Influence of Lumbar Disc Herniation on Chronaxie and Rheobase in Patients with Chronic Low Back Pain-A Quasi Experimental Pilot Study
Received: 11-Mar-2015 / Accepted Date: 26-Mar-2015 / Published Date: 03-Mar-2015
Abstract
Aim: To investigate the influence of lumbar disc herniation on rheobase and chronaxie in patients with low back pain.
Methods: The Strength duration curve, rheobase and Chronaxie in 10 LBP patients with radiculopathy due to lumbar disc herniation and 10 healthy controls were obtained following stimulation of tibialis anterior and peroneus muscles.
Results: Tibialis anterior and peroneus muscles in both Low back patients with radiculopathy due to lumbar disc herniation and healthy control showed normal pattern of strength duration curve typical of an innervated muscle. The rheobase and chronaxie values for tibialis anterior were 11.8 ± 1.93 and 0.54 ± 0.014 respectively in LBP patients and 7.4 ± 0.84 and 0.24 ± 0.14 respectively in control subjects. The rheobase and chronaxie values for peroneus muscles were 12.8 ± 2.93 and 0.41 ± 0.07 respectively in LBP patients and 7.6 ± 1.71 and 0.16 ±0.01 respectively control subjects. Rheobase and chronaxie were significantly higher in low back pain patients with radiculopathy than apparently healthy control subjects (P<0.00).
Conclusion: Findings from this study demonstrated higher rheobase and chronaxie in patients with LBP and lumbar disc herniation than the control subjects. The outcome of this study will be used to do power size calculation for a large randomised controlled trial
Keywords: Lumbar disc herniation; LBP; Chronaxie Rheobase
360636Introduction
Plotting a Strength duration curve (SDC) requires stimulating a muscle at its motor point with fixed pulse duration, ranging from 0.01 to 300 milliseconds (ms), recording the current strength in milliampere mA required to elicit a threshold twitch contraction. The mA values obtained and the pulse duration utilized is plotted on the X and Y axis respectively to obtained SDC graph [1]. The SDC was historically performed from the 1930s-1960s to assess nerve injuries prior to the common recent use of electromyography and nerve conduction testing [1]. SDC was a mean of evaluating the severity and subsequent recovery of a nerve injury. It provides graphic representation of the integrity of the muscle-nerve complex. The SDC remains useful even though electrophysiologic evaluation techniques have become more sophisticated in the past three decades, it still remains a reliable index of muscle/nerve functional integrity [1,2]. The response of a nerve and a muscle to electrical stimulus depend on three variable excitation factors: strength of the stimulus, period of time for which the current flows and the rate of change of the stimulus. In SDC testing, the stimulus consist of rectangular impulses of interrupted direct current of varying strength and duration. SDC of a denervated muscle will be shifted to the right compared to normal innervated muscle; subsequently shifting to the left occur during re-innervation [1]. Thus, SDC can be used to demonstrate or confirm normal innervation of a muscle, presence or progress of lower motor neuron lesion disorders [1,2].
For many years, traditional electrodiagnosis has been the main means of testing for radiculopathies caused by lumbar disc herniation. Historically, the use of electrodiagnosis in the study of radiculopathies with disc compression evolved in three stages. It began in 1868 with Erb’s method of electrodiagnosis by faradic and galvanic currents. The second stage, first through Lapigue in 1926 and then in 194, saw the introduction of the SDC obtained with rectangular or triangular-wave electrical pulses of variable duration and the three typical types of curve corresponding to normality, partial denervation, and total denervation [2]. The introduction of the needle-concentric electrode by Adrian and Bronk in 1929 marked the start of the last stage, the electromyographic one, which expanded in the 1960s. Electromyography (EMG) still constitutes the instrumental methodology of reference in the central and peripheral nerve and muscle pathologies [3].
