Improving Sustainment of Weight Loss: Implementation of Motivational Interviewing in a Retail Health Setting
Received: 15-Oct-2022 / Manuscript No. JOWT-22- 77309 / Editor assigned: 17-Oct-2022 / PreQC No. JOWT-22- 77309 (PQ) / Reviewed: 19-Nov-2022 / QC No. JOWT-22- 77309 / Revised: 23-Nov-2022 / Manuscript No. JOWT-22- 77309 (R) / Published Date: 30-Nov-2022 DOI: 10.4172/2165-7904.1000526
Abstract
Objective: The aim of this quality improvement project was to implement the use of motivational interviewing in the retail health setting to achieve quality patient outcomes. The use of motivational interviewing was to provide a comprehensive method to address nutrition, diet, exercise, sleep, and medication adherence. The overall goal of the quality improvement measure was to identify a larger amount of weight loss for patients in a 3-month period, decreased waste circumference, and increased patient satisfaction with provider interactions, improved blood pressure readings, and overall sustainment of weight loss.
Method: Dorothea Elizabeth Orem’s self-care theory of nursing was utilized as the conceptual framework for facilitating sustained weight loss in the retail health setting. Motivational interviewing and peer coaching were the interventions being integrated to further improve lifestyle choices. The acronym FRAMES (Feedback, Responsibility, Advice, Menu, Empathy) was utilized as a method to guide discussions throughout patient encounters.
Results: The findings from the QI project did confirm that the use of motivational interviewing had a positive influence on overall weight loss and waist circumference. There was not a significant difference in the systolic or diastolic blood pressure measurements or overall BMI. There were a total of 36 patients that did not follow up for three consecutive visits. This group consisted of 7 males and 29 females. The racial breakdown of this group was 17 Caucasians, 14 African Americans, 4 Native American, and 1 Hispanic. The group that did not follow up as instructed had lower readiness for change results. This implies that those patients that arrive to the clinic motivated to adopt healthy lifestyle behaviors are more likely to remain committed to the program.
Conclusions: This quality improvement project serves to inform community leaders and stakeholders about the prevalence of obesity, devastating costs, and negative impact on population health. An evidence-based tool of motivational interviewing has been implemented as a solution to the epidemic of obesity. Collaborative efforts between key stakeholders, community leaders, schools, and churches are imperative to combat this problem. Based on the review of literature, low economic cost to implement this quality improvement measure, and patient benefits, motivational interviewing should be adopted by outpatient and inpatient providers.
Keywords
Motivational Interviewing; Obesity; Retail Health; Dorothea Orem’s Self-Care Theory; FRAMES Technique
Introduction
Obesity is a complex, multifactorial, and largely preventable disease that increases the risks of a range of diseases for adults. This includes higher rates of complications and serious illness from COVID-19, as well as type 2 diabetes, high blood pressure, heart disease, stroke, arthritis, depression, sleep apnea, liver disease, kidney disease, gallbladder disease, pregnancy complications, infertility, many cancers, and overall mortality [1]. Obesity and its repercussions constitute an important source of morbidity, impaired quality of life, and its complications can have a major bearing on life expectancy [2]. North Carolina has the 20th highest adult obesity rate in the nation, while ranking 12th in the nation for diabetes and 13th in the nation for hypertension, both of which are considered obesity related diseases [3]. Although public awareness has increased concerning obesity, nearly two-thirds of Americans are overweight or obese [4]. An estimated 45 million Americans go on diets annually and spend $33 billion on weight loss products [4]. Nationally, as few as 5% of those individuals will maintain the weight loss long-term [4].
At the Retail Health Clinic (RHC), the overall initial success rate of losing weight is high, but the sustainment of weight loss after 3 months is low. RHC is located within the southeastern portion of North Carolina. It is privately-owned by a Family Nurse Practitioner (FNP) and Pharmacist which oversee the daily operations for the clinic and pharmacy. This clinic meets the designation as a retail health center or convenient care clinic because it is a health center within a retail store or pharmacy. At urgent care clinics, at least one board-certified physician must legally be on staff; however, at retail health clinics they typically staff the clinic with an FNP, Physician Assistants (PA), and/or a Medical Doctor (MD).
