Research Article Open Access
Instrumental Assessment of Balance Functional Performance. A Numerical Score to Discriminate Defective Subjects: A Retrospective Study
Michele Gallamini1,2*, Giorgio Piastra1,3, Debora Porzio1, Matteo Ronchi1, Fabio Scoppa4,5 and Franco Bertora6
1Ben-Essere Sport and Wellness Association Rapallo, Third-Sector Liguria Region Registry, Geneva, Italy
2Medical Devices R&D Consultant, Italy
3ASL4 Chiavarese (Liguria Regional Health Service) Via G. B. Ghio, 9-16043 Chiavari, Geneva, Italy, Sport Medicine, N.S. di Montallegro Hospital, Rapallo, Geneva, Italy
4Posturology, Medicine and Dental Surgery, Sapienza, University of Rome, Geneva, Italy
5Chinesis I.F.O.P. Osteopathy School, Rome, Italy
6IIT – Italian Institute of Technology, Genoa University, Italy
- *Corresponding Author:
- Michele Gallamini
Eng Freelance Researcher
Sal.Maggiolo di Nervi, 7-16167
Genova (GE), Italy
Tel: +39 010 3725061, +39 3355683177
E-mail: m.gallamini@ben-essere-asd.it
Received date: May 16, 2016; Accepted date: July 26, 2016; Published date: August 08, 2016
Citation: Gallamini M, Piastra G, Porzio D, Ronchi M, Scoppa F, et al. (2016) Instrumental Assessment of Balance Functional Performance. A Numerical Score to Discriminate Defective Subjects: A Retrospective Study. J Nov Physiother 6:305. doi: 10.4172/2165-7025.1000305
Copyright: © 2016 Gallamini M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Novel Physiotherapies
Abstract
Balance keeping is a key functional performance that becomes of crucial importance with increasing age when frailty makes falling a traumatic event. This functionality can be measured through several tests such as the Instrumented Romberg Test on a Force Platform. Many parameters and indicators obtained through this test have been proposed to quantify performance deficit and to point to possible aetiological causes. However, in spite of many studies, no final definition has been agreed upon. Rather, it seems that different combinations of strategies – probably in connection with anthropometrics, personal attitudes and lifestyle – can effectively solve the biomechanical problem of balance keeping. Such variability, in turn, entails a wide range of variability of all the individual parameters used to describe the path followed by the Center of Pressure over the force platform surface during the test. Ultimately, such a wide range makes the classical parameters rather undependable, when considered one by one, for clinical diagnostics. The diagnostic process in any case requires both a functionality assessment and, hopefully, reliable clues to achieve a deeper understanding of the dysfunction aetiology. A new heuristic approach has been proposed to develop a Score of Postural Functionality based on a reference population of healthy individuals. In this retrospective study, we applied this criterion in the analysis of the balance testing of 1626 compensated senior citizens. The Score has been compared to the most widely used balance indicators. The results do confirm the capability of this approach to quickly spot dysfunctional individuals with a high degree of sensitivity and specificity. The Score obtained seems potentially to show a correlation with the Risk-of-fall.
Keywords
Balance; Force platform; Risk of fall; Instrumented romberg test
Background and Purpose
The unintentional fall is a major concern worldwide: the most updated data reported by the US based CDC can be summarized as follows: “One out of three older adults (those aged 65 or older) falls each year but less than half talk to their healthcare providers about it. Among older adults, falls are the leading cause of both fatal and nonfatal injuries. In 2012, 2.4 million nonfatal falls among older adults were treated in emergency departments and more than 722,000 of these patients were hospitalized. In 2012, the direct medical costs of falls, adjusted for inflation, were $30 billion” [1].
Similar large figures also apply to the EU and undoubtedly motivate the EU program to extend the average life expectancy by 2 years by 2020 [2].
It is widely accepted that unintentional falls are primarily a geriatric pathology as it affects mostly individuals aged over 65 [3]. Doctor Rubenstein states that actually “Unintentional injuries are the fifth leading cause of death in older adults (after cardiovascular disease, cancer, stroke and pulmonary disorders), and falls constitute two-thirds of these deaths. In the United States, about three-fourths of deaths due to falls occur in the 13% of the population aged ≥ 65, indicative of primarily a geriatric syndrome. About 40% of this age group living at home will fall at least once each year, and about 1 in 40 of them will be hospitalised. Of those admitted to hospital after a fall, only about half will be alive a year later. Repeated falls and instability are very common precipitators of nursing home admission.”
It is still a controversial topic to state whether or not the Risk-Of- Fall (ROF) can be assessed through instrumental or clinical tools, in spite of many well-known studies by leading researchers like [4-9] and the accumulated evidence coming from current clinical practice.
MedLine shows an ever growing interest for the topic: by means of the search queries “risk of falls”, “risk of fall” and “Gait and Balance Disorders”, although probably with some partial overlapping, we found 32,322 indexed papers!
Besides the clinical assessment tools, which are very effective but to some extent exposed to subjective evaluation criteria, static and dynamic balance instrumental tests are increasingly being applied.
In this article, we wish to focus on the Static Balance Diagnostic process, proposing a simplified approach that can be closely related to the ROF assessment. We propose a numeric indicator that is obtained through processing well known balance parameters.
The Static Balance Assessment on the Force Platform
The force platform test
The force platform static balance test is a quantitative, instrumented version of the classic Romberg test [10]. It tests neurological function and is based on the premise that a person requires at least two of the three sensory channels involved in maintaining balance during quiet standing, namely proprioception, vestibular function, and vision. The analysis of force platform data (the sampled and digitized path of the Center of Pressure – COP) can provide a quick and reliable assessment of the main functionalities [11,12]. Actually, a number of “posturographic” parameters can be extracted from such data.
The “classical” parameters in the time domain (Sway Path, Sway Area, Mean and Max X,Y Oscillations); Parameters obtained from simple statistical analysis (area, size of the main and minor axes, and orientation of 95% confidence Ellipse) [13]; Parameters from power spectral density analysis [14]; Parameters from Sway “structural” analysis (Sway Density) [15]; Parameters derived from non-linear analysis models (Fractal Analysis, Neural Networks, Random Walk, etc.) [16-19].
However, the clinical interpretation of these parameters in the framework of a straightforward diagnostic process is far from clear for a number of reasons. The complexity of balance strategies [20] and intrinsic anthropometric variability [21], among other factors, in fact suggest different behaviours with different sway characteristics. An empirical alternative is a “functional” approach based on evaluating the degree of efficiency/effectiveness in maintaining balance and thus oriented towards assessing the “Risk-Of-Fall” (ROF) [22] and/or the energy expenditure in keeping upright stance [23].
On the other hand, one should also consider that subjects affected by a variety of neuromotor and neurosensory pathologies can often succeed in keeping upright balance and the corresponding sway patterns are likely to incorporate information about the adopted compensation strategies specific to the pathological situation.
The static balance diagnostic process
Although many clinically valuable suggestions may derive from thorough data examination, clinicians need and demand a short decision-making path. Even more so if, according to the requirement of massive screening programs, they are going to perform systematic screening of the large number of persons that, by age and/or other frailty indicators, might experience balance deficits.
To do so, it is perhaps worth restating the diagnostic process based on the balance assessment on the force platform. The process could be defined as the answer to three basic questions:
• Is a given subject functional or dysfunctional with respect to static balance keeping?
• If there is an indication of dysfunction, how significant is the impairment with regard to the ROF? III. In such a case, what indications can be provided for further clinical diagnostics?
With massive screening programs in mind, a quick and easy response would need to be found at least to the first and second question.
