Research Article Open Access
In The Aftermath of Cancer: The Psychological Status of Adolescent Cancer Survivors and its Correlates
Carmina Castellano-Tejedor1*, Marta Pérez-Campdepadrós1, Lluis Capdevila1,2 and Tomás Blasco-Blasco2
1Department of Basic Psychology, University of Barcelona, Bellaterra, Spain
2Pediatric Oncological and Hematological Service. Vall d'Hebron University Hospital, Barcelona, Spain
- *Corresponding Author:
- Carmina Castellano-Tejedor
Department of Basic Psychology
University of Barcelona, Bellaterra, Spain
Tel: +34 933 55 6000
E-mail: ninacastej@yahoo.es
Received Date: November 25, 2015; Accepted Date: December 14, 2015; Published Date: December 21, 2015
Citation: Castellano-Tejedor C, Pérez-Campdepadrós M, Capdevila L, Blasco-Blasco T (2015) In The Aftermath of Cancer: The Psychological Status of Adolescent Cancer Survivors and its Correlates. J Child Adolesc Behav 3:262. doi:10.4172/2375-4494.1000262
Copyright: © 2015 Castellano-Tejedor C et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Child and Adolescent Behavior
Abstract
Objective: To assess the psychological status of adolescent cancer survivors and examined its associations with selected personal (coping, cancer-related distress) and familial factors (parents’ general stress, cancer-related distress). Method: Using a cross-sectional design, forty-one survivors (12-19 years) answered standardized measures to assess psychological well-being, mood and emotions and self-perception (KIDSCREEN-52), coping (ACS) and cancer-related distress (two numeric scales). Similarly, forty-one parents were assessed for general stress (PSS-14) and cancer-related distress (two numeric scales). Results: Mean scores for all KIDSCREEN psychological dimensions assessed were within normative values (50 ± 10). Regression analyses revealed two models with a range of explained variance between 17.3-31.1% for psychological well-being (F(2,37) = 5.070; p = 0.011) and mood and emotions (F(3,36) = 6.877; p = 0.001) respectively. Conclusion: This study provides tentative evidence that survivors’ psychological status is related to diverse personal and familial factors, especially those concerning adolescent mobilization of coping resources during hospitalization, and parental general stress in survivorship. Although psychological outcomes in survivorship appeared satisfactory compared to normative values; this study revealed that to facilitate positive psychological adaptation in the aftermath of cancer, psychosocial interventions aimed to enhance personal and family strengths to cope with the illness are needed throughout the process.
Keywords
Childhood cancer survivors; Psychological status; Coping; Distress; Parents
Introduction
There has been a notable increase in the number of adolescent cancer survivors due to improved diagnosis and treatments. In spite of these advances, survivors are at risk for numerous physical and psychological late-effects as a result of their cancer and its therapies which produce different effects on their health-related quality of life (onwards, HRQoL) [1].
Due to the potential and severe disturbances of the sequelae associated to cancer therapy, literature on the physical impact of cancer has grown rapidly in the last decades [2]. However, the mid and longterm psychological consequences of cancer also merit attention and their study has provided some contradictory results [3].
The psychological impact of cancer can extend from diagnosis to treatment and also to survivorship, and can be influenced by a wide range of psychosocial variables. In different attempts to summarize the psychological consequences of cancer once patients are in survival stage, some reviews on this topic have been published [4]. While some studies report no differences between adolescent survivors and population norms in several psychological variables (e.g., self-esteem, well-being, and mood); [3,4] other studies showed lower scores in such variables at mid-long term [5]. Moreover, there is an increasing body of research that suggests that resilience trajectories are common and a sizeable proportion of persons who experience serious illness such as cancer, report increased HRQoL; specially, showing higher scores on psychological well-being, mood and/or self-perception, as well as other positive life changes following their experience [6,7]. Despite these contradictions, all studies identify some methodological problems in empirical work that difficult comparison between studies (e.g.,, heterogeneity of designs, main variables and selected measures); [1,4]. It is worth mentioning that most of the literature agrees to identify subgroups of survivors who show higher likelihood of maladjustment or psychological disturbances (e.g., central nervous system tumors); [1,2,8]; but overall, there are no general evidences to conclude that survivors inevitably fare badly. Furthermore, it has been suggested that other psychological and socio-family factors could explain these results.
In this sense, research aimed to explore the relationship between both personal and familial factors and mid-long term HRQoL and adaptation to cancer are scarce [9,10]. When speaking about childhood cancer adaptation, one must consider not only the efforts of the patients to meet the challenges posed by the illness but also the families’ efforts. At different stages in this trajectory, coping has proved to be related to different HRQoL and adaptation outcomes [9,11,12].