Retail health clinics are not appropriate for managing urgent problems or life-threatening issues. They provide services focused on treating minor illnesses, dermatologic disorders such as acnes or rashes, preventative services which include immunizations, school physicals, Department of Transportation (DOT) physicals, and weight loss [5]. Convenient Care is a patient-centric model of healthcare committed to high quality, easy access, affordable healthcare, and acts as a trusted and integrated partner in the healthcare system [5]. Since the first retail health clinics were established in the industry almost twenty years ago, there has been an increased establishment of locations by major business chains such as CVS Clinic, Rite-Aid, Walgreens, and Target as well as independent owners. CCA estimates there are over 2,000 retail health clinics nationally.
Problem Description
The Center for Disease Control and Prevention (CDC) [6] defines obesity as having a weight that exceeds a healthy weight based on height. Body mass index (BMI) may be calculated using the following formula: BMI=kg/m2 where kg is a person’s weight in kilograms and m2 is their height in meters squared [6]. BMI is performed as a screening tool to determine if an individual is underweight (BMI below 18.5), normal weight (BMI 18.5- 24.9), overweight (BMI 25-29.9), Class 1 obesity (BMI > or equal to 30-34.9), Class 2 obesity (BMI > or equal to 35-39.9), and Class 3 obesity (BMI > or equal to 40) [6].
The prevalence of obesity has been closely monitored and researched by the World Health Organization (WHO) due to its pervasive nature. Internationally, it has nearly tripled between 1975 and 2016 (WHO) [7]. In 2016, more than 1.9 billion adults worldwide (13%, 11% of men and 15% of women) were overweight with 650 million of these being obese [7]. Estimations predict that by 2030 an estimated 38% of the world’s population will be overweight and 20% will be obese [8].
Approximately one-third of the National population (almost 40%) is obese [5]. When looking at population health, obesity affects some groups more than others. In the United States, Hispanics (47%) and non-Hispanic blacks (46.8%) had the highest age adjusted prevalence of obesity, followed by non-Hispanic whites (37.9%), and non-Hispanic Asians (12.7%) [5].
Obesity is growing at alarming rates and significantly impacts communities within the state of North Carolina [3]. North Carolina’s current obesity rate is 32.1%, up from 20.9% in 2000, and 12.3% in 1999 [3]. The most recent obesity statistics in North Carolina are comparable to the National average. Within the Tarheel State, the prevalence of obesity decreases in the western portion of the state and drastically increases the farther east one travels [3]. For example, Buncombe County in the western mountain region of the state has an obesity rating of 23% which is significantly lower than Cumberland County’s obesity rating of 31.1% [9].
When taking a closer assessment of the population health in Cumberland County, which is in the southeastern section of the state, in 2017 the State of the Health Report, identified obesity as one of the top three priority health concerns of the area [10]. In 2017, Cumberland County’s adult obesity rate of 31.1%, Was slightly lower than the state and National prevalence rates [3]. Adults in Cumberland County aged 45-64 years had the highest rates of obesity at 38.2%, then adults aged 26-44 with a rate of 33.4% [3]. Older Adults 65 and older had the 3rd highest obesity rate of 30.3% and the age group with the lowest obesity rate was in the 18-25-year old group at 15.6% [3]. North Carolina (NC) paralleled the nation with obesity rates in women being higher than their male counterparts, at 33.8% and 30.5% [3].
The African American population in Cumberland County had the highest obesity rate at 41.1%, with Caucasians at 29.3%, and the Latino population with the lowest rate at 28.3% [3]. These staggering statistics demonstrate the magnitude of this problem in the geographical area.
The prevalence of obesity identified within the population of Cumberland County is directly associated with the development of the following chronic conditions: diabetes, heart disease, hypertension, arthritis, and cancer [3]. Some factors contributing to obesity in this population are physical inactivity and a lack of access to exercise opportunities [11]. The correlation between obesity and chronic comorbid conditions has been consistently reported in the literature. According to the State of Obesity [3], 11.4% of adults in Cumberland County have diabetes. In 2014, 81.4 per 100,000 of females and 100.4 males died from this disease [12]. Based on these critical findings, there is a tremendous need for quality improvement measures which decrease the incidence of obesity and lead to sustainment of weight loss.
Obesity related conditions include heart disease, stroke, type 2 diabetes, and certain types of cancers, which are some of the leading causes of preventable and premature deaths in the United States [13].
