Research Article Open Access
Killer Cell Immunoglobulin like Receptors (KIR) Gene Variations in Rheumatic Fever and Rheumatic Heart Disease Patients from North India
Sarkar S#1, Rastogi M#1, Kumar R2 and Chakraborti AN*1
1Department of Experimental Medicine and Biotechnology, Post Graduate Institute of Medical Education and Research, Chandigarh, India
2School of Public Health, Post Graduate Institute of Medical Education and Research, Chandigarh, India
#Both the authors contributed equally to this study
- *Corresponding Author:
- Chakraborti A
Department of Experimental Medicine and Biotechnology
Post Graduate Institute of Medical Education and Research
Chandigarh- 160012
India
Tel: +91 172 2746277
Fax: +91 172 2744401
E-mail: superoxide14@gmail.com
Received date: January 11, 2016; Accepted date: June 22, 2016; Published date: June 30, 2016
Citation: Sarkar S, Rastogi M, Kumar R, Chakraborti A (2016) Killer Cell Immunoglobulin like Receptors (KIR) Gene Variations in Rheumatic Fever and Rheumatic Heart Disease Patients from North India. J Clin Infect Dis Pract 1:105. doi: 10.4172/2476-213X.1000105
Copyright: © 2016 Sarkar S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Clinical Infectious Diseases & Practice
Abstract
The autoimmune sequelae of rheumatic fever (RF) and rheumatic heart disease (RHD) are due to untreated or partially treated pharyngitis caused by Group A streptococcus (GAS). RF/RHD usually affects the genetically susceptible individuals. KIR (Killer cell immunoglobulin like receptor) of NK (natural killer) cell has been documented in susceptibility to various autoimmune diseases. KIR is of activating, inhibitory, pseudo and framework types. In here, 29 patients (pharyngitis, RF and RHD) and controls were studied to establish the association of different KIR genes in development of RF/RHD. KIR genotyping in all the disease groups revealed that the frequency of activating KIR2DS4A and inhibitory KIR2DL5B were less in RHD compared to the control. On the other hand, frequency of activating KIR2DS5A was more in RHD than pharyngitis. A significant difference in the frequency of KIR2DS2A and KIR3DL1B were found in pharyngitis compared to control. Interestingly, the overall data revealed a marked decrease of activating genes in pharyngitis and an increase in RHD. However, in the study, the framework genes were comparatively conserved and pseudo genes did not show any significant change. Thus, the study suggests an association of KIR in the pathogenesis of RF/RHD by demonstrating the variations in specific genotypes. This can be correlated to the prolonged activation of NK cells which may be accountable for regulation of adaptive immune response and self-tolerance. Further study in large cohort may unveil more information regarding the role of KIR in the development of the disease.
Keywords
KIR; Natural killer cells; Group A streptococcus ; Rheumatic fever; Rheumatic heart disease; Activating gene; Inhibitory gene
Introduction
Rheumatic fever (RF) and rheumatic heart disease (RHD) are the post infection autoimmune disease sequelae of pharyngitis caused by Group A streptococcus (GAS) or Streptococcus pyogenes [1]. The annual incidence of GAS infection reaches to 700 million worldwide. A total of 470000 RF cases are diagnosed with 233000 reported deaths due to complications of RHD [2]. The underlying mechanism of the development of RF/RHD is poorly understood. However, the proposed hypothesis in the development of RF/RHD is the autoimmune reaction due to molecular mimicry between different GAS and host proteins [3]. Host adaptive and innate immune systems actively participate in the regulation of autoimmune diseases and adjunct the progression of RF/RHD pathogenesis.