Thus, cancer-related distress will be experienced by the whole family system and consequently, coping resources of all of them will be displayed. Coping consists of constant cognitive changes and behavioural adaptation (dynamic process) when handling specific external and/or internal demands that are evaluated as something that exceeds the resources of the person [13]. At the same time, is recognized for its significant impact on stress-related mental health and physical well-being for its potential intervention [14]. There is not a unique way to cope with cancer. The best way to cope would depend on the specific stressor and the features of the specific stage of the illness [15]. Scientific literature in this field has described that active coping would serve better for controllable stressors that allow certain degree of control for the individual, whereas non-active coping or disengagement strategies would be more useful in the case of noncontrollable stressors [16]. However, each cancer is different from diagnosis to specific survival situation and therefore, there is not a clear pathway [17,18]. Indeed, careful assessment of the coping process of patients and their families, especially the ways they think they would cope, is a necessary step toward designing appropriate interventions to reduce their anxiety and bolster their ability to cope with hospitalization or forthcoming challenges [19,20].
Cancer-related distress is also closely related to coping, as well as general day-to-day stress. In this sense, a certain amount of distress is normal when an individual or a relative has cancer; however, some people might be affected more than others and could start to experience high levels of distress, which would interfere with daily functioning and responsibilities [21,22]. On the one hand, if parents experience this distress, the support they provide to their child could be compromised in quantity or quality [23]. On the other hand, if the child experiences this distress, his/her coping could also be compromised and he/she could not properly adhere to treatment or other medical guidelines that are essential to the therapeutic approach [24]. Additionally, the patient could start to experience psychological disturbances that, if not attended, could lead to a major psychopathology that would hamper adaptation.
Thus, the relationship between cancer adaptation, stress and coping in the case of childhood cancer is very complex, since both patients and their parents are involved in the adaptation process from diagnosis to survivorship.
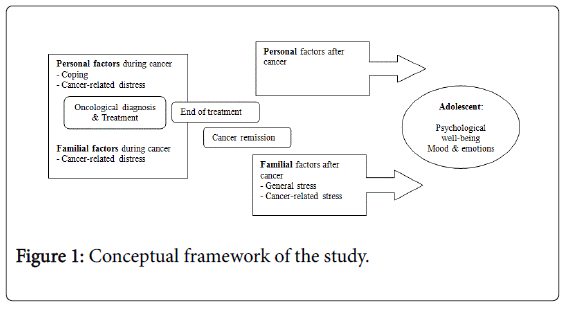
In this study, some of the above mentioned factors have been considered. The focus has been set to explore whether past and current personal and familial factors are related to different outcomes with regard to the psychological status of the survivors. The following research questions are posed: firstly, how is the psychological status of adolescent cancer survivors compared to general population? Secondly, how does certain personal (coping and cancer-related distress during hospitalization) and familial factors (general stress in survivorship and cancer-related distress during and after hospitalization) relate to such outcomes?
Methods
Study design
Descriptive study with retrospective (coping during hospitalization, cancer-related distress from patients and their parents) and crosssectional measures (psychological dimensions of patients’ HRQoL, and parents’ general stress and cancer-related stress) (Figure 1).
Ethics and setting
The whole study was carried out at the University Hospital Vall d’Hebron, pediatric Oncological and Hematological Department between May 2009 and May 2010. Ethical approval was obtained from the hospital ethics committee board. Informed consent was obtained before participation from each participant (and his/her parents) after they have received an information sheet and oral explanations about the aims and characteristics of the study. Patient confidentiality was guaranteed by the use of alphanumeric codes rather than names to identify records. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki declaration of 1975, as revised in 2000.
Recruitment and sampling
Eligible adolescent cancer survivors and their parents were identified through the RNTI-SEOP [25-27]. The RNTI-SEOP is a hospital-based central registry for all pediatric oncology centres and geographic areas of Spain. This registry was created to collect and process data related to pediatric oncology, and to provide it to national entities with research and clinical purposes.
Participants
Inclusion criteria required that: (a) adolescents had been diagnosed with cancer (excluding central nervous system tumors in order to reduce bias due to possible cognitive impairment) after the age of 8. Survivors diagnosed after the age of 8 were chosen to ensure that these patients had the appropriate cognitive maturity during cancer treatment so that reliable memories of their illness and personal experiences could be obtained. (b) To be 13-20 years old at the time of the study (both included), (c) to be off-treatment ≥ 1 year at the time of the study, and (d) to have a follow-up appointment at the reference hospital between May 2009-May 2010. Survivors with learning disabilities or psychopathology diagnosed before the first primary oncological diagnosis were excluded from the study.
Parents of the previously described survivors were also asked for participation. Only one parent for each survivor was included in the study. If both parents showed up to the assessment appointment, the primary caregiver during hospitalization and treatment (the one who spent more time at hospital) was identified and assessed (Table 1).
| Sample | Variable | Tool | Recall Period |
|---|---|---|---|
| Adolescent survivors | Demographics andmedical data | Specific protocol | At present |
| Psychological status | KIDSCREEN-52 dimensions: Psychological well-being Mood andemotions Self-perception |
At present | |
| Coping | ACS | Retrospectivea | |
| Cancer-related distress | 2-item Numeric scale | Retrospectivea | |
| Parents | General stress | PSS-14 | At present |
| Cancer-related distress | 2-item Numeric scale | Retrospectivea | |
| 3-item Numeric scale | At present |
aRetrospective: assessment based on the worst moment during hospitalization for cancer identified by the individual. ACS: Adolescent Coping Scale; PSS-14; Perceived Stress Scale-14 items.