Most recently, data has confirmed that obesity is a strong indicator of Covid-19 outcomes. Available studies now confirm that Covid-19 cases suggest that risks of hospitalizations, intensive care unit admission, invasive mechanical ventilation, and death are higher with increasing BMI [14]. Due to the overwhelming burden and development of chronic disease states, a 2021 study found that obesity accounted for $170 billion in higher medical costs annually in the United States which includes additional costs in Medicare and Medicaid programs [15].
When looking at population health, obesity affects some groups more than others. In the United States, Hispanics (47%) and non-Hispanic blacks (46.8%) had the highest age adjusted prevalence of obesity, followed by non-Hispanic whites (37.9%), and non-Hispanic Asians (12.7%) [13]. Based on this data, it identifies a racial disparity of obesity within the Hispanic and non-Hispanic black populations.
Literature Review
A review of literature was completed to identify the impact of motivational interviewing on weight loss in the outpatient setting. While conducting a review of the literature, most of the articles addressed barriers to weight loss and the poor health outcomes associated with obesity. In an article by Banerjee ES, et al., [16], a mixed-method study was conducted of low-income African American women who were obese. African American women are disproportionately impacted by obesity [16]. The use of motivational interviewing was monitored through the electronic med. l record system. The study suggested that motivational counseling may be a factor in promoting successful weight loss in low-income, African American Women [16].
The use of electronic health communication is an emerging use of technology which permits health care over the internet. In a quasi-experimental study, motivational interviewing was cited for the positive benefits on patients pursuing weight loss. Motivational interviewing was available electronically. The focus of the study was the integration of motivation interviewing via the internet to promote positive behavioral changes and increased physical activity. Patients that were a part of the “My Plan 1.0” had positive effects on physical activity and weight loss [17]. Physical inactivity is one of the major risk factors for poor health and contributes to obesity [17].
The main challenge of obesity treatment is not weight loss, but long-term weight loss maintenance [18]. This clinical issue has been consistently identified at the RHC. Patient barriers to weight loss described repeatedly in the literature include lack of motivation and readiness for change [19]. A comprehensive patient-centered approach, which includes motivational interviewing, is beneficial towards the achievement of sustained weight loss and lifestyle changes [19]. The article proposes an evidenced-based tool with principles, strategies,and motivational interviewing which incorporate using the 5 A’s (Ask, Advise, Assess, Assist, and Arrange) throughout patient encounters [19]. This adapted interview model is a meaningful addition into a collaborative and therapeutic relationship between the provider and patient that allows directed conversations tailored to address physical, psychological, and environmental obstacles that lead to increased adherence to lifestyle modifications [19].
Stelter R [20] described a single case study analysis of a coaching intervention with a focus on weight-loss which was conducted over 10 sessions throughout a period of 17 months. The client from the case study was a well-educated female that had attempted weight loss on numerous occasions with minimal to no lasting effects. The summary of positive results was not only inclusive of a 12 kg weight loss, but a reported improved mindfulness, increased physical activity, greater focus, and self-empowerment to make better decisions.
Prior to implementing motivational interviewing in both articles, providers had to be educated on what would be addressed in the encounters. Time constraint is a reoccurring challenge confronted by providers. The 5 A’s is a time-efficient model that is easily adaptable to a comprehensive examination or simplified to meet the time constraints of a focused interview [19]. Nurse practitioners are in a unique position to offer first-line assistance with weight loss management. Implementing the use of motivational interviewing at RHC could have a positive influence on how we approach weight loss, enhance patient satisfaction, and improve sustainment of weight loss.
Rationale
As people pursue strategies to achieve effective weight loss, one of the ongoing challenges experienced by patients is the ability to sustain weight loss. Dorothea Elizabeth Orem’s self-care theory of nursing can be utilized as the conceptual framework for facilitating sustained weight loss in the retail health setting. Dorothea E. Orem is one of America’s most influential nursing theorists that have shaped how we define nursing roles and changed our approach to clinical practice issues. The major concepts of this theory will be further explored in this formal report. Motivational interviewing and peer coaching are the interventions being integrated to further improve lifestyle choices.