In patients with chronic low back pain, it is important to establish whether or not radiculopathy is present. This is not difficult when clinical, radiological and electromyographic abnormalities consistent with focal nerve root involvement are found [4]. However, a high percentage of the patients referred to back pain clinics presents with leg pain only. The neurological examination may be normal or confusing showing non-radicular sensory changes [5]. Imaging studies may lack diagnostic specificity [6]. Needle EMG, which tests only ventral root function, may be normal in the absence of motor symptoms [6]. The clinical presentations of lumbosacral radiculopathy vary according the level of nerve root or roots involved. The most frequent are the L5 and S1 radiculopathies [6]. Patients present with pain, sensory loss, weakness, and reflex changes consistent with the nerve root involved. However, in radiculopathies, when the level of radicular compression must be sought, there appears to be no reason to abandon traditional electrodiagnosis i.e. SDC testing, which, compared to EMG, is easy to perform, is clearly better tolerated by patients and less costly [3,7,8]. It appears that SDC is not used as often as it could be, which may be due to lack of appreciation of its possible uses or its proven accuracy. The possibility of disc herniation with compression on peripheral nerves leading to reduction in the conduction velocity and alteration in SDC parameters in terms of an increase in rheobase and/or chronaxie of the affected nerve root segments has been suggested [9]. Effects of graded compression on nerve function were analysed by Dahlin et al. [8] in order to evaluate the relative importance of pressure level and duration of compression for functional deterioration. In Dahlin etal’s study, the pressure was applied by means of a small inflatable cuff and the effects of two pressure levels, i.e., 80 mm Hg applied for 2 hr or 400 mm Hg applied for 15 min, were studied in rabbit tibial nerves. Their findings indicated that mechanical pressure on peripheral nerve could cause ischemia of the compressed nerve segment and some degree of mechanical deformation of the nerve trunk, which in turn could lead to incomplete recovery following pressure release. They also concluded that duration of compression is of importance for the degree of nerve injury.
The correlation of the SDC with clinical and electrodiagnostic findings in normal individuals and in patients with subnormal peripheral nerve conduction and with EMG equivalents of axonal lesion was reported by [10]. In a similar vein, Nardin et al. [4] reported the accuracy of SDC parameters in evaluating chronic entrapment neuropathies in proportion to the incidence of axonal lesion.
Analysis of literature, reveals a scarcity of data on characteristics pattern of SDC in patients who suffer low back pain (LBP) with radiculopathy as a results of disc herniation. The present study was designed to compare SDC characteristics pattern and to compare rheobase and chronaxie between patients with low back pain lumbar spine disc herniation at L4/L5 and apparently healthy adults. We hypothesize that chronaxie and rheobase values will be significantly higher in LBP patients with radiculopathy than in apparently healthy individuals.
Methods
Design
A Quasi experimental pilot study design to compare rheobase and chronaxie in apparently healthy subjects and LBP patients with lumbar radiculopathy.
Recruitment strategy sampling technique and sample siz
Participants were recruited from among patients with chronic low back pain from Orthopaedic and Medical outpatient’s clinics of the University of Maiduguri Teaching Hospital, Maiduguri Borno State. Prior to this, recruitment posters and handbills were distributed to prospective participants in the outpatient clinic. Recruitment posters were also displayed on notice boards at strategic areas within the hospital. Convenient samples of 20 subjects including 10 LBP patients and 10 apparently healthy individuals volunteered to participate in this study. This sample size was adopted from a similar study by Dahlin et al. [8] in which mechanical effects of compression of peripheral nerves was investigated.
Participants
LBP patients with pain radiating to the leg and with a diagnosis of disc herniation at the lower lumbar region including L4/L5 seen at the Department of Physiotherapy, University of Maiduguri Teaching Hospital (UMTH), Maiduguri were recruited. The diagnosis was established on the basis of clinical findings and the report of the radiological investigations [X –ray and magnetic resonance imaging (MRI)] from a consultant Radiologist. Patients with any signs of serious spinal pathology (red flag), comorbid autoimmune or neoplastic pathologies were excluded. Individuals with peripheral and systemic/metabolic disease were excluded from the study. The study included 10 patients with mechanical back pain and lumbar disc herniation and 10 apparently healthy subjects. The apparently healthy subjects were recruited from among the staff and students at UMTH, they were those who have not experienced LBP for at least 2 years prior to commencement of this study, they also underwent radiological investigations to rule out the presence of lumbar disc herniation. Participants’ recruitment was carried out between February 2014 and December 2014.