Clinical relevance
Given the prevalence of falls among senior citizens with the already stated burden of resulting pain, discomfort and even death, a strong effort has to be made to prevent such a catastrophic event. The first step is the massive screening of senior citizens to identify subjects at risk and hopefully address them to further more specific diagnostics and to clinical interventions. Among interventions there is the promotion of Physical Activities as a part of a healthier lifestyle in a true “Population Strategy” as defined [24]. Within ASL4 Chiavarese, back in 2008, an Adapted Physical Activity (APA) Program was started that has produced good results [25]. The program is run by the Ben- Essere ASD, a non-professional, nonprofit, sport Association under the supervision of ASL4 clinicians. The periodical functional assessment was then started as well. The lack of a numeric assessment index was greatly felt. By a more comprehensive score it would have been easier to perform a truly effective diagnostic screening service at least to provide an indication of subjects with some likelihood of Risk-of-Fall.
SPF: A Score of Postural Functionality
General
The large set of posturographic parameters cited above (and others that can be found in the literature in growing numbers) are for obvious reasons not unrelated as they come from the very same measurement of the ground reaction forces.
A typical approach that has been pursued in the past in order to face such information redundancy is to proceed by “pruning” or by “data compression”, aiming at the smallest possible set of de-correlated indicators. However, although this method can effectively represent in compact form the behaviour of a normal population of subjects, it is not selective enough to detect subtle differences in a variety of clinical conditions, also considering that most posturographic parameters defined in the literature have rather large variation coefficients that tend to blur the difference between normality and abnormality.
Consider, for example, two posturographic parameters that are strongly correlated in the normal population. Unless the correlation is a consequence of the underlying biomechanics of the sway movements, it expresses some (quasi) invariant feature of the motor command patterns in physiological conditions. It may happen, however, that the modifications of the motor control induced by some pathological conditions do not affect the two parameters in a statistically significant way, if considered separately, but are detectable if we observe their ratio, which in practice can be regarded as an additional, derived parameter or indicator. Such posturographic indicators will probably have a very small variation coefficient in the normal population and thus may be quite sensitive to pathological conditions.
This is the heuristic basis for our proposal of a new evaluation scale, namely a Score of Postural Functionality (SPF) that exploits the hidden information underlying a redundant set of posturographic parameters. The idea is to count the number of ‘postural anomalies’ over the extended set of parameters, in relation to a reference population of subjects, and to define SPF as the relative number of anomalies: the higher the score the worse the balance control efficiency. Then, by plotting the relative probability of occurrence of the scores obtained by SPF it should be possible to define the best cut-off value to discriminate functional vs. dysfunctional subjects. The proposed procedure is explained in detail in the following sections.
Discrimination of a dysfunctional population from the reference population by means of the ROC curves
A Receiver Operating Characteristic (ROC) is a mathematical model in communication theory developed in the 50’s for the purpose of extracting information from radio signals contaminated by noise. In the 1960s ROC curves began to be used in psychophysics, to assess human detection of weak signals. More recently, it has become clear that they are remarkably useful in medical decision-making [26-28]. In signal detection theory, a ROC is a graphical plot of the sensitivity vs. specificity for a binary classifier system as the discrimination threshold is varied. ROC curves can also be interpreted as the plot of the fraction of true positives (TP) vs. the fraction of false positives (FP) in the decision making process [29].
The best possible discrimination/classification method would yield a graph that was a point in the upper left corner of the ROC space, i.e. 100% sensitivity (all true positives are found) and 100% specificity (no false positives are found). A completely random predictor would give a straight line at an angle of 45 degrees from the horizontal, from bottom left to top right: this is because, as the threshold is raised, equal numbers of true and false positives would be let in.
The ROC curve is frequently used to derive summary nonparametric statistics. In particular, a very common statistical parameter is the AUC (Area under the ROC curve) which is 1 in the optimal case and 0.5 for a random discrimination. The ROC curve can be used to choose the best operating point. The usual criterion is to consider the best trade-off between the costs of failing to detect positives and the costs of raising false alarms. These costs need not be equal. However, this is a common assumption and the typical cost function associated with classification is a simple sum of the cost of misclassifying positive and negative cases: C=K1*FP+K2*(1-TP) where C is Cost, FP stands for False Positives and TP stands for True Positives.
In defining the SPF the idea was therefore not only to define a method, but also to propose a reference value as a statistical best significant cut-off value to discriminate among Normo-Functional and Dys-Functional individuals.
Materials and Methods
This study was performed in two phases:
• SPF definition and reference set;
• Clinical verification of the SPF vs. standard parameters in a cohort of autonomous senior citizens.
Phase 1-SPF definition
The sample for SPF definition: The posturographic data during quiet standing were collected from a reference population that included healthy normal people and top-performing athletes in different sport disciplines. The consistency and reliability of the extended set of posturographic parameters was evaluated in the reference population, which consisted of 195 healthy, young subjects, 119 of them athletes engaged in different sport disciplines at excellence level.
The anthropometric parameters of the reference population are reported in Table 1. All subjects were duly informed and provided written consent to take part in the study.
| Sport specialty | Number | Age (y) | Weight (kg) | Height (m) |
|---|---|---|---|---|
| None | 76 | 33.17 7.02 | 65.71 15.31 | 1.68 0.10 |
| Basket | 17 | 29.53 7.05 | 98.47 16.11 | 2.00 0.08 |
| Karate | 27 | 24.63 4.62 | 56.96 8.20 | 1.73 0.09 |
| Ski | 43 | 16.09 1.56 | 59.93 9.75 | 1.72 0.09 |
| Swim | 32 | 18.00 4.87 | 54.78 8.58 | 1.73 0.13 |
| Total | 195 | 25.42 9.15 | 64.29 16.93 | 1.73 0.13 |
Table 1: Reference population anthropometrics for SPF definition.
All Subjects performed the Romberg Test over a Force Platform (ARGO – RGMD SpA – Genoa – Italy). Table 2 reports the functional characteristics of the platform (Figure 1) and the test conditions.
| Main Characteristics | |
|---|---|
| Platform Size | 600× 600 mm |
| Weight Range | 15 to 200 Kg |
| Type of sensors | Strain Gauges |
| Output | COP Position (x,y) vs. time |
| COP accuracy | <0.2 mm |
| Sampling Rate | 100 Hz |
| Data Processing | The trajectory of the COP is low-pass filtered with a 2nd order Butterworth filter (cutoff frequency 12.5 Hz). |
| Main Output Parameters | Sway Path, Sway Area, AP and ML Oscillations, 95% Confidence Ellipse, Harmonic analysis of x-y components in 8 bands, Sway Density. |
| Display | Stabilogram, Statokinesiogram, Spectral Analysis. |
| Mechanical Bandpass | >100 Hz |
| Test Mode | |
| Recording | 45 sec (first 5 sec not considered in parameter calculation) |
| Test Sequence | Closed Eyes, then Open Eyes |
| Feet position | Barefoot – Feet Joined and parallel |
| Arms | Hanging loose at sides |
| Mouth | Closed, unclenched teeth |
| Environmental | As defined by Kaptein et al. (1983) [27] |
Table 2: ARGO force platform characteristics and test mode.