Orem formulated her concept of nursing in relation to selfcare as part of a study on the organization and administration of hospitals, which she conducted at the Indiana State Department of Health. Orem used both philosophical and scientific methods in developing her insight and conclusions pertaining to the theory. Her major theoretical contributions and assertions were validated based on extensive empirical evidence. Her views are widely embraced by the nursing community. The central idea of the theory of self-care deficit is an abstract concept that, when expressed in terms of action limitations, provides guides for the selection of methods for helping and understanding patient roles in self-care. Orem labels her self-care deficit theory of nursing as a general theory composed of the following three related constituent theories:
The theory of self-care: which describes why and how people care for themselves. It is foundational to the others, expresses the purpose, methods, and outcome of taking care of self. There are five concepts embedded within Orem’s self-care theory. They include self-care, selfcare agency (ability to care for oneself and regulate their own human functioning), self-care requisite (These self-care requisites exist for persons who are ill or injured, who have specific forms of pathological conditions or disorders, including defects and disabilities, and who are under medical diagnosis and treatment. This is required for self-care to occur.), basic conditioning factors (socioeconomic, water, air), and health (primary goal).
The theory of self-care deficit: which describe and explains why people can be helped through nursing? It further provides the reason a person may benefit from nursing.
The theory of nursing systems: which describe and explains relationships that must be brought about and maintained for nursing to be produced? It is identified as the unifying theory and includes all the essential elements.
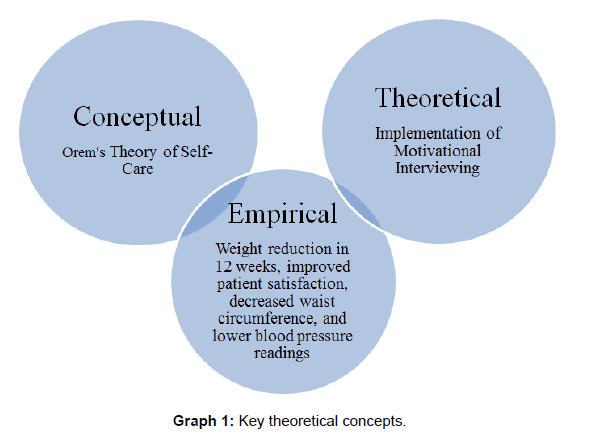
Key concepts of the theory can be utilized as the foundation for facilitating sustained weight loss in the retail health setting. Millions of patients seek assistance with weight loss programs daily; however, sustainment of weight loss efforts is often challenging. Self-care is a learned behavior that is done voluntarily to achieve or maintain health. Some of the barriers to achieving weight loss that have been verbalized by patients at RHC include lack of support, limited time to follow up in the clinic, diet recommendations are unreasonable, costs, and overeating provides an outlet for stress relief or boredom. By assisting patients with the adoption of more favorable self-care choices, sustainment of weight loss will become more obtainable (Graph 1).
The primary barrier identified by healthcare providers surveyed in the retail health setting includes the inconsistency of follow up and ability to connect with patients. When patients seek assistance with weight loss, they are encouraged to return weekly. This enables providers to review meal tracker sheets, discuss progress, or potential hurdles. Unfortunately, some patients will enter the clinic initially and receive prescription medications to assist with weight loss; however, follow up is often less than optimal. Respectively, patients should return weekly for consultation. Based on a review of approximately fifty charts, patients that followed up weekly in our retail health clinic achieved a greater overall weight loss and sustained it throughout the 3-month program. Orem’s theory is an ideal model for empowering patients to take an active role in their weight loss process.
Specific Aims
The aim of this quality project (QI) is to implement the use of motivational interviewing in the retail health setting to achieve quality patient outcomes. The use of motivational interviewing will provide a comprehensive method to address nutrition, diet, exercise, sleep, and medication adherence. The overall goal of the QI measure will
be a larger amount of weight loss for patients in a 3-month period, decreased waste circumference and increased patient satisfaction with provider interactions, improved blood pressure readings, and overall sustainment of weight loss. Through improved self-care measures and a reduction in weight, this will have a profound long-term impact on morbidity and mortality associated with obesity.
Context
This project took place at a Retail Health Clinic (RHC) in southeastern North Carolina. This clinic serves approximately 120 patients weekly seeking treatment for minor acute care conditions, primary prevention, and weight loss. Approximately 60% of those visits are designated to weight loss. There was a total of three providers that solely managed the clinic, all of which are Family Nurse Practitioners (FNP’s), working rotating shifts. Patients were seen during clinic hours on a walk-in basis and designated appointments are not available. The intervention was feasible for the providers and easily integrated into a typical work week. The use of motivational interviewing did not require any special equipment or external resources.
