Intrahepatic Portosystemic Venous Shunt: A Case Report
Received: 02-Nov-2023 / Manuscript No. roa-23-118744 / Editor assigned: 06-Nov-2023 / PreQC No. roa-23-118744 / Reviewed: 20-Nov-2023 / QC No. roa-23-118744 / Revised: 24-Nov-2023 / Manuscript No. roa-23-118744 / Published Date: 30-Nov-2023
Abstract
The intrahepatic portosystemic venous shunt is defined as communication between an intrahepatic portal vein and a systemic vein, including the hepatic and perihepatic veins, via an anomalous intrahepatic venous channel. Intrahepatic shunts between portal and systemic veins can be acquired (cirrhosis, trauma, rupture of a portal vein aneurysm) or congenital. Intrahepatic portosystemic venous shunts (IPSVSs) are rare vascular malformations. They can be asymptomatic or present with various symptoms including encephalopathy. We present one case of IPSVS discovered incidentally.
Keywords
IPVS; MRI; Ultrasound; Asymptomatic
Introduction
The term IPSVS is used specifically to describe a lesion with abnormal communication(s) between the portal and hepatic veins, and four morphological types has been described [1]. The type 1 is the most common IPSVS involves a single large vessel of constant diameter connecting the right portal vein to the inferior vena cava (IVC). In type 2 IPSVS, one or multiple connections are present between peripheral branches of portal and hepatic veins in a single hepatic segment. If there is an aneurysmal connection between portal and hepatic veins is defined as a shunt and it is classified as type 3.Multiple communications between portal and hepatic veins involving both lobes of the liver is found in type 4 IPSVS.
These lesions are usually asymptomatic and are discovered incidentally when ultrasound (US), computed tomography (CT) scan, or magnetic resonance are performed for other reasons. Patients may be misdiagnosed with psychiatric or neurologic disorders if the IPSVS is not identified as a cause for encephalopathy [2].
In this manuscript, we describe one case of IPSVS involved a patient who was asymptomatic and in whom IPSVS was an incidental finding on an abdominal Ultrasound performed for other indications.
Observation
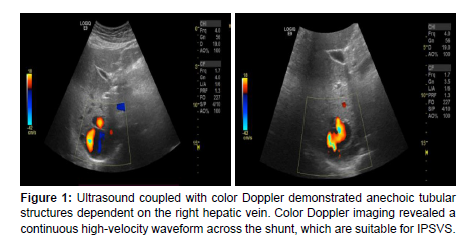
A 42-year-old patient, who presented for evaluation of bladder pain, she was referred by a general practitioner for suspicion of a hydatid cyst of the right liver. On ultrasound: Structure of a vascular nature of the right liver, probably at the expense of the right hepatic vein (Figure 1).
A follow-up CT scan showed no significant change in the IPSVS and hepatic mass (Figure 2a and 2b).
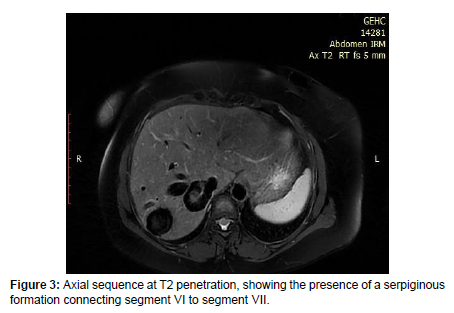
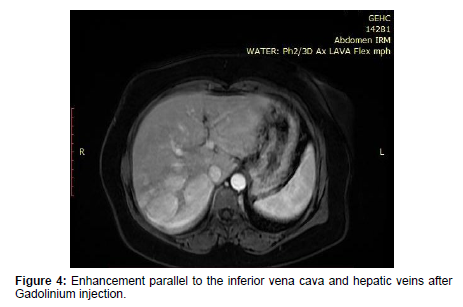
The patient underwent liver MRI to better characterize the abovementioned lesion, which showed an enlarged liver with a hepatic arrow measured at 17 cm with a homogeneous signal, with no sign of dysmorphism. It is the site of a thin-walled serpiginous formation straddling segments VI and VII in un signal T1 and T2 (Figure 3), without septum or endoluminal material or calcifications parietal. It communicates the right hepatic vein with the retro-hepatic part of the inferior vena cava (Figure 4).