Processing of the posturographic data: From the raw data delivered by the force platform, namely the readings of four calibrated force transducers, the time course of the two components of the COP or posturographic traces (x: Medio-Lateral; y: Antero-Posterior) was evaluated. The two traces could be analysed separately or in combination by considering the statokinesigram, namely the layout of a line connecting the successive positions of the centre of pressure during the recording, ultimately obtaining a geometrical figure. During posturographic analysis 27 parameters were extracted from both the posturograhic traces and the statokinesigram. The parameters can be subdivided into two main classes, namely global parameters (either in the time or the frequency domain) and structural parameters (resulting from the breakdown of the sway patterns into sub-patterns). They are defined as follows:
9 global parameters:
• AP, ML [mm]: Range of the posturographic traces in the two directions, antero-posterior (AP) and medio-lateral (ML), respectively;
• SP [mm/s]: Length of the Sway Path, normalized with respect to the duration of the acquisition interval (it is equivalent to the average speed of the posturographic path);
• SA [mm2/s]: Area swept by the radius connecting each subsequent point of the statokinesigram to the average position of the COP, normalized with respect to the duration of the acquisition interval;
• EA, Emin, Emax [mm2, mm, mm]: The area and the two radii of the ellipse that contains 95% (±2σ) of the samples of the statokinesigram;
• Jx, Jy [mm/s3 ]: Measure of the smoothness of the statokinesigram, estimated by means of the average jerk integral in the two main directions (x=ML, y=AP);
16 frequency domain parameters:
• 1x/1y [mm2]: Spectral energy of the two components of the posturogram, in the frequency band 1 (0.01-0.1 Hz);
• 2x/2y [mm2]: Spectral energy of the two components of the posturogram, in the frequency band 2 (0.1-0.25 Hz);
• 3x/3y [mm2]: Spectral energy of the two components of the posturogram, in the frequency band 3 (0.25-0.35 Hz);
• 4x/4y [mm2]: Spectral energy of the two components of the posturogram, in the frequency band 4 (0.35-0.5 Hz);
• 5x/5y [mm2]: Spectral energy of the two components of the posturogram, in the frequency band 5 (0.5-0.75 Hz);
• 6x/6y [mm2]: Spectral energy of the two components of the posturogram, in the frequency band 6 (0.75-1 Hz);
• 7x/7y [mm2]: Spectral energy of the two components of the posturogram, in the frequency band 7 (1-3 Hz);
• 8x/8y [mm2]: Spectral energy of the two components of the posturogram, in the frequency band (3-10 Hz);
Structural parameters: The topological structure of the sway patterns was analysed by means of the Sway Density Curve (SDC), which has been defined [15,30] as the time-dependent curve that counts, for each time instant, the number of consecutive samples of the statokinesigram falling inside a circle with a suitably small radius.
This curve was low-pass filtered (cut-off frequency 2.5 Hz) in order to identify the sequence of peaks, from which we extracted the following SDC parameters:
• SD [mm]: Mean Spatial Distance, i.e. the average displacement of the COP trace between one peak of the SDC and the next one;
• ST [s]: Mean Stay Time, i.e. the average time spent by the COP trace in the neighbourhood of each peak, over the observed sway of each subject: it is proportional to the height of the peak of the SDC curve.
Results: Table 3 shows the mean values and ranges (±2σ) of the 27 basic or classical posturographic parameters defined above in the reference population of subjects, in the two experimental conditions, namely Open Eyes (OE) and Closed Eyes (CE).
| Nr. | Parameter | Open Eyes value | Closed Eyes value |
|---|---|---|---|
| 1 | AP [mm] | 20.85 6.35 | 29.41 9.09 |
| 2 | ML [mm] | 20.55 5.80 | 31.75 9.22 |
| 3 | Sp [mm/s] | 11.38 2.90 | 20.14 6.96 |
| 4 | Sa [mm2/s] | 18.80 8.12 | 47.03 26.75 |
| 5 | Ea [mm2] | 190.77 104.65 | 374.87 198.92 |
| 6 | Emin [mm] | 6.24 1.56 | 9.14 2.37 |
| 7 | Emax [mm] | 9.22 2.92 | 12.35 3.56 |
| 8 | Jx [mm/s3] | 99.22 34.7 | 183.19 85.85 |
| 9 | Jy [mm/s3] | 136.80 76.26 | 208.52 107.96 |
| 10 | 1st Harmonic Band X [mm2] | 180.49 202.55 | 241.78 338.09 |
| 11 | 1st Harmonic Band Y [mm2] | 246.64 257.63 | 313.07 319.69 |
| 12 | 2nd Harmonic Band X [mm2] | 48.5635.85 | 112.37 76.54 |
| 13 | 2nd Harmonic Band Y [mm2] | 47.19 43.94 | 88.27 59.12 |
| 14 | 3rd Harmonic Band X [mm2] | 24.99 16.49 | 81.09 58.56 |
| 15 | 3rd Harmonic Band Y [mm2] | 20.8 16 | 59.06 41.19 |
| 16 | 4th Harmonic Band X [mm2] | 14.24 10.12 | 46.55 32.56 |
| 17 | 4th Harmonic Band Y [mm2] | 12.98 10.12 | 37.38 26.8 |
| 18 | 5th Harmonic Band X [mm2] | 7.54 4.76 | 23.77 19.51 |
| 19 | 5th Harmonic Band Y [mm2] | 5.4 3.44 | 19.65 15.82 |
| 20 | 6th Harmonic Band X [mm2] | 4.74 3.76 | 15.66 14.76 |
| 21 | 6th Harmonic Band Y [mm2] | 3.27 3.00 | 9.44 8.72 |
| 22 | 7th Harmonic Band X [mm2] | 0.66 0.41 | 2.34 1.96 |
| 23 | 7th Harmonic Band Y [mm2] | 0.49 0.35 | 1.43 1.36 |
| 24 | 8th Harmonic Band X [mm2] | 0.01 0.01 | 0.02 0.02 |
| 25 | 8th Harmonic Band Y [mm2] | 0.01 0.01 | 0.03 0.05 |
| 26 | Mean Spatial Distance [mm] | 3.33 1.01 | 7.18 2.57 |
| 27 | Mean Stay Time [sec] | 1.17 0.37 | 0.63 0.24 |
Table 3: Basic posturographic parameters in the reference population of subjects.
Extending the basic set of posturographic parameters with posturographic indicators: Given the great intrinsic variability of the basic parameters of Table 3, they can hardly be relied on in order to form a diagnostic pattern. As an example, while no one denies the significance of the Romberg Test, whether the results of balance assessments can be interpreted as a “Risk-Of-Fall” (ROF) indicator or not is still being debated [31,32].
With specific reference to the force platform test, however, there is a consensus that stabilization is an active, not a passive process. This process integrates in complex ways different sources of information, complex control arrangements (including proprioceptive feed-back and feed-forward anticipatory actions), generated in an intermittent way [33-38].
From a clinical perspective it is however important to evaluate the effectiveness and efficiency of balance keeping in upright unperturbed stance and, observing that also heavily impaired subjects can often perform this task and are indeed maintaining such a stance in daily living activities, we have to assume that the COP Path very likely carries the information we seek. By considering the wide range of biomechanical parameters that can affect motor control and the extremely flexible range of interactive learning [39,40], it may be postulated that different combinations of motor strategies could well achieve unperturbed upright stance and such “strategies” could be apparent in combinations of basic parameters or posturograhic indicators.
To define and estimate such indicators, we first computed the correlation coefficients between all the pairs of the set of 27 basic parameters defined above in the reference population of healthy subjects: in this way we obtained 351 values, for both the Open Eyes [OE] and Closed Eyes [CE] conditions, with a total of 702 correlation values.