Table 1: Assessment tools.
Measures
Summarizes the assessment tools administered to the sample
Adolescents
Demographics and medical data
Socio-demographics (gender, age, education) and illness-related data (oncological diagnosis, type of treatment, bone marrow transplant, relapse, second malignancy, age at the first diagnosis and time passed since first diagnosis) were retrieved from patients and their parents in a joint semi-structured interview and later corroborated and completed by the main researcher of this study from medical records.
Psychological status (at present): Psychological status of survivors was assessed using three dimensions of the Spanish self-reported version of the KIDSCREEN-52 questionnaire [28]. The KIDSCREEN consists of 52 items in 10 subscales: physical well-being, psychological well-being, mood and emotions, self-perception, autonomy, parent relations and home life, social support and peers, school environment, social acceptance/bullying and financial resources. For the purposes of the present research, only the psychological well-being, mood and emotions and self-perception dimensions will be considered. T-scores (M = 50, SD = 10) can be calculated for each dimension stratified by age and gender. Higher scores indicate better outcomes. In our sample, Cronbach’s Alpha values for selected dimensions were 0.83, 0.86 and 0.47 respectively.
Coping (during cancer): Coping was assessed with the Spanish version of the Adolescent Coping Scale (ACS); [26] in its specific form (retrospective measure). The ACS is a self-report checklist inventory that consists of 79 items scored on a 5-point Likert scale (ranging from 1 = doesn’t apply or don’t do it to 5 = used a great deal), which assesses the use of 18 coping strategies by adolescents in dealing with stress. Higher scores indicate higher use of these coping strategies (20-29 = unused strategy, 30-49 = strategy rarely used, 50-69 = strategy used sometimes, 70-89 = strategy used frequently, 90-105 = strategy used a great deal). These coping strategies could be collapsed into three general coping styles: solving-problem coping, coping in reference to others and non-productive coping [26]. The ACS provides normative data stratified by gender [26]. Cronbach’s alpha for the three general styles previously mentioned were 0.84 (solving problem coping), 0.84 (coping in reference to others) and 0.82 (non-productive coping).
Self-perceived emotional distress with regard to cancer and effort to overcome the hardest moments of the disease: To assess self-perceived distress and effort to overcome difficult situations during hospitalization, a 2-item numeric scale was developed. The first item assessed self-perceived distress in the hardest moments of their hospitalization period (1. According to your experience, think back and focus on the hardest moments of your cancer and rank how bad did you feel, from 0 = no distress to 10 = very distressed). The second item had the same structure; however, it was focused on the selfperceived effort to overcome with the difficult situation (2. How much effort did it take to you to bear or overcome such difficult situations? From 0 = no effort to 10 = a tremendous effort). In both cases, the score was obtained for each item from the direct value rated by the adolescent. The obtained Cronbach’s alpha coefficient was 0.66.
Parents
General stress
The level of perceived stress was evaluated by means of the Spanish version [27] of the Perceived Stress Scale (PSS). This scale is a selfreport measure that assesses the level of general perceived stress during the last month. The PSS consists of 14 items answered in a 5-point Likert scale (from 0 = never to 4 = very often) with higher scores indicating higher levels of perceived stress. The authors of the PSS-14 have indicated the cut-off point > 30 to screen for stress pathology. The PSS-14 provides normative data and has shown good psychometric characteristics [27]. In our sample, Cronbach’s Alpha was 0.82.
Self-perceived emotional distress with regard to cancer and effort to overcome the hardest moments of the disease: To assess self-perceived distress and effort to overcome difficult situations during hospitalization of their child, a 2-item numeric scale was developed. The first item assessed self-perceived distress in the hardest moments of their child hospitalization period (1. According to your perception, think back and focus on the hardest moments you have experienced during your child hospitalization and rank how bad did you feel, from 0 = no distress to 10 = very distressed). The second item had the same structure; however, it was focused on the self-perceived effort to overcome with the difficult situation previously identified (2. How much effort did it take to you to bear or overcome such difficult situations? From 0 = no effort to 10 = a tremendous effort). In both cases, the score was obtained for each item from the direct value rated by the parent. Cronbach’s Alpha was 0.52.
Cancer-related distress
To assess persistence of cancer-related distress in survivorship in the sample of parents, a 3-item numeric scale was developed to screen 1) the degree of worry, 2) frequency of thought and 3) interference of these worries in the parents’ daily routines. Items were the following: 1. Currently, how concerned are you regarding your child’s cancer? (from 0 = Not at all, to 4 = A lot), 2. Currently, how much do you think about your child’s cancer? (from 0 = Never, to 4 = A lot (several times per day) and 3. Currently, how much distress would you say is causing you all this cancer-related distress (from 0 = Not at all, to 4 = A lot). The obtained Cronbach’s Alpha was 0.91.
