). This monitoring will be done best on the imaging plane by CT or MRI if possible and biologically by hydatid serology [20,21].
Albendazole is currently the most effective imidazole although its effect is far from constant. Garcia-Vicuna [21] found 80% improvement or healing, however, Bonifacino [20] found no efficacy in this location. In our series we see 50% improvement under treatment with Albendazole. Medical treatment may be associated with surgery as pre-surgical prophylactic treatment in order to reduce the fertility of cysts and prevent the spread, for breach of fertile cysts. It is six weeks of continuous treatment before surgery, and more effective in the serous locations, liver and lung. Post-surgical treatment or treatment with curative referred avoids recurrence and is three treatments depending on the clinical course, radiological, and tolerance of treatment [19].
The radical solution to the inter-iliac abdominal disarticulation is sometimes necessary without putting the patient immune to relapses. This disarticulation is a mutilating surgery, debilitating and should be discussed in the case of advanced damage in elderly patients or those with defects. So what in the subject Young, conservative treatment is best. Curettage interventions are the cause of recurrence and reoperation without results [6,7].
During its evolution, either spontaneously or after puncture or surgery, a secondary infection of the lesions can occur. This infection can cause serious general complications and caused locally microbial chronic osteitis superimposed. According DEVE, this microbial osteitis may be, next to its adverse effects, causing a lesion osteosclerosis may oppose to some extent to the bone echinococcosis. Generally, evolution is irreversible and fatal. Thus, DEVE himself, attributes the "white cancer" bone hydatid disease [4].
Conclusion
Treatment can only be surgical. Medical treatment is used as an adjuvant to surgery, sometimes present the only possible over large lesions scattered or difficult to access. Bone hydatid disease is rare, it’s slow and insidious, delaying the discovery of radiological images evocative to any stage or often exceeded the reasonable therapy is what makes the real treatment for this condition, remains in its prophylaxis to be exercised every level of the epidemiological chain.
References
- Briant JF, Richez B, Belil E, Barea D, Raillat A, et al. (1998) Osteoarticular parasitic: Bone echinococcosis. J Radiol 79: 1351-1357.
- Baklouti S, Elleuch MH, Fourati H, Guermazi million Jlidi R, Sellami S et al. (1995) Hydatid cyst bone of the femur about a case of misleading radiological appearance. Sem Paris Hosp 71: 102-105.
- Belzunegui J, Maiz O, Lopez L, Plazaola I, Gonzalez C, et al. (1997) Hydatid disease of bone with adjacent seal involvement: A radiological follow-up of 12 years. Br J Rheumatol 36: 133-135.
- Houyam LSA, Hasna Hassiko AE, Abdelhakim T, Najia H (2003) Bone Hydatidose: A study of 11 cases. Revue Joint Bone Spine 70: 732-735.
- El-Madhi T, Ameur A, El-Ounani Medaghri J, Boumdin M, Manouar M (1996) Bone hydatidose: Apropos of 10 cases. Maghreb Medical 306: 16-20.
- Zlitni M, Kooli M, Ezzaouia K, Lebib H, Mestiri M (1996) Bone lesions parasitoses, musculoskeletal. Encycl Med Chir Elsevier (Paris), pp: 5.
- Franceschi JP, Curvale G, Noca P, Roux H (1991) Hydatid cyst of the basin About a case followed over 8 years. Joint Bone Spine 58: 211-213.
- Campoy E, Rodriguez-Moreno J, Del Blanco J, Â Narvaez J, TRoig Escofet CD et al. (1995) Hydatid disease, An unusual case of chronic monarthritis. Arthritis Rheum 38: 1338-1339.
- Baba A, Chaieb A, Khairi H, Keskes J (1991) Epidemiological profile of Pelvic Hydatidosis about 15 cases. J Biol Reprod Gynecol Obstet 20: 657-660.
- Bergaoui N, Ben Hammouda M, Touzi MK (1996) Hydatidose in costal and dorsal epidural location. Rheumatology 48: 207-211.
- Song XH, Ding LW, Wen H (2007) Bone hydatid disease. Postgrad Med J 12: 536-542.
- Akhan O, Dincer A, Saatei I, Gulekon N, Bessim P (1991) A spinal intradural hydatid cyst in a child. Br J Radiol 64: 465-456.
- Karray S, Zlitni M, Fowles JV, Zouari O, Slimane N, et al. (1990) Vertebral hydatidosis and paraplegia. J Bone Joint Surg Br 72: 84-88.
- Govender T, Aslam M, Parbhoo A, Corr P (2000) Hydatid disease of the spine. A long-term follow-up after-surgical treatment. Orthop Wink 378: 143-147.
- Sapkas GS, Stathakopoulos DP, Babis GC, Tsarouchas JK (1998) Hydatid disease of bones and joints, followed eight boxes for 4-16 years. Acta Orthop Scand 69: 89-94.
- Keller TM, Schweitzer JS, Helfend LK, Chappell T (1997) Treatment of progressive cervical spinal instability secondary to hydatid disease: A case report Spine 15: 915-919.
- Merkle EM, Kramme E, Vogel J, Kramer S, Schulte H, et al. (1997) Bone and soft tissue manifestations of alveolar echinococcosis. Skeletal Radiol 26: 289-292.
- Baykaner MK, Dogulu F, Ozturk G, Edali Tali N (2000) A viable TA residual spinal hydatid cyst cured with albendazole Case report. J Neurosurg 93: 142-144.
- Bonifacino R, Dogliani E, Craig PS (1997) Albendazole treatment and serological follow up in hydatid disease of bone. Int Orthop 21: 127.
- Garcia Vicuna R, Carvajal I, Ortiz-Garcia A, Lopez-Cobledillo AD, Laffon A, et al. (2000) Primary solitary echinococcosis in cervical spine: Postsurgical successful outcome long-term after-albendazole treatment. Spine 15: 520-523.
Citation: Sabri EM, Omar L, Reda FM, Boufettal M, Basir RA, et al. (2019) Hydatidosis of the Pelvis: Six Cases and Review of the Literature. J Infect Dis Ther 7: 399. DOI: 10.4172/2332-0877.1000399
Copyright: © 2019 Sabri EM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3737
- [From(publication date): 0-2019 - Oct 12, 2025]
- Breakdown by view type
- HTML page views: 2832
- PDF downloads: 905