The posturographic indicators were then defined as the ratios of basic parameters whose correlation coefficient is sufficiently high (in absolute value, because we are not interested in distinguishing between positive and negative correlation). Empirically, we found that 0.7 is a good choice for the correlation threshold in terms of stability of the results. We found that 36 out of 702 were the parameter ratios with a correlation coefficient greater than the 0.7 threshold in at least one of the two experimental conditions (OE and CE). These indicators are listed in Table 4. In particular, 16 of them are above threshold in conditions, 10 only in the OE condition and 10 only in the CE condition.
| Nr.(*) | Abbr. | Description | Â Â Â Â Â Â Â Â Â R | |
|---|---|---|---|---|
| OE | CE | |||
| 28 | EA/Emin | Ellipse Area/Ellipse Minor Axis | 0.93 | 0.94 |
| 29 | EA/Emax | Ellipse Area/Ellipse Major Axis | 0.9 | 0.91 |
| 30 | SP/MD | Sway Path/Mean Spatial Distance | 0.72 | 0.9 |
| 31 | SA/SP | Sway Area/Sway Path | 0.75 | 0.89 |
| 32 | EA/SA | Ellipse Area/Sway Area | 0.79 | 0.85 |
| 33 | EA/ML | Ellipse Area/Medio Lateral Oscillation | 0.73 | 0.82 |
| 34 | Emax/AP | Ellipse Major Axis/Antero Posterior Oscillation | 0.7 | 0.71 |
| 35 | SA/Emax | Sway Area/Ellipse Major Axis | 0.74 | 0.81 |
| 36 | 1Y/Emin | First Y Band Harmonic Pwr/Ellipse Minor Axis | 0.79 | 0.72 |
| 37 | EA/AP | Ellipse Area/Antero Posterior Oscillation | 0.78 | 0.75 |
| 38 | Emax/ML | Ellipse Major Axis/Medio Lateral Oscillation | 0.74 | 0.78 |
| 39 | SA/Emin | Sway Area/Ellipse Minor Axis | 0.76 | 0.78 |
| 40 | Emin/AP | Ellipse Minor Axis/Antero Posterior Oscillation | 0.77 | 0.7 |
| 41 | Emax/Emin | Ellipse Major Axis/Ellipse Minor Axis | 0.71 | 0.76 |
| 42 | 1Y/EA | 1st Y Band Harmonic Pwr / Ellipse Area | 0.73 | 0.72 |
| 43 | Jx/7X | Jerk X/7th Band X Harmonic Pwr | 0.72 | 0.76 |
| 44 | SP/ST | Sway Path/Mean Stay Time | 0.8 | |
| 45 | MD/ST | Mean Spatial Distance/Mean Stay Time | 0.77 | |
| 46 | Jx/SP | Jerk X/Sway Path | 0.8 | |
| 47 | SP/7X | Sway Path/7th Band X Harmonic Pwr | 0.77 | |
| 48 | SA/MD | Sway Area/Mean Spatial Distance | 0.76 | |
| 49 | 1Y/AP | First Y Band Harmonic Pwr/Antero Posterior Oscillation | 0.75 | |
| 50 | SP/7Y | Sway Path/7th Band Y Harmonic Pwr | 0.73 | |
| 51 | SA/AP | Sway Area/Antero Posterior Oscillation | 0.72 | |
| 52 | 7Y/8Y | 7th Band Y Harmonic Pwr/8th Band Y Harmonic Pwr | 0.72 | |
| 53 | Jy/SP | Jerk Y/Sway Path | 0.70 | |
| 54 | Jx/8X | Jerk X/8th Band X Harmonic Pwr | 0.82 | |
| 55 | SA/ML | Sway Area/Medio Lateral Oscillation | 0.79 | |
| 56 | MD/5Y | Mean Spatial Distance/5th Band Y Harmonic Pwr | 0.79 | |
| 57 | Emin/ML | Ellipse Minor Axis/Medio Lateral Oscillation | 0.78 | |
| 58 | 6X/7X | 6th Band X Harmonic Pw /7th Band X Harmonic Pwr | 0.78 | |
| 59 | SA/7Y | Sway Area/7th Band Y Harmonic Pwr | 0.77 | |
| 60 | MD/7X | Mean Spatial Distance/7th Band X Harmonic Pwr | 0.77 | |
| 61 | SA/5Y | Sway Area/5th Band Y Harmonic Pwr | 0.75 | |
| 62 | MD/6Y | Mean Spatial Distance/6th Band Y Harmonic Pwr | 0.75 | |
| 63 | Jx/Jy | Jerk X/Jerk Y | 0.75 | |
| (*) To be added to the 27 basic parameters listed in Table 3 | ||||
Table 4: Correlation index for derived parameters.
The table also shows that in general the correlation is higher in the CE than in the OE condition, in particular in most parameters that are above threshold in both conditions. This difference may be interpreted as a “simplification” of the control patterns that become more stereotyped when the subjects are deprived of the information coming from the visual channel.
From the evidence provided in Table 4, we could extend the set of 27 basic posturographic parameters by adding the list of 36=16+10+10 derived parameters or posturographic indicators, with an overall total of 63 parameters.
The derived parameters may be expected to have a variation coefficient (VC=standard deviation/mean) generally smaller than the basic parameters. This is indeed what actually happens: Table 5 shows the list of the 10 posturographic parameters with the smallest VC and 9 of them are indeed derived parameters.
| Parameter | VC (%) | ||
|---|---|---|---|
| 1 | Emin/ML | Ellipse Minor Axis/Medio Lateral Oscillation | 18.08 |
| 2 | Emin/AP | Ellipse Minor Axis/Antero Posterior Oscillation | 19.14 |
| 3 | Jx/SP | Jerk X/Sway Path | 19.74 |
| 4 | SP/MD | Sway Path/Mean Spatial Distance | 20.66 |
| 5 | Emax/AP | Ellipse Major Axis/Antero Posterior Oscillation | 20.68 |
| 6 | Emax/Emin | Ellipse Major Axis/Ellipse Minor Axis | 23.05 |
| 7 | Emin | Ellipse Minor Axis | 24.92 |
| 8 | EA/Emax | Ellipse Area/Ellipse Major Axis | 24.92 |
| 9 | Jx/Jy | Jerk X/Jerk Y | 25.51 |
| 10 | SP | Sway Path | 25.52 |
Table 5: List of the 10 parameters showing the least variation coefficient (VC).
Computing a score of postural functionality: For each parameter of the extended set of 63, the mean value μi and the standard deviation σi were computed in both conditions (OE and CE, respectively). The collection of all the (μi, σi) pairs of values is denominated reference posturographic dataset: one dataset (63 values) for the OE condition and another dataset (63 values) for the CE condition.
These datasets can be used to characterize the postural behaviour of any given normal subject or clinical patient. First of all, a confidence interval Δi is defined for each parameter:
Δi : μi ± 2σi (1)
(1) A “Posturographic Anomaly” is then defined as the occurrence of a posturographic parameter pi outside the corresponding confidence interval:
pi ∉ Δi (2)
(2) From this the Score of Postural Functionality [SPF] of a given subject was defined as the Number of observed Posturographic Anomalies. By definition, SPF ranges between 0 and 63:
0 ≤ SPF ≤ 63 (3)
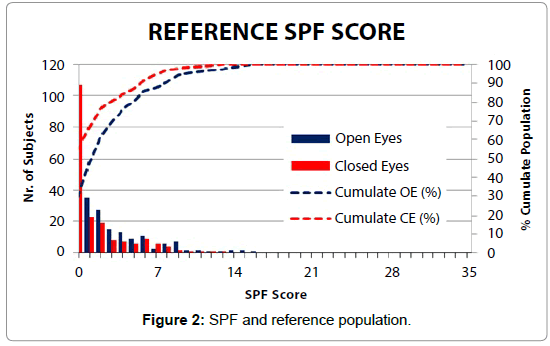
SPF and the ROC curve: With the extended set of parameters, we can compute the SPF: the graph of Figure 2 shows the distribution of SPF in the Closed and Open Eyes Test Conditions and the corresponding cumulative probability. SPF is under 9 for over 95% of the reference population of subjects.
By plotting the SPF cumulative value in a normalized graph (0- 100% of Subjects and 0-100% of SPF), it is easy to pinpoint a “knuckle” or cut-off point affording the best compromise between sensitivity (Positive/True Positive) and specificity (Negative/True Negative).
Recalculating the SPF cumulative values as a percentage and plotting them in a graph affording the same scale for the X and Y axes, the “best” cut-off value is the closest point to the ideal point (X=0, Y=100) that corresponds to the condition in which there are no false alarms and all true positives are detected.