Procedure
Survivors eligible for the study were contacted via telephone by a qualified researcher in psychology. In this initial contact, they were informed about the purpose of the study and asked for participation. If they agreed to participate, an assessment appointment was scheduled. The assessment was conducted by the main researcher of this study, in a hospital office for a 45-minute session. At the face-to-face assessment appointment, the psychologist provided oral and written information about the study and informed consent was obtained. Demographics and medical data were collected jointly with the patient and the parents (or the primary caregiver identified) and completed with hospital records. Finally, parents were requested to remain in the waiting room and to fill out their questionnaires after appropriate instructions; simultaneously, the patient individually answered the questionnaires. At the end of the assessment, the researcher and the adolescent gathered again the parents and discussed possible issues raised after completion of the questionnaires before closing the assessment appointment. The whole process lasted approximately 90 minutes.
Data analysis
Descriptive statistics were performed for all variables considered: demographics and medical data, psychological impact (selected dimensions of HRQoL), coping, cancer-related distress (during hospitalization and in survivorship period) and general stress. Multiple linear regression analyses (stepwise) were performed to investigate the explanatory value of selected independent variables: the 3 basic coping styles for adolescents (productive coping, coping in reference to others and non-productive coping), the general stress’ scores for parents (PSS-14) and the cancer-related distress (numeric scales) experienced by both adolescents and their parents (the latter, measured at present and retrospectively), in relation to the criterion variables (psychological well-being and mood and emotions). Self-perception was not considered for regression analyses due to the low internal consistency found in our study. Analyses were corrected for (a) demographics (age and gender), and (b) medical selected variables (diagnosis, type and length of treatment, age at first diagnosis, bone marrow transplantation, relapse and second malignancy). For these purposes, non-parametric Mann-Whitney U-Tests and Pearson correlations were performed to determine which among these variables should be included in the regression analyses. All tests were two-sided with 5% significance level.
Results
Participant’s characteristics
A total of 47 survivors were asked to take part in the study. Among them, 6 survivors did not participate arguing several reasons (response rate 87.23%). Most of the non-participants just did not want to be confronted again with cancer (n = 4) and the remaining reported that they did not have enough time to participate (n = 1) or did not attend to the assessment appointment (n = 1). Finally, data from 41 survivors could be used for the analyses (26 males, 63.4%). Their demographic information along with the medical data is summarized in Table 2. Characteristics between participants and non-participants did not differ significantly with regard to demographical (age, gender, educational level) or medical data (diagnosis, type and duration of treatment, bone marrow transplantation, relapse, second malignancy, age at the first diagnosis and time passed since first diagnosis).
| N | Percentage | ||
| Gender | |||
| Male | 26 | 63.4 | |
| Female | 15 | 36.6 | |
| Educational level (at the assessment) | |||
| High school | 29 | 70.7 | |
| Professional studies | 9 | 22 | |
| University | 3 | 7.3 | |
| Diagnosis | |||
| Leukemia | 14 | 34.1 | |
| Lymphoma | 18 | 43.9 | |
| Solid tumors | 9 | 22 | |
| Treatment | |||
| Only chemotherapy | 14 | 34.15 | |
| Only surgical intervention | 1 | 2.44 | |
| Combined therapya | 26 | 63.41 | |
| Bone marrow transplantation | |||
| Yes | 11 | 26.8 | |
| No | 30 | 73.2 | |
| Relapse | |||
| Yes | 4 | 9.75 | |
| No | 37 | 90.25 | |
| Second malignancies | |||
| Yes | 1 | 2.4 | |
| No | 40 | 97.6 | |
| Mean | SD | Range | |
| Age, mean (SD) | 17 | 1.94 | 13 – 20 |
| Age at first diagnosis, mean (SD) | 11.76 | 2.55 | 8 – 16 |
| Time in years since first diagnosis, mean (SD) | 5.80 | 2.61 | 2 – 11 |
aIt includes different combinations: chemotherapy + surgical intervention + radiotherapy, chemotherapy + surgical intervention, chemotherapy + radiotherapy, radiotherapy + surgical intervention
Table 2: Demographic and medical characteristics of the sample of survivors (N = 41).
On the other side, we counted on the participation of 41 parents, 8 males (19.5%) and 33 females (80.5%). In every case, a father or a mother were evaluated by each adolescent participating. All the males that participated have a full-time job (n = 8, 100%). Among them, 4 cases (50%) had a degree equal or lower to scholar graduate, secondary school or similar degrees; 3 cases (37.5%) had completed their secondary school degree or higher; in one case (12.5%) had completed his University degree. In mothers’ case, most of them were working (n = 22, 66.6%), either full-time job (n = 15) or half-time job (n = 7). The rest were homemakers (n = 7, 21.21%), or in unemployment (n = 3, 9.09%) and only one mother was incapable and was not working (3.03%). Regarding their educational degrees, one woman (3.03%) had not cursed any degree, though she was able to read and write correctly, 5 women (15.5%) abandoned their degrees before completing the primary school, in 10 cases (30.3%) women had completed primary school, 13 women (39.3%) had completed secondary school or similar, and only 4 women (12.12%) had finished University degrees.