Ethics
Approval to carry out this study was obtained from the Research and Ethics Committee of the University of Maiduguri Teaching Hospital. All the subjects were informed of the purposes of the research and of the modalities of the study and all took part in it voluntarily after signing an informed consent form.
Patient preparation
All the participants in the study underwent a clinical assessment and a detailed physiological and pathological history was collected. For patients with LBP and lumbar disc herniation, tibialis anterior and peroneus group of muscles on the side of pain radiation were assessed. For apparently healthy subjects, a random method was used to select either right or left tibialis anterior muscle and peroneus group of muscles to minimize systematic error. Subjects were positioned in supine lying with small pillows underneath the head and knees for comfort during the testing procedure. Subjects were draped so that the lower extremity below the knee was uncovered. To maintain a standardized resting-length position of the tibialis anterior and peroneus muscles, the subject's feet were placed against a 90-degree footboard.
Equipment preparation
An electrical stimulator with interrupted direct current facility was used for the SDC testing. All the wires from mains to plug box and to the machine are intact and properly insulated. The examiner tested the machine by attaching leads and electrodes to the terminals and by switching ‘on’ the machine and increasing the intensity to feel the current. The dispersive electrode was large (300 cm2); the active stimulating electrode was small (4 cm2). Both electrodes were covered with gauze and soaked in a hypertonic sodium chloride solution before each subject was tested.
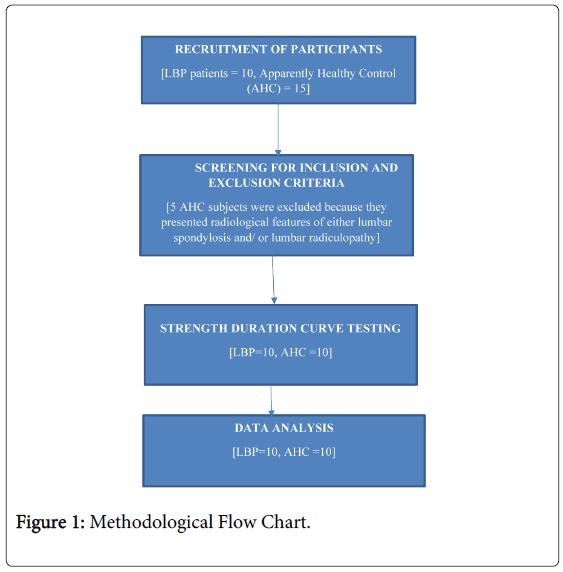
Procedure: SDC testing was carried out on tibialis anterior and peroneus muscles since L4/L5 disc herniation with nerve root compression could cause Impairment of conduction on nerve supply to the hallux (big toe), ankle evertors (peroneus) and ankle dorsiflexors (tibialis anterior). The dispersive electrode was placed underneath the gastrocnemius muscle, at the point of entrance of common peroneal nerve into the ankle dorsiflexors and evertors muscles and was secured to the leg with a Velcro strap to assure proper contact. To locate where to place active electrode, the anatomic boundaries of each of the tibialis anterior muscle and peroneus group of muscles were noted when the subject actively dorsiflexed and everted the ankle of the selected limb respectively. The largest muscle mass during contraction was usually located about halfway between the proximal and distal muscle fibre attachments. This area roughly corresponds to the region where the band of motor endplates runs transversely across the muscle [8]. The active electrode was then moved about several points within this location to get a location of greatest contraction with least stimulation. Velcro strap was used to secure the active electrode at this site to avoid problems arising from movements of electrode during testing. The SDC was obtained by using the standard clinical technique of successively decreasing the pulse widths (300, 100, 50, 38, 10, 7, 5, 3, 0.8, 0.6, 0.4, 0.3, 0., and 0.05 ms) while noting what current (mA) was necessary to maintain a minimal visible contraction of the muscle. These values were recorded for each pulse duration. The longest pulse duration is chosen first and the intensity of the current is increased until the minimum observable contraction is obtained before shifting to the second longest pulse duration etc. The rheobase i.e. is the smallest current that will produce a muscle contraction and the duration of the shortest impulse that will produce a response with a current of double rheobase is the chronaxie. The evaluator was blinded to the group allocations of the participants and was not involved in any other aspects of the study (Figure 1).