This is of course under the assumption that sensitivity and specificity have an equal rating. This point seems to correspond to SPF = 9.
The basic suggestion for its clinical application is therefore that an SPF value in excess of 9 in any of the two conditions might be a positive indication of a dys-function warranting a further diagnostic effort. The whole process is summarized in the Flow-Chart of Table 6.
| 1 | A reference population of most likely, Balance-wise, “Functional” individuals was submitted to the standard Test providing 27 “Classical” Parameters with a resulting set of reference values (Mean ±2ÏÂ?). |
| 2 | The possible combinations of the 27 parameters are 351 in each of the two tests (Closed Eyes andOpen Eyes) for a total of 702 Ratios |
| 3 | Given the Pearson Correlation test to the combinations, 36 ratios were selected because showing a correlation coefficient greater of 0.7 |
| 4 | For each of the 27+36 values obtained testing the Reference population it was defined the reference interval (Mean ±2ÏÂ?). |
| 5 | SPF is then calculated as the number of out of range values |
| 6 | Through ROC criteria the Threshold of SPF=9 was defined as the one under which lies over 95% of reference population |
Table 6: SPF definition flow-chart.
Phase 2-SPF field test
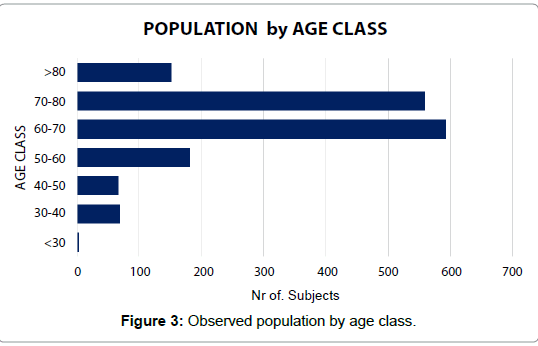
The sample: In close cooperation with ASL4 Chiavarese (Liguria Regional Health Service) an extensive test was performed on a population of 1,626 subjects, aged 21 to 104 years (for full anthropometric data, see Table 7 and Figure 3).
| Age Range | Nr | Median Age (years) | Median Height (cm) | Median Weight (Kg) |
|---|---|---|---|---|
| <30 | 4 | 67.41 | 158.58 | 66.36 |
| 30-40 | 69 | |||
| 40-50 | 67 | |||
| 50-60 | 182 | |||
| 60-70 | 593 | |||
| 70-80 | 559 | |||
| >80 | 152 | |||
| Total Population | 1,626 | |||
Table 7: Main anthropometrics of the observed population.
All the subjects:
• Were autonomous and self-sufficient and could be rated as “compensated”,
• Were taking part in an Adaptive Physical Activity (APA) Program performed by Ben-Essere A.S.D. in cooperation with ASL 4 Chiavarese and could therefore be rated as functionally “Autonomous”;
• Were duly informed and provided formal written consent to the test;
• Received the Balance Test with the ARGO balance platform according to the test standards given in Table 2.
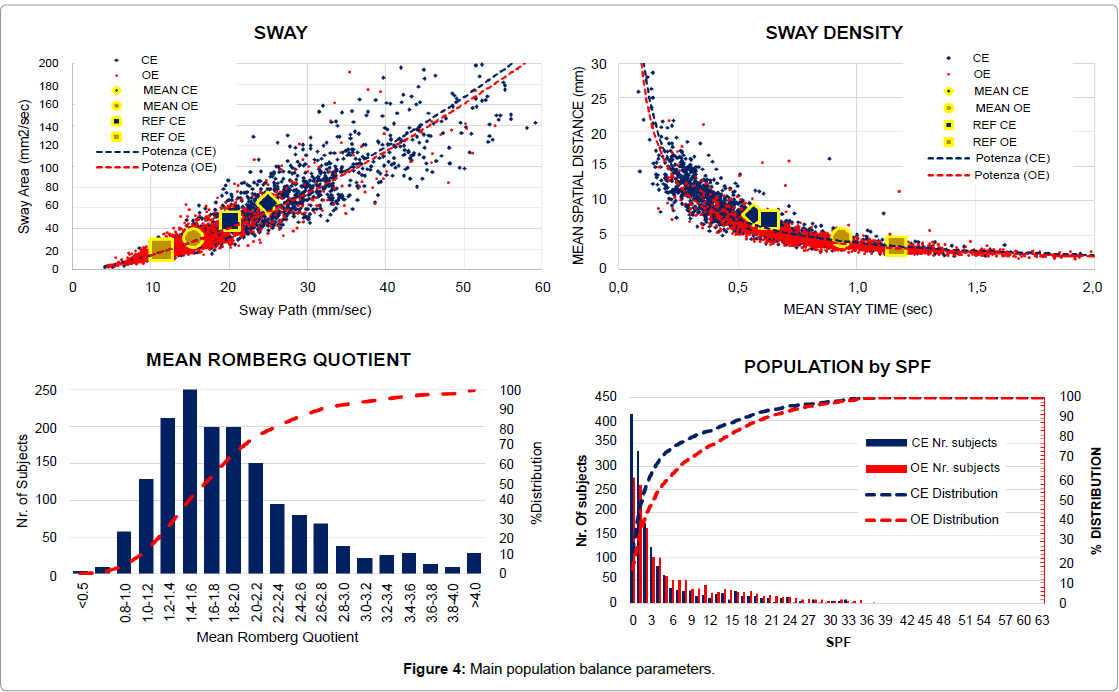
Balance parameters: Population data were plotted both on the Sway Plane (Sway Area vs. Sway Path) and on the Sway Density Plane (Mean Spatial Distance vs. Mean Stay Time) in both Open and Closed Eyes conditions (Figure 4). In the graphs both the Average and the Reference Standard Values (Std. Dev indicated as Error Bars) are also plotted for both Open and Closed Eyes tests.
a) Both the Sway Parameters (Sway Path (SP) and Sway Area (SA)) and the Sway Density Parameters (Mean Stay Time (ST) and Mean Spatial Distance (SD) do show a consistent intercorrelation (> 0.81 for Open Eyes and >0.84 for Closed Eyes) in a Power Relationship where
SA=0.4×SP1.5 and SD=3.9×ST-0.9
Such stable relationships possibly indicate the relationships between the Sway parameters and the Postural Tone [41], and between the Sway Density Plot and the “impulsive” motor control activities [36,37,42].
b) The average values are very close to Reference values: all the mean values – except Sway Path and Sway Area Open Eyes, which are slightly higher – are within ± 1σ of Reference values, thus confirming the validity of the Reference itself as Normality Values;
c) The larger Std.Dev. afforded by the population data is mainly obtained from subjects well outside the 2σ “Confidence Level” as a result of defective performances in a rather un-symmetrical distribution as shown for the Average Romberg quotient (Average between Sway Path, Sway Area, Ellipse Area, Mean Spatial Distance and Mean Stay Time(*) Quotients).
(*) The Romberg quotient in the Mean Stay Time was calculated reciprocally (Open Eyes/Closed Eyes) because for this parameter “the higher the better” unlike all the other balance parameters.