Descriptive Outcomes
Adolescents
Psychological status: Mean scores for each selected dimension of the KIDSCREEN-52 were examined for comparability with standardized scores from the questionnaire reference values [28]. Reported standardized mean scores of survivors were within normative values and were the following: psychological well-being M = 51.66 (SD = 8.89, range 38.37-68.49), mood and emotions M = 52.13 (SD = 10.42, range 32.51-70.91) and self-perception M = 47.78 (SD = 6.03, range 37.85-69.78). No significant differences were found with regard to gender for any dimension assessed or any of the medical variables considered in this study.
Coping styles scores: The most used coping style among survivors was problem-solving coping (M = 58.57, SD = 13.47, range 31.80-87.80, median = 59) reported as a strategy used sometimes, followed by non-productive coping (M = 47.30, SD = 9.27, range 27.43-72.14, median = 46.85) as a strategy rarely used. Finally, the less preferred style among survivors was coping in reference to others (M = 45.82, SD = 10.70, range 28.17-73.50, median = 45.16), revealed as a strategy rarely used too. No differences were found between males and females in the use of any of the coping styles assessed. The same occurred for the medical variables considered in this study.
Cancer-related distress: With regard to perceived distress in the hardest moments during hospitalization, survivors showed high mean scores for self-report distress (M = 7.98, SD = 2.16, range 2-10, median = 9) and medium-to-high scores for self-reported effort to overcome with these difficult situations (M = 6.12, SD = 3.06, range 0-10, median = 7). No differences were found with regard to gender or any of the medical variables considered.
Parents
Perceived stress scale
Mean scores for self-perceived stress for parents were medium-tolow (M = 21.51, SD = 7.51, range 4-37) showing no statistically significant differences with regard to gender. By analyzing parents’ scores on the PSS, it can be seen that 85.4% showed scores below the cut-off point (≥30); [27].
Cancer-related distress (retrospectively): With regard to perceived distress in the hardest moments while their child hospitalization, parents showed high mean scores for self-report distress (N = 40, M = 9.50, SD = 1.32, range 4-10, median = 10) and medium-to-high scores for self-reported effort to overcome with these difficult situations (N = 40, M = 7.48, SD = 3.01, range 0-10, median = 9). No differences were found with regard to gender or any other demographic feature.
Cancer-related distress (at present): With regard to cancer-related distress among parents and, specifically, the degree of worry, medium scores were found (M = 1.88, SD = 1.05, range 0-4, median = 2). The frequency of thinking was medium too (M = 1.95, SD = 0.89, range 1-4, median = 2) and the day-to-day distress or interference of distressing memories in relation to cancer was medium-to-low (M = 1.32, SD = 1.10, range 0-4, median = 1). No differences were found with regard to gender.
Multiple linear regression analyses: Multiple linear regression analyses revealed two significant models (Table 3) that, as a whole, include a percentage of explained variance (assuming the value of R2 corrected) between 17.3-31.1%. In the psychological well-being model, two variables were included. One retrospective variable from adolescents and one variable referred to parents’ general stress in survivorship. Finally, the regression model of mood and emotions included three variables; two retrospective variables from the adolescent and one current variable referred to parents. From lower to higher percentage of explained variance, regression models obtained were: mood and emotions (F(3,36) = 6.877; p = 0.001) and psychological well-being (F(2,37) = 5.070; p = 0.011).
| Standardized regression models | R2 | R2(corrected) | p | |
|---|---|---|---|---|
| Psychological well-being=(0.338 • General stress: parents) + (-0.315 • Effort at the hardest moments during cancer: adolescent) | 21.50% | 17.30% | 0.011 | |
| Mood andemotions=(-0.342 • Problem solving coping: adolescent) + (0.426 • General stress: parents) + (-0.481 • Effort at the hardest moments during cancer: adolescent) | 36.40% | 31.10% | 0.001 |
Table 3: Multiple linear regression models.
Discussion
As more children survive cancer, the physical and emotional costs of enduring cancer therapy become increasingly important. This paper is focused on the emotional costs and it raises issues about the relationship of some personal and socio-familiar variables on the psychological status of a sample of adolescents in the aftermath of cancer.
Firstly, our results suggest that the emotional status of adolescents who survived cancer is not substantially different from that of the normal population. Our findings are in line with studies of Pemberger et al. [29] and Langeveld et al. [5], which report that long-term childhood cancer survivors show comparable or even higher positive outcomes in several areas of psychological well-being (e.g., emotional status, self-esteem, etc.). Several explanations to these outcomes have been proposed. It has been pointed out that the experience of surviving cancer might lead to a different appreciation of life, own health and well-being. Thus, possible impairments or limitations could be considered as less important and internal standards, values or life priorities might change. The theory of response shift have developed and discussed further these hypotheses [30].