Statistical analysis
Descriptive demographic data was presented as mean, standard deviation, frequency and percentage. Chronaxie and rheobase values were reported as mean and standard deviation. Independent t-test was used to test the differences in the mean rheobase and chronaxie between the apparently healthy subjects and low back pain patients with radiculopathy. Differences at P<0.05 were considered significant. The analysis was carried out using the SPSS 10.0 for Windows.
Results
The demographic characteristics of the participants is presented in Table 1. We examined 10 LBP patients with disc herniation (6 males, 4 females) and 10 apparently healthy controls (6 males, 4 females). Mean age of LBP patients and controls was 40.2 ± 10.3 and 41.6 ± 8.93 years respectively. Significant differences in gender and age and BMI were not observed between the patients and controls (P>0.05).
| Characteristics | SLBPR | AHS | P-values |
|---|---|---|---|
| Age[X±SD] | 40.2±10.3 | 41.6±8.9 | 0.987 |
| Gender N [%] | |||
| Male | 6[60] | 6[60] | 0.985 |
| Female | 4[40] | 4[40] | |
| BMI [X±SD] | 23.5± 8.9 | 24.2±7.8 | 0.763 |
| LBP duration [X±SD] | 3.4±0.9 | NA |
SLBR: Subjects with low back pain and radiculopathy
AHS: Apparently Healthy Subjects
N: Number of subjects
NA: Not applicable
Table 1: Demographic Characteristics of the participants.
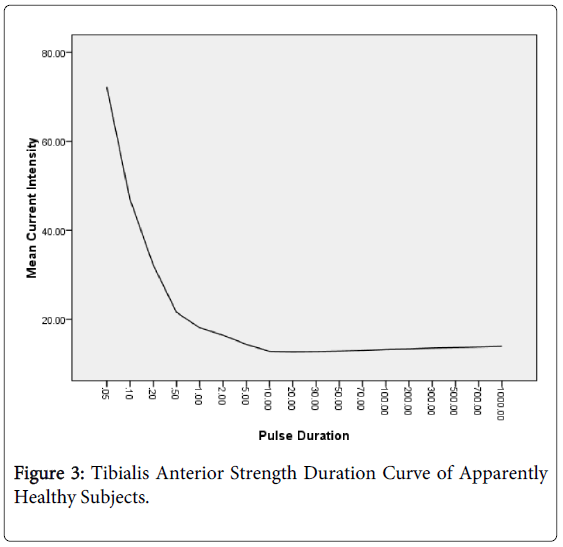
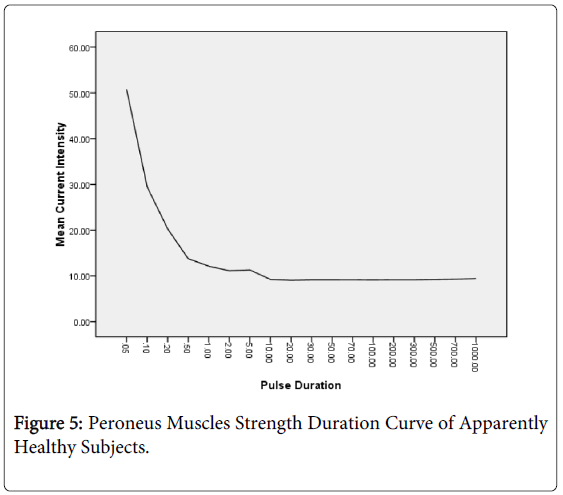
Figures 2-5 show the SDC obtained by plotting the mean minimum current required to elicit perceptible contraction at successively decreasing the pulse widths (300, 100, 50, 38, 10, 7, 5, 3, , 0.8, 0.6, 0.4, 0.3, 0., and 0.05 msec for the LBP patients and apparently healthy respectively.