The score of postural functionality:
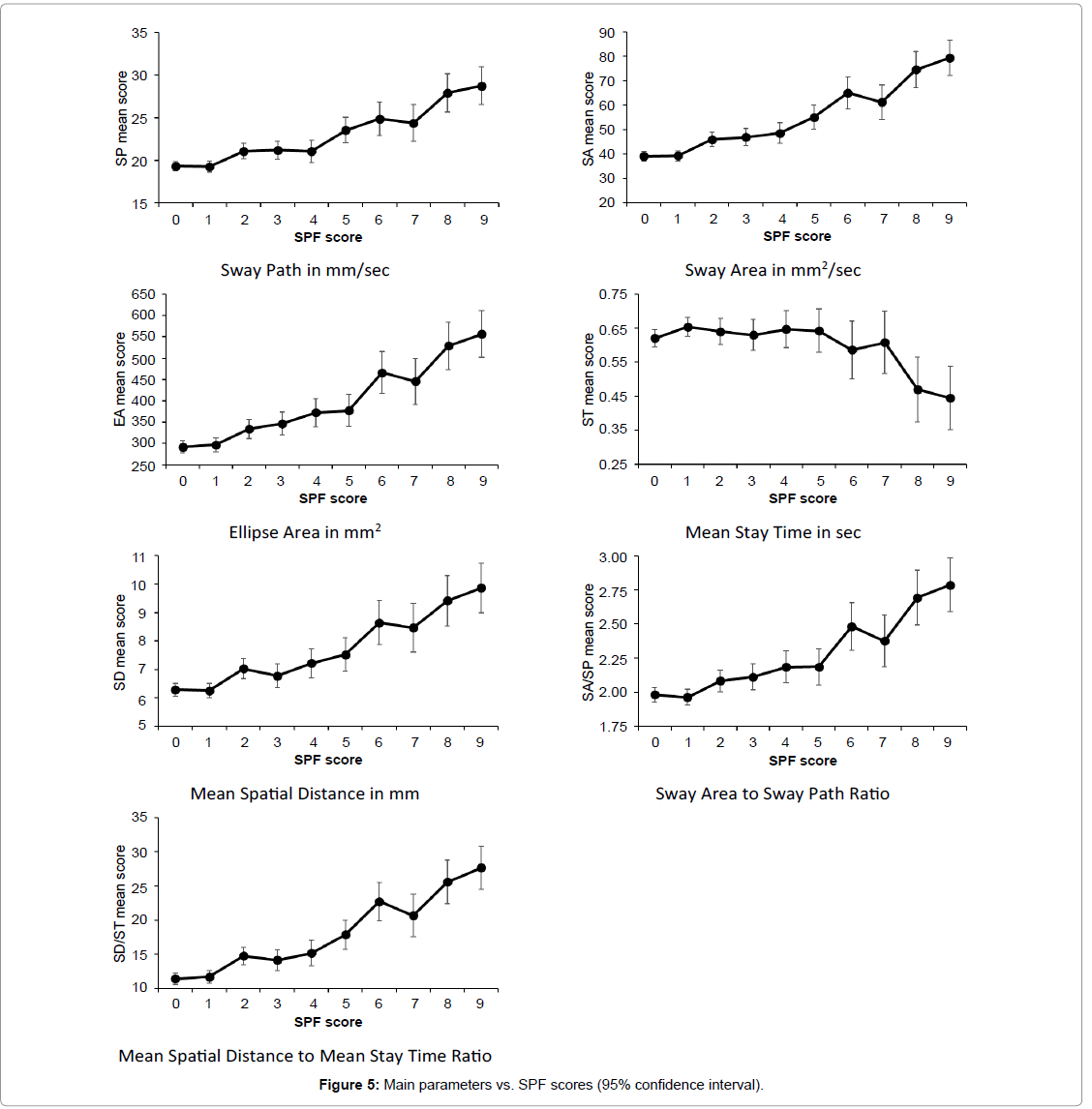
Statistical analysis of SPF significance: We tested the association of Closed Eyes SPF scores with scores on the main parameters. We adopted a twofold approach. First, we computed the correlations of SPF scores with raw scores on the parameters, with recoded scores (as described in Section 6.1.5), and with recoded scores after adjustment for the inflation of the statistic due to main parameters being part of the SPF score. Second, we tested the significance of differences in scores on the main parameters between groups defined by below-threshold SPF scores.
Mean comparisons were performed through analyses of variance (ANOVAs). They were all significant (p<0.001), with at least moderate (η2>0.06) effect sizes, except ST, which showed a small effect size (η2=0.02). To test differences in scores on the main parameters between groups defined by below-threshold SPF scores we performed analyses of variance.
Correlations are reported in Panel 1 as well as results of the omnibus test (Panel 2). Post-hoc comparisons were performed with the adaptive [43] step-up false discovery rate-controlling procedure in order to control the inflation of the probability of making at least one Type I error due to multiple comparisons. Results are reported in Panel 3 and Figure 5.
| Parameter | raw scores r | unadjusted recoded | adjusted recoded scores r |
|---|---|---|---|
| scores r | |||
| Sway Path (SP) | 0.79*** | 0.59*** | 0.57*** |
| Sway Area (SA) | 0.84*** | 0.63*** | 0.62*** |
| Area of the 95% Confidence Ellipse | 0.77*** | 0.61*** | 0.60*** |
| Mean Stay Time (ST) | -0.43*** | -0.04 | -0.07 |
| Mean Spatial Distance (SD) | 0.75*** | 0.57*** | 0.55*** |
| SA/SP | 0.71*** | 0.56*** | 0.54*** |
| SD/ST | 0.79*** | 0.55*** | 0.53*** |
| Note: ***: p<0.001; **: p<0.01; ***: p<0.05. | |||
Panel 1: Correlation between SPF and parameters.
| Parameter | F(9,1307) | Effect size h2 |
|---|---|---|
| Sway Path (SP) | 19.55*** | 0.12 |
| Sway Area (SA) | 32.57*** | 0.18 |
| Area of the 95% Confidence Ellipse | 24.37*** | 0.14 |
| Mean Stay Time (ST) | 3.45*** | 0.2 |
| Mean Spatial Distance (SD) | 18.25*** | 0.11 |
| SA/SP | 16.88*** | 0.10 |
| SD/ST | 28.53*** | 0.16 |
| Note: ***: p<0.001; **: p<0.01; ***: p<0.05. h2<0.01: negligible effect size (ES); 0.01<h2<0.06: small ES; 0.06<h2<0.14: moderate ES; h2>0.14: large ES. | ||
Panel 2: Results of the omnibus test.