The motivational interviewing was open to all patients desiring weight loss and met inclusion criteria. Participants in the QI project consisted of both male and females, having a BMI of 25 or higher, ages eighteen and older, and English speaking. Eligible participants all received written handouts discussing the quality improvement project.
Resources and Constraints
The RHC was a key stakeholder for this QI project and offered many great resources to facilitate this intervention. The practice has an alphabetized filing system that made the database search for eligible participants both feasible and accessible. The providers were supportive of the QI measure and agreed that it would be beneficial to the overall outcomes of patients. The owner of the clinic allocated a secondary examination room each day for the sole purpose of this project. The RHC offered standard equipment to include blood pressure cuffs, pulse oximeters, digital scales and tape measures for the physical assessment measures. This was helpful in identifying patient progress, making comparisons of findings, and used for the method of evaluation. The Doctoral of Nursing Practice (DNP) student did not incur any additional expenses.
The RHC does not file insurance for weight loss services. It is a cash fee for service for the monthly visit when the prescribing of weight loss medications is involved and could be a potential barrier for patients committing to a consecutive three-month time span. Patients that are only receiving the lipotropic injection and prescribing of weight loss medication is not required, pay a flat rate. Another potential barrier to the implementation of the project was identifying willing participants since the retail health clinic is small and relatively new in operations. This barrier was minimized by using flyer notifications as patients entered and exited the premises. The final potential barrier was participants agreeing to follow up for a total of three visits. This barrier was minimized by completing reminder calls and continuing flexible hours of operation seven days a week for return visits.
Methods
Intervention
Motivational interviewing is a counseling approach developed in part by clinical psychologists William R. Miller and Stephen Rollnick. It is a directive, client-centered counseling style for eliciting behavior change by helping patients to explore and resolve ambivalence [21].
The four general principles of motivational interviewing are to express empathy, develop discrepancy, deal with resistance, and support self-efficacy [21]. The OARS is an acronym for four methods that are used throughout the motivational interviewing process. These are asking open-ended questions, affirmations, reflective listening, and summarizing [21]. The fifth method of motivational interviewing is to elicit change talk for the development of autonomy. This requires some skill level to facilitate through motivational interviewing.
Study of the Intervention
There were various steps required in order to implement the QI project. Staff education was provided by the DNP student during a 2-hour monthly meeting. The motivational interviewing training was adopted from the foundational principles of the Yale Rudd Center for Policy and Obesity using the FRAMES (Feedback, Responsibility, Advice, Menu, and Self-efficacy) criteria. The sample open-ended questions used in the training to prepare for patient dialogue were beneficial. This enabled providers to have a greater understanding of participant’s attitudes concerning weight loss.
Topics discussed during the training included an explanation of the overall purpose for the quality improvement project, goals, methods for integrating motivational interviewing within patient encounters, and most recent organizational, county, state, and national data related to obesity. This additional knowledge and training prepared everyone for necessary proficiency with implementation of the intervention. Providers were reminded to integrate the OARS acronym when communicating throughout patient encounters which reinforced the FRAMES approach to motivational interviewing. The effectiveness of the training was validated by role play demonstration amongst the providers. They were given a hard copy of the FRAMES guidelines for future reference. The example is located in Appendix B of this document. The DNP student was available to answer additional questions by providers and reinforce motivational interviewing training.
Measures
The measurement of the patient outcomes was collected by obtaining blood pressure readings, weight on a standing scale, BMI calculation, and waist circumference. These assessments were obtained in the office at the pre-visit, mid-visit, and post-visit. The findings were used to evaluate the response to motivational interviewing.
Analysis
The t-test is used for the analysis of only two groups; therefore, ANOVA was the preferred method of choice for comparing the three different data sets of pre, mid, and post office visits. The purpose of the analysis was to determine if there was a statistically significant difference (p-value < 0.05), in systolic blood pressures, diastolic blood pressures, waist circumference, standard weight, and BMI at the three separate encounters. The data for this analysis was collected over a 12- week period. Descriptive analysis was conducted by the DNP student to identify associations and differences of the participant’s readiness for change questionnaire results. Due to the high attrition rate, additional descriptive analysis was conducted to compare the nominal data and questionnaire responses of those participants that successfully returned to the clinic for three visits and those that failed to follow up as instructed.