Discussion
IPSVS are rare hepatic vascular malformations which are usually congenital, but they may also be acquired due to portal hypertension or iatrogenic causes. When diagnosed, periodic laboratory evaluations are important because of the ongoing potential risk of hepatic encephalopathy [3]. While most asymptomatic IPSVS are discovered incidentally as in our case, if suspected, color Doppler sonography, is highly sensitive and specific.
Our case is defined as a type 1 of IPSVS involves a single large vessel of constant diameter connecting the right portal vein to the inferior vena cava (IVC).
Multiple imaging modalities are useful for diagnosis of an intrahepatic portosystemic venous shunt including color Doppler ultrasonography, contrast-enhanced CT, MRI or conventional catheterdirected angiography. The imaging finding most consistent with diagnosis of a portosystemic venous shunt is visualization of a direct communication between portal and hepatic veins. Secondary findings on imaging suggestive of a shunt include abnormal blood pooling from a dilated portal branch with early visualization of the hepatic venous system [4].
The more difficult situation is that of the asymptomatic patient. Although transfemoral transcatheter embolization with coils or other mechanical occluders is a relatively safe procedure, complications do occur including infection, hemorrhage, portal vein occlusion, and portal hypertension, among others [5].
The analysis Risk/benefit is difficult, due to the unknown natural history of an IPSVS that has remained asymptomatic into adulthood. Several reports have shown that IPSVS can be a cause of hepatic encephalopathy and the incidence of hepatic encephalopathy has been found to increase with age [2,6].
The entity of IPSVS and their endovascular treatment have been described previously. The approach to the asymptomatic patient and the question of whether a prophylactic procedure should be offered has never been discussed in the literature.
Conclusion
IPSVS are rare hepatic vascular malformations. Although usually asymptomatic and discovered incidentally on imaging, we described one case an asymptomatic 42-year-old, whose shunt was incidentally discovered. There is no consensus on how to approach asymptomatic patients with IPSVS. We believe that treatment of asymptomatic IPSVS, if straightforward, should be offered to otherwise healthy patients, regardless of age, as an alternative to clinical and Doppler ultrasound surveillance.
References
- Park JH, Cha SH, Han JK, Han MC (1990) Intrahepatic portosystemic venous shunt. AJR Am J Roentgenol 155: 527-528.
- Mori H, Hayashi K, Fukuda T (1987) Intrahepatic portosystemic venous shunt: occurrence in patients with and without liver cirrhosis. AJR Am J Roentgenol 149: 711-714.
- Senocak E, Oğuz B, Edgüer T, Cila A (2008) Congenital intrahepatic portosystemic shunt with variant inferior right hepatic vein. Diagn Interv Radiol 14: 97-99.
- Pocha C, Maliakkal B (2004) Spontaneous intrahepatic portal‐systemic venous shunt in the adult: case report and review of the literature. Dig Dis Sci 49: 1201‐1206.
- Angle JF, Siddiqi NH, Wallace MJ (2010) Quality improvement guidelines for percutaneous transcatheter embolization: Society of Interventional Radiology Standards of Practice Committee. J Vasc Interv Radiol 21: 1479-1486.
- Lee YJ, Shin BS, Lee IH (2012) Intrahepatic portosystemic venous shunt: successful embolization using the Amplatzer Vascular Plug II. Korean J Radiol 13: 827-831.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Jaddour M, Imrani K, Moatassimbillah N, Nasser I (2023) IntrahepaticPortosystemic Venous Shunt: A Case Report. OMICS J Radiol 12: 505.
Copyright: © 2023 Jaddour M, et al. This is an open-access article distributedunder the terms of the Creative Commons Attribution License, which permitsunrestricted use, distribution, and reproduction in any medium, provided theoriginal author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Usage
- Total views: 1428
- [From(publication date): 0-2023 - Dec 10, 2025]
- Breakdown by view type
- HTML page views: 1100
- PDF downloads: 328