| Mean comparisons of scores on main parameters between groups defined by below-threshold SPF scores: p-values of post-hoc comparisons, after adjustment for multiple comparisons, performed with the adaptive Benjamini and Hochberg (2000) step-up false discovery rate-controlling procedure. The darker the color, the more statistically significant the difference. | ||||||||||||||||||||
| Sway Path | Sway Area | |||||||||||||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |||
| 0 | 0.93 | 0.003 | 0.004 | 0.022 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0 | 0.908 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |
| 1 | 0.003 | 0.004 | 0.021 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 1 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |||
| 2 | 0.918 | 0.982 | 0.009 | 0.002 | 0.009 | <0.001 | <0.001 | 2 | 0.703 | 0.372 | 0.003 | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| 3 | 0.918 | 0.017 | 0.003 | 0.015 | <0.001 | <0.001 | 3 | 0.586 | 0.011 | <0.001 | 0.001 | <0.001 | <0.001 | |||||||
| 4 | 0.019 | 0.003 | 0.015 | <0.001 | <0.001 | 4 | 0.061 | <0.001 | 0.004 | <0.001 | <0.001 | |||||||||
| 5 | 0.347 | 0.619 | 0.003 | <0.001 | 5 | 0.019 | 0.183 | <0.001 | <0.001 | |||||||||||
| 6 | 0.81 | 0.055 | 0.015 | 6 | 0.464 | 0.067 | 0.005 | |||||||||||||
| 7 | 0.032 | 0.009 | 7 | 0.013 | 0.001 | |||||||||||||||
| 8 | 0.692 | 8 | 0.389 | |||||||||||||||||
| Ellipse Area | Mean Stay Time | |||||||||||||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |||
| 0 | 0.67 | 0.003 | 0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0 | 0.193 | 0.682 | 0.847 | 0.682 | 0.774 | 0.761 | 0.875 | 0.012 | 0.004 | |
| 1 | 0.012 | 0.003 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 1 | 0.774 | 0.682 | 0.875 | 0.847 | 0.339 | 0.682 | 0.003 | 0.001 | |||
| 2 | 0.517 | 0.072 | 0.063 | <0.001 | <0.001 | <0.001 | <0.001 | 2 | 0.847 | 0.877 | 0.946 | 0.585 | 0.774 | 0.007 | 0.003 | |||||
| 3 | 0.268 | 0.219 | <0.001 | 0.002 | <0.001 | <0.001 | 3 | 0.847 | 0.847 | 0.682 | 0.847 | 0.012 | 0.004 | |||||||
| 4 | 0.834 | 0.003 | 0.03 | <0.001 | <0.001 | 4 | 0.939 | 0.576 | 0.774 | 0.009 | 0.003 | |||||||||
| 5 | 0.007 | 0.052 | <0.001 | <0.001 | 5 | 0.645 | 0.774 | 0.012 | 0.004 | |||||||||||
| 6 | 0.603 | 0.114 | 0.022 | 6 | 0.847 | 0.193 | 0.089 | |||||||||||||
| 7 | 0.045 | 0.007 | 7 | 0.125 | 0.052 | |||||||||||||||
| 8 | 0.525 | 8 | 0.847 | |||||||||||||||||
| Mean Spatial Distance | Sway Area / Sway Path | |||||||||||||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |||
| 0 | 0.84 | 0.001 | 0.058 | 0.002 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0 | 0.645 | 0.052 | 0.027 | 0.004 | 0.01 | <0.001 | <0.001 | <0.001 | <0.001 | |
| 1 | 0.001 | 0.051 | 0.002 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 1 | 0.027 | 0.014 | 0.002 | 0.005 | <0.001 | <0.001 | <0.001 | <0.001 | |||
| 2 | 0.416 | 0.59 | 0.194 | 0.001 | 0.004 | <0.001 | <0.001 | 2 | 0.645 | 0.187 | 0.223 | <0.001 | 0.011 | <0.001 | <0.001 | |||||
| 3 | 0.231 | 0.058 | <0.001 | 0.001 | <0.001 | <0.001 | 3 | 0.398 | 0.423 | 0.001 | 0.027 | <0001 | <0.001 | |||||||
| 4 | 0.483 | 0.004 | 0.022 < | 0.001 | <.001 | 4 | 0.989 | 0.01 | 0.13 | <0.001 | <0.001 | |||||||||
| 5 | 0.037 | 0.094 | 0.001 | <.001 | 5 | 0.014 | 0.146 | <0.001 | <0.001 | |||||||||||
| 6 | 0.781 | 0.231 | 0.057 | 6 | 0.455 | 0.148 | 0.033 | |||||||||||||
| 7 | 0.162 | 0.037 | 7 | 0.033 | 0.007 | |||||||||||||||
| 8 | 0.514 | 8 | 0.55 | |||||||||||||||||
| Mean Spatial Distance / Mean Stay Time | ||||||||||||||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | ||||||||||||
| 0 | 0.69 | <.001 | 0.003 | 0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |||||||||||
| 1 | <.001 | 0.009 | 0.002 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||||||||||||
| 2 | 0.551 | 0.727 | 0.019 | <0.001 | 0.001 | <0.001 | <0.001 | |||||||||||||
| 3 | 0.424 | 0.007 | <0.001 | <0.001 | <0.001 | <0.001 | ||||||||||||||
| 4 | 0.075 | <0.001 | 0.004 | <0.001 | <0.001 | |||||||||||||||
| 5 | 0.009 | 0.165 | <0.001 | <0.001 | ||||||||||||||||
| 6 | 0.376 | 0.219 | 0.028 | |||||||||||||||||
| 7 | 0.038 | 0.003 | ||||||||||||||||||
| 8 | 0.396 | |||||||||||||||||||
Panel 3: Significance of SPF differences.
Taken together, these results suggest that the SPF score is able to discriminate between different levels of impairment, as measured by main parameters. However, the ST score seem to be less consistent than the other main parameters.
SPF sensitivity: The SPF plots of the field test population do confirm the presence of quite a few “dysfunctional” subjects. While the SPF distribution in the Normal Sample indicates just 5% of subjects with a score in excess of 9, in our population we had:
• 309 (19%) subjects with Closed Eyes SPF score>9 and
• 472 (29%) subjects with Open Eyes SPF score>9.
Such a difference can be physiological, indicating an average functional decline with age. However it can help in sorting out dysfunctional subjects for further selective medical attention.
It is perhaps worth underlining the significantly higher rate of Open Eyes defective subjects, which might well indicate a higher prevalence of visual impairments.
About sway density: This concept seems worth further consideration.
• The Mean Stay Time seems to express the presence of destabilizing stimuli;
• The Mean Spatial Distance between Stabilization Points seems to indicate the effectiveness of the control strategy to control balance.
• The Mean Time Distance between subsequent stabilization points shows a very limited variability: Its almost negligible oscillation (Std.Dev 0.04 sec) around its mean value (0.54 sec) in both Closed and Open Eyes tests could perhaps be interpreted as a Time-Constant in the ballistic impulsive motor control as suggested by Benjamini [43].
Conclusions
From the above evidence we can draw the following conclusions:
(1) The Score of Postural Functionality is a robust diagnostic tool: the higher its value, the higher the dysfunction level;
(2) A difference of SPF higher than 2 is to be considered strongly significant.
(3) The experimental application of SPF classification on a population that, although affected by different dysfunctions, is “compensated” and thus capable of “autonomous” life insofar as it is capable of performing daily life tasks, confirms the reliability of this Score;
(4) The strong correlation between the SPF score and all the balance parameters actually suggests its possible use as a dependable overall indicator;
(5) As recently demonstrated [44], the SPF might be used also as a diagnostic indicator to support selective proprioceptive deficit treatment;
(6) A fresh approach to balance-keeping diagnostics can be proposed as follows:
a. Is either Closed Eyes and/or Open Eyes SPF higher than 9? A positive answer indicates the likelihood of some deficit;
b. Is the SPF higher in the Closed Eyes test than in the Open Eyes one? A positive answer, together with a Romberg Quotient higher than normal, points to a proprioceptive deficit;
c. Further morphological analysis of the COP path parameters can then provide more specific diagnostics
It may be further remarked that some quasi-invariant parameters in the control of upright unperturbed stance (such as the Mean Time Distance, the Sway Area to Sway Path Ratio, the Confidence Ellipse Diameters Ratio) seem to be present, in some way confirming the nonlinear behaviour of the control itself. Further studies along these lines might cast additional light on the complex process of balance keeping.
Acknowledgements
(1) The Score of Postural Functionality was originally proposed by Prof. P.G. Morasso, Dr. L.Baratto and Dr M.Jacono, all of whom deserve full credit for the intuition of the SPF concept and the development of the specific algorithm.
(2) The authors gratefully acknowledge the assistance of Prof. Carlo Chiorri (University of Genoa, Italy, and VIE - Valorizzazione Innovazione Empowerment srl, Genova, Italy, http://www.vie-srl.com/) for reviewing the statistical analyses.
(3) The population data were collected by the Trainers of the Ben-Essere Non-Professional Sport Association which is performing a program of Adapted Physical Activity in support of the senior citizens of the ASL4 Chiavarese territory. To them go our thanks for their valuable contribution to our research and for their commitment to reducing frailty in the senior population through the adoption of a healthier lifestyle.
Funding and Conflicting Interests
The research was carried out without any specific funding through the analysis of collected data as part of routine functional assessment.
All the authors declare the absence of any commercial or conflicting interests.