Ethical Considerations
The QI project at RHC required providers to integrate motivational interviewing techniques at each patient encounter. Patient participation included returning to the clinic for three visits and completing a seven-item readiness for change questionnaire. These questions were answered by each participant at the initial visit. The information obtained from the patient was stored in a double locked file cabinet. Each participant was assigned a number, measurements were recorded, and follow up visits were tracked for review purposes.
It is essential that human rights are protected with the implementation of a QI project. Ethical aspects of this project were fully considered prior to the initiation. There were not any specific risks identified with the implementation of this project. RHC did not require separate Internal Review Board (IRB) approval due to the classification as a QI project. All patients signed a general consent form and HIPAA privacy statement the first visit. The DNP student and RHC staff ensured that all patient information was always kept confidential. Participation was voluntary, and patients had the right to decline.
Results
The use of motivational interviewing to sustain weight loss is a quantitative study. The project data was analyzed using ANOVA, Friedman rank sum test, and descriptive statistics.
Non-Parametric
The statistical analysis and compilation of data was completed using Intellectus Statistics (2020). ANOVA was used to compare the blood pressure measurements, waist circumference, BMI, and weight loss at pre, mid, and post office visits. The Friedman rank sum test was conducted to determine whether the medians of the blood pressure measurements were equivalent. There was not a significance in the p-value of systolic blood pressure readings, diastolic blood pressure readings, or BMI. There was statistical difference in the weight, waist circumference, and pre-BMI over the 12 weeks (Tables 1-5).
| Variable | Mean | Standard Deviation |
|---|---|---|
| Pre_Systolic | 125.00 | 8.32 |
| Mid_Systolic | 126.00 | 7.55 |
| Post_Systolic | 125.67 | 7.14 |
Table 1: Systolic Blood Pressure Comparisons (No Significance).
| Variable | Mean | Standard Deviation |
|---|---|---|
| Pre_Diastolic | 80.39 | 6.52 |
| Mid_Diastolic | 81.11 | 7.24 |
| Post_Diastolic | 80.11 | 6.12 |
Table 2: Diastolic Blood Pressure Comparisons (No Statistical Significance).
| Source | df | SS | MS | F | p | ηp2 |
|---|---|---|---|---|---|---|
| Within-Subjects | ||||||
| Within Factor | 2 | 18.10 | 9.05 | 12.02 | < .001 | 0.41 |
| Residuals | 34 | 25.61 | 0.75 | |||
| Df=degree of freedom; SS=sum of squares; MS=mean square; F=ratio of two variances; p=probability; ηp2=partial eta squared | ||||||
Table 3: Waist Circumference Results (Statistical Significance).
| Contrast | Difference | SE | df | t | p |
|---|---|---|---|---|---|
| Pre_BMI - Mid_BMI | 0.53 | 0.12 | 17 | 4.54 | < .001 |
| Pre_BMI - Post_BMI | 0.99 | 0.22 | 17 | 4.58 | < .001 |
| Mid_BMI - Post_BMI | 0.46 | 0.16 | 17 | 2.95 | .023 |
| SE=standard error; df=degree of freedom; t=t value; p=probability | |||||
Table 4: BMI Comparisons (No Statistical Significance; Pre-BMI improved).
| Variable | Mean Rank | χ2 | df | p |
|---|---|---|---|---|
| Pre_Weight | 2.69 | 16.93 | 2 | < .001 |
| Mid_Weight | 1.97 | |||
| Post_Weight | 1.33 | |||
| χ2=chi square; df=degree of freedom; p=probability | ||||
Table 5: Weight Loss (Statistical Significance). Friedman Rank Sum Test.
Discussion
Summary
This QI project aimed to improve the sustainment of weight loss in a retail health setting. During the time of this intervention, a sample size of fifty-four patients was seen and expressed a desire to lose weight. Of the fifty-four patients that were assessed, and questionnaires completed, only eighteen followed up for a minimum of the three encounters as instructed. During the past 4 years at the clinic, there has been a steady increase in the number of patients seeking medical guidance to lose weight. Through the review of medical records, it was determined that less than 10% of patients seen in the clinic are able to sustain weight loss. These findings and poor outcomes were congruent with the national average. The integration of motivational interviewing provided a method for combatting challenges with achieving weight loss goals.