Secondly, in the studied sample, the preferred pattern to cope with cancer has been problem-solving coping. The non-productive coping style and the coping in reference to others style have been reported as rarely used. In general population, most of the studies reveal a preference for problem-solving coping and coping in reference to others styles when coping is assessed as a dispositional factor [26]. However, some studies with clinical samples, specifically, adolescents with cancer, have started to point out that these adolescents usually display strategies such as keep to self, ignore the problem or just not coping with the situation when their coping is measured in the specific situation of the hospitalization for cancer and its subsequent procedures [31]. This concept has been called “repressive adaptative style” [18] and it has been defined as a person’s tendency to inhibit the experience and the expression of negative feelings or unpleasant cognitions in order to prevent one’s positive self-image from being threatened [18]. Additionally, an individual with such coping style is operationally identified by low scores on trait anxiety but high scores on a measure of defensiveness. It has been discussed that this style may help to cope with the uncertainty of the prognosis and some of the uncontrollable situations that the adolescent might face throughout the oncological process. As it has been proposed, a disengagement coping style could be adaptative if it circumscribes to a specific situation, is temporary, and no control over the stressor could be performed [13]. Repression, or in its alternative form of blunting, minimizing, and rejecting, refers to a defensive maneuver in which the individual employs strategies to avoid or negate awareness of affects and impulses. Therefore, this type of coping could help individuals to bear with the situation and to keep their psychological well-being relatively stable.
As expected, cancer-related distress among adolescents was high (median = 9), but self-reported effort to cope and overcome these situations was lower (median = 7). The high values of distress are not surprising since they were asked to rate their distress in the worst situation throughout their oncological process. In contrast, the scores regarding the effort to cope were lower than expected and mainly focused on solving the problem. A higher prevalence of active coping strategies in front of difficult situations is commonly observed both in general and clinical samples. Therefore, the use of such strategies could provide a certain sense of mastery and control among adolescents and modulate their self-perceived effort to cope with difficult situations impose by cancer. Additionally, resilience framework could also help to understand such results [7,9,23]. For example, having enough social support at that time could reduce the efforts of the adolescents to cope and ask for additional help (e.g., lower use of coping in relation to others). Much of the literature on cancer survivors has focused on negative consequences of cancer; however, there is an increasing body of research that studies positive outcomes in the aftermath of cancer and related variables that may enable such results [6]. For all phases of the cancer continuum, resilience descriptions include preexisting or baseline features, such as demographics and other personal variables (e.g., personality traits, optimism, social support), mechanisms that enhance positive adaptation (e.g., coping strategies) and medicalrelated factors (e.g., cancer prognosis, relationship with healthcare providers, etc.); [7]. Therefore, promoting resilience by recognizing and optimizing all these potential related variables, when possible, is a critical element of an integrative approach of cancer patients’ psychosocial care. Finally, although most of the survivors appear to lead normal adult lives (e.g., achieving different educational degrees, good jobs, socio-familiar status, etc.) there is also a small percentage of them who show some psychological problems such as anxiety, depression, fear of recurrence or related complications [1,2]. Thus, the proper evaluation of the cancer-related distress, or even posttraumatic distress symptoms, is required.
With regard to parents, general daily stress in survivorship was medium-to-low suggesting that a normal recovery pattern has been achieved. Similarly, cancer-related distress in survivorship has shown medium-to-low scores, suggesting no persistent distress (median 1 and 2). However, cancer-related distress during the adolescent hospitalization was high for both variables assessed; self-perceived distress (median = 10) and effort to cope with the situation (median = 9). According to existing literature on this topic [23], our findings revealed that parents experience great distress throughout the process and even in survivorship. Therefore, they could benefit from interventions targeted to offer support, counseling, encouragement or even to allow expression of their worries and feelings [23]. Professionals responsible for cancer patients need to assess the impact of cancer diagnosis and treatments on parents’ well-being, in order to prevent future complications and enhance positive adaptation. Only by doing this, it will possible to increase parents’ strengths and resources during the challenging trajectory of their children’s cancer, with the ultimate purpose of provide optimal care for the child with cancer.
With regard to the regression analyses, two models comprising a combination of past and current variables from both adolescents and their parents have been obtained. Overall, the psychological status of the adolescent survivor seems to be significantly related to the experience that him/her-self had about the oncological process. Specifically, of the worst self-reported situations. In this sense, several studies have reported the importance of providing a multidisciplinary and integrative care to the whole family system, not only to the adolescent patients. Moreover, this support should be offered throughout the whole process, including the survivorship stage with accurate follow-ups [10,23]. This approach would enhance positive adaptation on the family at each stage and this is expected to lead to a better patients’ HRQoL once they are at survivorship.
Within this context, it has been observed a negative relationship between problem solving coping and the efforts realized during the hardest moments of the disease, and the psychological well-being and mood and emotions scores. These results suggest that starting up active coping mechanisms or mobilization of socio-familiar resources in front of non-pleasant situations (or during acute processes noncontrolled by the patient), it is likely to cause emotional distress and worsen survivors’ psychological outcomes at mid-long term [19].