Table 2 shows that the mean rheobase and chronaxie values for Tibialis anterior muscles were 11.8 3 ± 1.93 mA and 0.54 ± 0.14 ms in the LBP patients and 7.4 ± 0.84 mA and 0.24 ± 0.14 ms in apparently healthy controls, respectively.
| Rheobase (mA) | Chronaxie (ms) | |||
|---|---|---|---|---|
| TBA | PER | TBA | PER | |
| LBP patients | 11.8 ± 1.93 | 12.8 ± 2.93 | 0.54 ± 0.14 | 0.41 ± 0.07 |
| Apparently Healthy | 7.4 ± 0.84 | 7.6 ± 1.71 | 0.24 ± 0.14 | 0.16 ± 0.01 |
| t-value | 3.50 | 5.65 | 3.55 | 16.58 |
| P-value | <0.005* | <0.005* | <0.005* | <0.005* |
TBA = Tibialis Anterior
PER = Peroneus Muscles
Table 2: Participants Mean Rheobase and Chronaxie values.
In a similar vein, the rheobase and chronaxie values for peroneus muscles were higher in LBP patients (12.83 ± 2.93 mA, 0.41 ± 0.07 ms) than the apparently control subjects (7.6±1.71 mA, 0.16± 0.01 ms). There were statistically significant differences in rheobase and chronaxie values for peroneus and tibialis anterior muscles between the patients and apparently healthy controls (<0.05).
Discussion
The purpose of this study was to investigate the influence of lumbar disc herniation on rheobase and chronaxie in patients with LBP. Inclusion of apparently healthy control subjects without clinical signs and symptoms of LBP but with radiological features of lumbar spondylosis and/or lumbar radiculopathy could constitute potential confounding variables. Thus, only those participants who have not experienced LBP for at least 2 years prior to this study and without radiological features of lumbar radiculopathy served as control in this study. The Methodological flow chart is presented in Figure 1. In the present study, the SDC obtained for both apparently healthy subjects and LBP with disc herniation is typical of a normal SDC. A Normal curve as described by Sri et al. [10], is a continuous rectangular hyperbola consisting of two parts; the parts due to stimulation with pulse duration below 1.0 ms where the curves incline upwards and the part due to stimulation with pulse duration above 1 mseconds where the curve is horizontal. What is different however, is the value of rheobase and chronaxie obtained between the apparently healthy subjects and the low back pain patients with disc herniation for each of the muscle investigated.
The rheobase is the smallest current that will produce a muscle contraction. Reported Normal values of rheobase in the literature vary considerably, Harris [11] gave a value of 8 to 35 volts, Richardson and Parry [12] reported a value which ranged from 15 to 30 volts. The electrical stimulator used in the present study was calibrated in milliampere thus the rheobase values obtained could not be compared with those in Harris’s and Richardson and Parry’s studies. There could be considerable variation in the values of rheobase and chronaxie for the same muscles in normal healthy individuals depending on whether a constant voltage or a constant ammeter electrical stimulator is used. Melo et al. [13] reported a rheobase value of 19 mA ± 8.0 for tibialis anterior muscles in patients with polyneuromyopathy of critical illness which was slightly higher than the rheobase for Tibialis anterior in low back pain patients with radiculopathy obtained in the present study. The differences might be partly due to the differences in the underlying conditions of patients in both studies which in turn might have affected the electrical property of the peripheral nerve differently.
Chronaxie is the minimal period of time for which a stimulus must flow to produce a contraction, when using a stimulus of twice the rheobase strength. It is a convenient single value for excitability of a tissue and has been used as an isolated diagnostic test [2]. It appears that chronaxie for low back pain patients with radiculopathy has not been widely reported, however, the chronaxie of nerve and/or innervated muscle is short, usually less than 1 ms; denervated muscle is a larger capacitor requiring more energy to discharge, usually with a chronaxie of greater than 1 ms [3] and could be as ten times higher than a normal innervated muscles. The values of chronaxie recorded in the present study was lower than 1 ms, thus similar to those of the previously reported for normal individuals. Different values of chronaxie have been reported for normal individual in the literature. Ritchie [14] found the normal chronaxie values ranges from 0.03 to 0.08 ms while Richardson and Wynn-Parry reported 0.05 to 0.5 ms, 0.07 to 0.3 ms was reported by Harris [11] while 0.08 to 0.7 ms was reported by Arid [15]. Mogvoros et al. [9] and Kanai et al. [16] in their studies reported that strength duration time constant (SDTC) was longer in patients with diseases that affect the lower motor neurons/axons. However findings from their studies could not show statistical significant difference in the Rheobase and Chronaxie values obtained between patients with lower motor neuron lesion and healthy controls. Moreso, the underlying pathological mechanism of the subjects in their study is not same as lumbar radiculopathy, thus the results of their study could not be compared with the present study.