Interpretation
The findings from the QI project did confirm that the use of motivational interviewing had a positive influence on overall weight loss and waist circumference. There was not a significant difference in the systolic or diastolic blood pressure measurements or overall BMI. There were a total of thirty-six patients that did not follow up for three consecutive visits. This group consisted of seven males and twenty-nine females. The racial breakdowns of this group were 17 Caucasians, 14 African Americans, 4 Native American, and 1 Hispanic. The group that did not follow up as instructed had lower readiness for change results. This implies that those patients that arrive to the clinic motivated to adopt healthy lifestyle behaviors are more likely to remain committed to the program. When reviewing the readiness for change questionnaire, the following were identified:
• Question 1: “Do you feel motivated to lose excess body fat at this time?” Of the thirty-six patients, five were somewhat motivated, 17 were quite motivated, and 14 were extremely motivated.
• Question 2: “How motivated are you to change your eating habits at this time?” Of the thirty-six patients, three were somewhat motivated, 28 were quite motivated, and 5 were extremely motivated.
• Question 3: “How motivated are you to increase your physical activity at this time?” Of the thirty-six patients, one patient was not at all motivated, eight patients were somewhat motivated, 21 patients were quite motivated, and 6 patients were extremely motivated.
• Question 4: “How motivated are you to try new strategies/ techniques for changing your dietary, physical activity, and other health related behaviors at this time?” Of the thirty-six patients, eight patients were somewhat motivated, 19 patients were quite motivated, 9 patients were extremely motivated.
• Question 5: “How confident are you that you can devote time and effort, now and over the next few months?” Of the thirtysix patients, twelve patients were somewhat confident, 15 patients were quite confident, 9 patients were extremely confident.
• Question 6: “How confident are you that you will be able to record everything you eat and drink and your movement, most days of the week for 2-4 weeks?” Of the thirty-six patients, one patient was slightly confident, fourteen patients were somewhat confident, 17 were quite confident, 4 patients were extremely confident.
• Question 7: “How satisfied would you be if you achieved a 10% weight loss that significantly improved your health and quality of life?” Of the thirty-six patients, one patient would be slightly satisfied, seven patients would be somewhat satisfied, 16 would be quite satisfied, and 12 would be extremely satisfied.
Limitations
The clinic setting is located within the city limits of southeastern North Carolina. It is considered a relatively new retail health clinic site and opened 4 years ago. One limitation could be due to the lack resources and inability to promote completion of the QI project with compensation. A second limitation is the high attrition rate of 66%. There was a total of fifty-four patients that were seen and completed the initial survey; however, there was only eighteen patients that returned as instructed. Due to the small sample size, generalizations cannot be made to a larger population. The final limitation of the QI project was the brief time span of 12 weeks. By following up with the patients for a longer period of time such as 1-year, additional measurements could be collected to evaluate improvement of health indicators.
Conclusion
This QI project validated that the integration of motivational interviewing with patient encounters has a positive influence on overall weight loss. The continuation of this QI project is uncertain; however, there are many reasons to advocate for its sustainment when considering the detrimental impact of obesity. Unfortunately, there was a high attrition rate identified which could be contributed to the holiday season, unexpected illness, transportation issues, cost, as well as conflicting schedules.
Due to the emergence of Covid-19, it has been a driving force to encourage providers to get creative in how we can address the needs of patients without requiring physical office visit contact. Perhaps providing patient encounters virtually via telehealth platforms would substantially improve attrition. The use of email, phone calls, and text messaging could be additional modes of ensuring patient engagement, especially being sensitive to individuals demanding schedules. A courtesy text message reminder system of a pending follow up appointment could be instituted to also improve overall participation.
In addition to the overwhelming burden of disease, many individuals are confronted with both stigma and discrimination associated with obesity. The threat of fear and perceptions of others pose another potential barrier for sustainment of in-person encounters. Weightbased discrimination can result in measurable and often devastating consequences, including social isolation, mental health disorders, reduced wages, and poorer educational, employment, and health outcomes [22]. These findings serve as a catalyst for more weight-based programs being offered virtually in a private forum and supported by commercial and government funded insurance companies. It is essential for healthcare providers to receive the appropriate training to motivate patients by establishing a rapport to adopt healthy lifestyles. A more comprehensive approach will include behavioral therapy, nutritional counseling, assessment of social needs, exercise planning, and pharmacotherapy prescribing [23].