Regarding general stress of parents in survivorship, it positively related to the psychological outcomes of the adolescent survivor in the psychological well-being and mood and emotions dimensions. If we observe the parents’ scores on the PSS, the vast majority (85.4%) of them show up results below the cut-off point (≥30). Therefore, it could be said that families are “little stressed” with activation levels similar to those observed in the general population [27]. However, this scale assesses self-efficacy and helplessness with items asking about time to oneself, time to finish up daily chores, thoughts about pending issues, feeling nervous or the ability to control day-to-day hassles. Perhaps our results may indicate the dedication and extra efforts performed by these parents, to take care of their responsibilities and the specific needs of their child now that he/she has overcome cancer. Consequently, parents could feel moderately stressed and sometimes overload, but the adolescent survivor could perceive the care and attentive concern displayed by their parents. As a result, better scores on psychological well-being and mood could be displayed among these cancer survivors.
Limitations
There are some limitations that need to be considered for the current study. First, there is a relatively small sample of survivors that could undermine the generalization of results and a retrospective cross-sectional study could not be the best design to explore such issues, due to the malleability of memory and current mood as a potential bias for recollecting pass stressful memories. Secondly, it is conceivable that some of the non-participating survivors (those who refuse to participate in the study) experienced different psychological outcomes. However, it is not clear whether this would result in better or worse results. For example, patients who feel good might disregard the importance of the study and, on the other hand, it is also possible that some survivors may have refused to collaborate to avoid being confronted again with their disease and their memories, which might suggest concerns or persistent distress, or even less effective coping strategies and poorer emotional adaptation in survivorship. Third, it could be said that the emotional status of survivors was only partially explained by the factors that were investigated in the present study and one regression model accounted only for the 17.3 of explained variance including two variables. Other explanatory factors, such as personality traits or other stressful life situations may also be of importance. Additionally, we believe it is important to consider the incidence and spectrum of late effects following cancer treatments. Similarly, psychological status’ results might be influenced by the choice of a general measure of HRQoL which also revealed low internal consistency for self-perception dimension in our studied sample. A non-specific and generic questionnaire may not identify potential problematic issues, specially associated to this population. Moreover, possible benefit finding in the aftermath of trauma is neither registered with these assessment tools. Unfortunately, there are not too many valid questionnaires and properly adapted to different socio-cultural contexts for these purposes. We suggest for future studies to have this in consideration.
Conclusions and Clinical Implications
With the number of adolescent cancer survivors continually increasing, it is important to acknowledge what specific variables could foster and facilitate positive adaptation throughout the whole process. Considering that parents are the main providers of social support for such patients and that they would support them in their cancer journey in several ways, not including their variables into the equation would be a big mistake. In addition, to understand adolescents’ coping strategies and distress facing cancer have been suggested as key elements to design tailored psychosocial interventions aimed to positively influence their psychological adjustment and HRQoL throughout hospitalization and at survival.
In summary, given all the variation in findings about pediatric cancer survivors’ psychological status, more data is needed to provide a more comprehensive picture of the characteristic and specific needs of this population. The results of the present study may be helpful in comprehending these issues and add to the existing knowledge with new insights.
Acknowledgements
The authors would like to thank all the adolescent cancer survivors and their parents for their disinterested contribution to this study. We also thank Rajmil for his comments and help with the questionnaire KIDSCREEN-52.
References
- Cantrell MA (2011) A narrative review summarizing the state of the evidence on the health-related quality of life among childhood cancer survivors. Journal of Pediatric Oncology Nursing28: 75-82.
- McDougall J, Tsonis M (2009) Quality of life in survivors of childhood cancer: a systematic review of the literature (2001-2008). Support Care Cancer 17: 1231-1246.
- Wechsler AM, Sánchez-Iglesias I (2013) Psychological adjustment of children with cancer as compared with healthy children: a meta-analysis. Eur J Cancer Care (Engl) 22: 314-325.
- Eiser C, Hill JJ, Vance YH (2000) Examining the psychological consequences of surviving childhood cancer: systematic review as a research method in pediatric psychology. J PediatrPsychol 25: 449-460.
- Langeveld NE, Grootenhuis MA, Voûte PA, de Haan RJ, van den Bos C (2004) Quality of life, self-esteem and worries in young adult survivors of childhood cancer. Psychooncology 13: 867-881.
- Aspinwall LG, MacNamara A (2005) Taking positive changes seriously. Cancer 104: 2549-2556.
- Castellano-Tejedor C, Blasco-Blasco T, Pérez-Campdepadrós M, Capdevila-Ortís L (2014) Making sense of resilience: a review from the field of paediatric psycho-oncology and a proposal of a model for its study. Anales de Psicología 30: 865-877.