References
- http://www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html
- http://fallsprevention.eu/
- Rubenstein LZ (2006) Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing 35: ii37-ii41.
- Shumway-Cook A, Baldwin M, Polissar NL, Gruber W (1997) Predicting the probability for falls in community-dwelling older adults. PhysTher 77: 812-819.
- Shumway-Cook A, Brauer S, Woollacott M (2000) Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. PhysTher 80: 896-903.
- Horak FB (1987) Clinical measurement of postural control in adults. PhysTher 67: 1881-1885.
- Berg KO, Wood-Dauphinee SL, Williams JI, Maki B (1992) Measuring balance in the elderly: validation of an instrument. Can J Public Health 83 Suppl 2: S7-S11.
- Tinetti ME (2003) Clinical practice. Preventing falls in elderly persons. N Engl J Med 348: 42-49.
- Raîche M, Hébert R, Prince F, Corriveau H (2000) Screening older adults at risk of falling with the Tinetti balance scale. Lancet 356: 1001-1002.
- Lanska DJ, Goetz CG (2000) Romberg's sign: development, adoption, and adaptation in the 19th century. Neurology 55: 1201-1206.
- Njiokiktjien C, de Rijke W (1972) The recording of Romberg' test and its application in neurology. Agressologie 13: 1-7.
- Norré ME (1993) Sensory interaction testing in platform posturography. J LaryngolOtol 107: 496-501.
- Kapteyn TS, Bles W, Njiokiktjien CJ, Kodde L, Massen CH, et al. (1983) Standardization in platform stabilometry being a part of posturography. Agressologie 24: 321-326.
- Demura S, Kitabayashi T, Noda M (2008) Power spectrum characteristics of sway position and velocity of the center of pressure during static upright posture for healthy people. Percept Mot Skills 106:307-316.
- Baratto L, Morasso PG, Re C, Spada G (2002)A new look at posturographic analysis in the clinical context: sway-density versus other parameterization techniques. Motor Control6:246-270
- Blaszczyk JW, Klonowski W (2001) Postural stability and fractal dynamics. ActaNeurobiolExp (Wars) 61: 105-112.
- Chiari L, Cappello A, Lenzi D, Della Croce U (2000) An improved technique for the extraction of stochastic parameters from stabilograms. Gait Posture 12: 225-234.
- Collins JJ, De Luca CJ (1993) Open-loop and closed-loop control of posture: a random-walk analysis of center-of-pressure trajectories. Exp Brain Res95:308-318.
- Rocchi L, Chiari L, Cappello A (2004) Feature selection of stabilometric parameters based on principal component analysis. Med BiolEngComput42:71-79.
- Isableu B, Ohlmann T, Crémieux J, Amblard B (2003) Differential approach to strategies of segmental stabilisation in postural control. Exp Brain Res 150:208-221.
- Chiari L, Rocchi L, CappelloA (2002)Stabilometric parameters are affected by anthropometry and foot placement. ClinBiomech 17:666-677.
- Baczkowicz D, Szczegielniak J, Proszkowiec M (2008) Relations between postural stability, gait and falls in elderly persons--preliminary report. OrtopTraumatolRehabil10:478-485.
- Houdijk H, Fickert R, van Velzen J, van Bennekom C (2009)The energy cost for balance control during upright standing. Gait Posture30:150-154.
- Strachan D, Rose G (1991) Strategies of prevention revisited: effects of imprecise measurement of risk factors on the evaluation of "high-risk" and "population-based" approaches to prevention of cardiovascular disease. J ClinEpidemiol44:1187-1196.
- Piastra G, Ferrari Bravo M,Lucarini S,Cavagnaro P (2012)Back pain and Adapted Physical Activity: results from the experience in ASL 4 Chiavarese of Liguria. G Gerontol 60:106-112.
- Metz CE (1978) Basic principles of ROC analysis. SeminNucl Med8:283-298.
- Zweig MH, Campbell G (1993) Receiver-operating characteristic (ROC) plots: a fundamental evaluation tool in clinical medicine. ClinChem39:561-577.
- Zou KH, O'Malley AJ, Mauri L (2007) Receiver-operating characteristic analysis for evaluating diagnostic tests and predictive models. Circulation115:654-657.
- Lasko TA, Bhagwat JG, Zou KH, Ohno-Machado L (2005)The use of receiver operating characteristic curves in biomedical informatics. J Biomed Inform38:404-415.
- Jacono M, Casadio M, Morasso PG, Sanguineti V (2004) The sway-density curve and the underlying postural stabilization process. Motor Control 8: 292-311.
- Huang HC, Gau ML, Lin WC, George K (2003) Assessing risk of falling in older adults. Public Health Nurs 20: 399-411.
- Laessoe U, Hoeck HC, Simonsen O, Sinkjaer T, Voigt M (2007) Fall risk in an active elderly population--can it be assessed? J Negat Results Biomed 6: 2.
- Ghafouri M, Thullier F, Gurfinkel VS, Lestienne FG (1998) Muscular after-contraction and ongoing postural reactions in standing and sitting humans. NeurosciLett 250: 61-65.
- Gatev P, Thomas S, Kepple T, Hallett M (1999) Feedforward ankle strategy of balance during quiet stance in adults. J Physiol514 : 915-928.
- Winter DA, Patla AE, Rietdyk S, Ishac MG (2001) Ankle muscle stiffness in the control of balance during quiet standing. J Neurophysiol 85: 2630-2633.
- Loram ID, Lakie M (2002) Human balancing of an inverted pendulum: position control by small, ballistic-like, throw and catch movements. J Physiol 540: 1111-1124.
- Bottaro A, Casadio M, Morasso PG, Sanguineti V (2005) Body sway during quiet standing: is it the residual chattering of an intermittent stabilization process? Hum MovSci 24:588-615.
- Kiemel T, Oie KS, Jeka JJ (2006)Slow dynamics of postural Sway are in the feedback loop. J Neurophysiol 95:1410-1418.
- Shadmehr R (2000) Learning of action through adaptive combination of motor primitives. Nature 407:742-747.
- Tin C, Poon CS (2005)Internal models in sensorimotor integration: perspectives from adaptive control theory. J Neural Eng2:S147-S163.
- Gogola A, Saulicz E, Kuszewski M, Matyja M, Mysliwiec A (2014) Development of low postural tone compensatory patterns - predicted dysfunction patterns in lower part of the body. Dev Period Med18:386-393.
- Elias LA, Watanabe RN, Kohn AF (2014) Spinal mechanisms may provide a combination of intermittent and continuous control of human posture: predictions from a biologically based neuromusculoskeletalmodel. PLoSComputBiol 10:e1003944.
- Benjamini Y, Hochberg Y (2000) On the adaptive control of the false discovery rate in multiple testing with independent statistics. Journal of Educational and Behavioral Statistics 25: 60–83.
- Scoppa F, Gallamini M, Belloni G (2015) Treating Balance Disorders with Ulllt Acupuncture Stimulation: A Further Pilot Study on Normal Subjects Confirms Clinical Applicability of Treatment. J Nov Physiother 6: 285.
Relevant Topics
- Electrical stimulation
- High Intensity Exercise
- Muscle Movements
- Musculoskeletal Physical Therapy
- Musculoskeletal Physiotherapy
- Neurophysiotherapy
- Neuroplasticity
- Neuropsychiatric drugs
- Physical Activity
- Physical Fitness
- Physical Medicine
- Physical Therapy
- Precision Rehabilitation
- Scapular Mobilization
- Sleep Disorders
- Sports and Physical Activity
- Sports Physical Therapy
Recommended Journals
Article Tools
Article Usage
- Total views: 11752
- [From(publication date):
October-2016 - Aug 29, 2025] - Breakdown by view type
- HTML page views : 10778
- PDF downloads : 974