Finally, an essential option to explore for sustainment of this QI project is obtaining support from key stakeholders. A collaborative effort with key stakeholders focused on reducing the healthcare disparity of obesity is critical to achieving quality health outcomes. Dissemination of quality improvement findings is essential for translation of knowledge. Stakeholders that should be considered for supporting ongoing implementation of motivational interviewing include hospitals, churches, community settings, and civil groups. By developing a strong coalition, this will facilitate continued investment, provide ongoing insight, and assist with combatting the epidemic of obesity.
References
- The State of Obesity: Better Policies for a Healthier America (2022) Special Feature: Food and Nutrition Insecurity Among Youth and Families.
- Abdelaal M, le Roux CW, Docherty NG (2017) Morbidity and mortality associated with obesity. Ann Transl Med 5: 161.
- State of Obesity (2018) The state of obesity in North Carolina.
- Boston Medical Center [BMC] (2019) Weight management.
- Convenient Care Association [CCA] (2018) About our clinics.
- Centers for Disease Control and Prevention [CDC] (2017) Defining adult overweight and obesity.
- World Health Organization [WHO] (2018) Obesity and overweight.
- Xu S, Xue Y (2015) Pediatric obesity: Causes, symptoms, prevention, and treatment. Exp Ther Med 11: 15-20.
- County Health Rankings (2016) Adult obesity.
- Cumberland County Health Department [CCHD] (2017) State of the County Health Report.
- Open Data Network. (2015) Health.
- Institute for Health Metrics (2014) County profile: Cumberland County, North Carolina.
- Centers for Disease Control and Prevention [CDC] (2018) Overweight and obesity.
- Centers for Disease Control and Prevention [CDC] (2021) Obesity, race, ethnicity, and Covid-19.
- Ward ZJ, Bleich SN, Long MW, Gortmaker SL (2021) Association of body mass index with healthcare expenditures in the United States by age and sex. PLoS One 16: e0247307.
- Banerjee ES, Herring SJ, Hurley KE, Puskarz K, Yebernetsky K, et al. (2018) Overcoming obesity: A mixed methods study of the impact of primary care physician counseling on low-income African American women who successfully lost weight. Am J Health Promot 32: 374-380.
- Degroote L, Plaete J, Bourdeaudhuij ID, Verloigne M, Stappen VV, et al. (2018) The effect of the ehealth intervention “My Plan 1.0” on physical activity in adults who visit general practice: A quasi-experimental trial. Int J Environ Res Public Health 15: 1-13.
- Montesi L, El Ghoch M, Brodosi L, Calugi S, Marchesini G, et al. (2016) Long-term weight loss maintenance for obesity: A multidisciplinary approach. Diabetes Metab Syndr Obes 9: 37-46.
- Roberts JL, Standage RP, Olaoye I, Smith LF (2015) Overcoming barriers to weight loss practice guidelines in primary care. J Nurse Practitioners 11: 544-550.
- Stelter R (2015) I tried so many diets, now I want to do it differently: A single case study on coaching for weight loss. Int J Qual Stud Health Well-being 10: 1-13.
- Miller WR, Rollnick S (2002) Motivational Interviewing: Preparing People for Change (2nd edn). New York: The Guilford Press.
- O’Keeffe M, Stuart F, Watts K, Rubino F (2020) Knowledge gaps and weight stigma shape attitudes towards obesity. Lancet Diabetes Endocrinol 8: 363-365.
- DiLillo V, Siegfried NJ, Smith WD (2003) Incorporating motivational interviewing into behavioral obesity treatment. Cogn Behav Pract 10: 120-130.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Swinson C, Hodges S (2022) Improving Sustainment of Weight Loss: Implementation of Motivational Interviewing in a Retail Health Setting. J Obes Weight Loss Ther 12: 526. DOI: 10.4172/2165-7904.1000526
Copyright: © 2022 Swinson C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3339
- [From(publication date): 0-2022 - Dec 09, 2025]
- Breakdown by view type
- HTML page views: 2851
- PDF downloads: 488