However, there is a need for caution when reporting, comparing and interpreting chronaxie values. Mogyororos [9] showed that chronaxie values are alike for anatomically related muscles of synergistic function; that proximal muscles (neck, trunk and shoulder and hip) have lower chronaxies than distal muscles and muscles of facial expression. Anterior muscles have lower chronaxies than posterior muscles in the same limb segment and flexor muscles have lower chronaxie than extensor muscles [11]. Mogyoros [9] pointed out that in children under the age of eighteen months, chronaxie is ten times greater than the expected value. At birth, chronaxie is ten times higher than normal, at 3rd month the values are lower, but still high and by 18-20 months the chronaxies fall to normal values. Dry skin, muscle fatigability and tissue ischaemia has been reported to increase threshold and decrease excitability of nerves and muscles by as much as 100% [1,16]. Direct explanation was not offered for the varying values of chronaxies due to these factors. However a rule of thumb to be kept in mind is that the effects of an electrical fields on peripheral nerves i.e. depolarisation and hyperpolarisation are always greater on the larger diameter axons and axons closest to the electrode [15-17].
The higher rheobase and chronaxie values in low back pain patients with disc herniation than apparently healthy subjects in the present study might be due to the effects of reduced conduction velocity of the nerve root caused by compression due to disc herniation. Studies comparing the chronaxie and rheobase values in patient with LBP and healthy control are scarce thus, limiting comparison of the results of the present study with others. In cases of nerve root compression caused by disc herniation, there is evidence of raised chronaxie levels in the muscles supplied by the affected nerve root. It has been reported that a compression of 200 mmHg sustained for two hours or more could cause gradual reduction on nerve conduction velocity only at the level of compression, in contrast to the nerves compressed at 400 mmHg for two hours in which conduction velocity was reduced both at the level of compression and distal to the compressed segment. Morphologically, the nerves compressed at 200-400 mmHg for two hours showed varying degrees of demyelination and axonal degeneration three weeks after compression [16]. Depending on the amount of pressure exerted on the peripheral nerve, it could also be that not all cases of disc herniation or compression on peripheral nerves will eventually alter the nerve conduction velocity rheobase and/or chronaxie. A pressure of 50 mmHg applied for two hours induced only minimal or no deterioration of maximal conduction velocity and nerve fibre structure.
Implication for practice
Findings from the present study in terms of significant differences in the values of rheobase and chronaxie obtained with SDC between healthy control and low back pain patients with disc herniation might implies that strength duration test and SDC could be used to compliment normal procedure of assessment of low back pain patients with disc herniation. SDC test might not replace other diagnostic methodologies for low back pain with disc herniation but could be complementary to them. It could be that SDC may be useful in the diagnostic phase prior to rehabilitation and in the monitoring of post-surgical rehabilitation of this group of patients. More generally, it may be used in evaluating the effectiveness of a treatment or as a support in the diagnosis of these neuromusculoskeletal disorders [18]. SDC electrodiagnostic testing is not influenced by the will of the subject and for this reason it might also be suitable for medical-legal purposes [19,20]. More so, SDC test is rapid to administer, patient compliance is good, and the costs of instrumentation are contained. For these reasons, SDC remains a valuable test in clinical practice. It might be preferred in patients with particular infectious pathologies or in those who are resistant to the use of the needle.
Limitation
The study was underpowered by small number of subjects which in turn could impact on the external validity including generalizability and representativeness of the findings of this study. However, the results of this study will be useful to do a power size calculation to determine the minimum number of participants that will be required for our future large randomised controlled trial.
Conclusion
The outcome of this study showed evidence of raised chronaxie and rheobase in patient with low back pain with disc herniation in the muscles supplied by affected nerve root. We therefore suggest the use of strength duration test to compliment the procedure of assessment of patients with low back pain with disc herniation.