- Pérez-Campdepadrós M, Castellano-Tejedor C, Sábado-Álvarez C, Gos-SubíasLl, Capdevila-OrtísLl, et al. (2014) Type of tumor, gender and time since diagnosis affect differently health-related quality of life in adolescent cancer survivors. Eur J Cancer Care (Engl) 24: 635-641.
- Patterson JM, Holm KE, Gurney JG (2004) The impact of childhood cancer on the family: a qualitative analysis of strains, resources, and coping behaviors. Psychooncology 13: 390-407.
- Yagci-Küpeli B, Akyüz C, Küpeli S, Büyükpamukçu M (2012) Health-related quality of life in pediatric cancer survivors: a multifactorial assessment including parental factors. J PediatrHematolOncol 34: 194-199.
- Castellano C, Pérez-Campdepadrós M, Capdevila L, Sánchez de Toledo J, Gallego S, et al. (2013) Surviving childhood cancer: relationship between exercise and coping on quality of life. Span J Psychol 16: 1-8.
- Maurice-Stam H, Oort FJ, Last BF, Grootenhuis MA (2009) A predictive model of health-related quality of life in young adult survivors of childhood cancer. Eur J Cancer Care (Engl) 18: 339-349.
- Lazarus RS, Folkman S (1984) Stress, appraisal and coping. New York: Springer Publishing.
- Taylor SE, Stanton AL (2007) Coping resources, coping processes, and mental health. Annu Rev ClinPsychol 3: 377-401.
- Kazak AE (2005) Evidence-based interventions for survivors of childhood cancer and their families. J PediatrPsychol 30: 29-39.
- Penley JA, Tomaka J, Wiebe JS (2002) The association of coping to physical and psychological health outcomes: a meta-analytic review. J Behav Med 25: 551-603.
- Franks HM, Roesch SC (2006) Appraisals and coping in people living with cancer: a meta-analysis. Psychooncology 15: 1027-1037.
- Garssen B (2007) Repression: finding our way in the maze of concepts. J Behav Med 30: 471-481.
- Aldridge AA, Roesch SC (2007) Coping and adjustment in children with cancer: a meta-analytic study. J Behav Med 30: 115-129.
- Hagedoorn M, Kreicbergs U, Appel C (2011) Coping with cancer: The perspective of patients' relatives. ActaOncol 50: 205-211.
- Amador DD, Gomes IP, Reichert AP, Collet N (2013) Impact of childhood cancer for family caregivers: integrative review RevistaBrasileira de Enfermagem 66: 264-270.
- Enskar K, von Essen L (2007) Prevalence of aspects of distress, coping, support and care among adolescents and young adults undergoing and being off cancer treatment. Eur J OncolNurs 11: 400-408.
- Long KA, Marsland AL (2011) Family adjustment to childhood cancer: a systematic review. Clin Child FamPsychol Rev 14: 57-88.
- Evan EE, Zeltzer LK (2006) Psychosocial dimensions of cancer in adolescents and young adults. Cancer 107: 1663-1671.
- BonetPeris- R, B Giner Garcia A, Sanchez de Toledo J, T Acha (2003) National Childhood Tumor Registry (RNTI - SEOP). Basic statistics from 1980 to 2001. Survival 1980-1997. Valencia: Valencia University.
- Pereña J, Seisdedos N (1996) ACS Manual: teen coping scales. Madrid: Ediciones TEA.
- Remor E (2006) Psychometric properties of a European Spanish version of the Perceived Stress Scale (PSS). Span J Psychol 9: 86-93.
- Ravens-Sieberer U, Gosch A, Rajmil L, Erhart M, Bruil J, et al. (2008) The KIDSCREEN-52 quality of life measure for children and adolescents: psychometric results from a cross-cultural survey in 13 European countries. Value Health 11: 654-658.
- Pemberger S, Jagsch R, Frey E, Felder-Puig R, Gadner H, et al. (2005) Quality of life in long-term childhood cancer survivors and the relation of late effects and subjective well-being. Support Care Cancer 13: 49-56.
- Schwartz CE, Bode R, Repucci N, Becker J, Sprangers MA, et al. (2006) The clinical significance of adaptation to changing health: a meta-analysis of response shift. Qual Life Res 15: 1533-1550.
- Phipps S (2007) Adaptive style in children with cancer: implications for a positive psychology approach. J PediatrPsychol 32: 1055-1066.
Relevant Topics
- Adolescent Anxiety
- Adult Psychology
- Adult Sexual Behavior
- Anger Management
- Autism
- Behaviour
- Child Anxiety
- Child Health
- Child Mental Health
- Child Psychology
- Children Behavior
- Children Development
- Counselling
- Depression Disorders
- Digital Media Impact
- Eating disorder
- Mental Health Interventions
- Neuroscience
- Obeys Children
- Parental Care
- Risky Behavior
- Social-Emotional Learning (SEL)
- Societal Influence
- Trauma-Informed Care
Recommended Journals
Article Tools
Article Usage
- Total views: 11904
- [From(publication date):
December-2015 - Aug 30, 2025] - Breakdown by view type
- HTML page views : 10856
- PDF downloads : 1048