References
- Friedli WG, Meyer M (1984) Strength-duration curve: a measure for assessing sensory deficit in peripheral neuropathy.J NeurolNeurosurg Psychiatry 47: 184-189.
- Jablecki CK, Andary MT, Di Benedetto M, Horowitz SH, Marino RJ, et al. (1996) American Association of Electrodiagnostic Medicine guidelines for outcome studies in electrodiagnostic medicine.Muscle Nerve 19: 1626-1635.
- Nardin RA, Patel MR, Gudas TF, Rutkove SB, Raynor EM (1999) Electromyography and magnetic resonance imaging in the evaluation of radiculopathy.Muscle Nerve 22: 151-155.
- Robinson LR (1999) Electromyography, magnetic resonance imaging, and radiculopathy: it's time to focus on specificity.Muscle Nerve 22: 149-150.
- Guidelines in electrodiagnostic medicine. American Association of Electrodiagnostic Medicine.Muscle Nerve 15: 229-253.
- Caruso I, Lo Monaco M, Saraceni V (1983). Elettrodiagnosi di stimolazione. Rome; Pozzi L.
- Dahlin LB, Danielsen N, Ehira T, Lundborg G, Rydevik B (1986) Mechanical effects of compression of peripheral nerves.J BiomechEng 108: 120-122.
- Mogyororos I, Matthew C, Burke D (1996). Strength-duration properties of human peripheral nerve. Brain 119: 439-447.
- Siri E, Ljoka C, Mamone M, Foti C, Caruso I (2001). Definizionedeidatinormativi di rheobase, cronassia e quoziente di accomodazionenell’esameelettrodiagnostico: studio sperimentale. Europa Medicophysica 37: 73-75
- Harris R (1965). Chronaxy in Electrodiagnosis and electromyography(2nd edtn)Connectuit.
- Richardson AT, Wynn-Parry CB (1959). The theory and practice of electrodiagnosis. Ann. Phys. Med5: 248.
- Melo FP, Duringan J, Laurache L, Silva P, Lemos B, Fillo J et al. (2014) The measurement of chronaxie and Rheobase in patients with polyneuromyopathy of critical illness. Critical Care New Approaches. American Thoracic Society International Conference Abstract, San Diego.
- Ritchie AE (1954). Peripheral Nerve injuries. Stationery Office London
- Arid L. A companion in surgical studies, (2nd edtn), Livingstone London.
- Kanai K, Kuwabara S, Arai K, Sung JY, Ogawara K, et al. (2003) Muscle cramp in Machado-Joseph disease—altered motor axonal excitability properties and mexiletine treatment. Brain126(4):973
- Rydevik B, Nordborg C (1980) Changes in nerve function and nerve fibre structure induced by acute, graded compression.J NeurolNeurosurg Psychiatry 43: 1070-1082.
- Kurokawa H, Nakagawa I, Kubota M, Niinai H, Takezaki T, et al. (1996) [Electrophysiological examinations in Bell's palsy using electroneuronography and strength-duration curve].Masui 45: 842-845.
- Lauder TD, Dillingham TR, Andary M, Kumar S, Pezzin LE, et al. (2000) Predicting electrodiagnostic outcome in patients with upper limb symptoms: are the history and physical examination helpful?Arch Phys Med Rehabil 81: 436-441.
- Lauder TD, Dillingham TR, Andary M, Kumar S, Pezzin LE, et al. (2000) Effect of history and exam in predicting electrodiagnostic outcome among patients with suspected lumbosacral radiculopathy.Am J Phys Med Rehabil 79: 60-68.
Citation: Sokunbi OG, Nasir GM, Bukar GH, Abubakar A (2015) Influence of Lumbar Disc Herniation on Chronaxie and Rheobase in Patients with Chronic Low Back Pain-A Quasi Experimental Pilot Study. J Nov Physiother 5:256.
Copyright: © 2015, Sokunbi OG, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 14980
- [From(publication date): 4-2015 - Aug 29, 2025]
- Breakdown by view type
- HTML page views: 10311
- PDF downloads: 4669