An important component of the innate immune system is NK (Natural killer) cells comprising 10-15% of total peripheral blood lymphocytes. NK cells are instrumental in playing a decisive role in immune activation and regulation [4]. Upon activation, NK cells trigger subsets of T-cells followed by releasing cytokines and chemokines for the clearance of pathogens. During the initial stages of infection, NK cells secrete interferon-γ (IFN-γ), which triggers expression of MHC class I and class II on antigen presenting cells and initiates differentiation of CD4+ T cells to Th1 cells [5,6]. They sequentially produce IL-2 and IFN-γ, which induce the synthesis cytokines and promote the proliferation of NK cells [7]. NK cells expresses KIR (killer cell immunoglobulin like receptor) on their surface and are divided into activating, inhibitory, pseudo and framework genes. KIR molecules target class-I human leukocyte antigen (HLAs) during the time of NK cell inhibition. Continuous expression of inhibitory and activating genes interacts with HLA class- II molecule and subsequently generates signals to eliminate the cells lacking ligands for the KIR inhibitory receptor [8]. HLA class-II molecules, which have been found to be associated with RHD, are targeted by the KIR and subsequently regulate the function of NK cells [8,9].
The regulation of NK cells and its function depends on the balance between activating and inhibitory genes, which further help NK cells to initiate the effector functions like cytolytic activity [10]. The activation of NK cells may be explained by “missing self ” and “induced self ” hypothesis. Normally, cells expressing adequate MHC class-I proteins are not targeted by the NK cells. But, as per the “missing self ” hypothesis, cells lacking MHC class-I proteins (either due to viral infection or cancer) are readily targeted and killed by the NK cells [11-13]. According to “induced self ” hypothesis, stress condition created by malignant or virus infected cells produce signal like MICA/ MICB and serve as ligand for the activating receptor NKG2D (natural killer group 2, member D) present on the surface of NK cells [14]. Unlike activating KIR receptors, which selectively interact with major histocompatibility complex (MHC) class I ligands, the inhibitory receptors of NK cells specifically target MHC class I ligands [15].
Rajagopalan et al. have demonstrated that peptides having low affinity to MHC class I show an antagonistic effect to the peptides having high affinity. Additionally, this antagonism is irrespective of KIR genotyping and frequency of activating or inhibitory receptors [16]. Framework genes are the haplotypes, which shows a conserved region in KIR genomic pattern [17]. The framework KIR receptors are thought to be consisted of haplotype A and B. Haplotype A KIR genes are considerably frequent in the Caucasian population, whereas, the haplotype B KIR genes comprises genotypes carrying more activating genes [18-21]. In contrast, pseudo KIR genes like 2DP1 cannot encode receptors due to the presence of aberrant reading frames [22]. KIR with different activating and inhibitory genes has been reported to be significantly associated with leukemia [23], autoimmune disease like type-I diabetes mellitus [24], uveitis [25], rheumatic diseases like systemic sclerosis [26], systemic lupus erythematosus [27,28], ankylosing spondylitis [29], rheumatoid arthritis [30] and autoimmune hepatitis [31]. In the present study, an attempt has been made to correlate the association of different KIR receptors with the progression of the RF/RHD pathogenesis.
Materials and Methods
Sample collection
Clinically diagnosed 5 to 15 year old pharyngitis and 5 to 65 year old RF/RHD patients (n=30), who visited the Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh, India, were included in the study. Blood samples from each disease group (pharyngitis, RF and RHD) as well as healthy individuals were collected after their written informed consents. All the RF/RHD patients were on prophylactic penicillin during the time of blood collection while, no penicillin prophylaxis were given to the patients of pharyngitis prior to the blood collection.
DNA isolation
Genomic DNA was isolated from whole blood by HiYieldTM Genomic DNA mini kit in accordance with the manufacturer’s instructions (Real Biotech Corporation, Taiwan).
KIR genotyping
KIR is located on human chromosome 19q13.4 of the leukocyte receptor complex (LRC) and consists of 15 genes [32,33]. These genes can be classified into inhibitory genes (2DL1, 2DL2, 2DL3, 2DL5), activating (2DS1, 2DS2, 2DS3, 2DS4, 2DS5, 3DL1, 3DS1), pseudo (2DP1 ), and framework genes (2DL4, 3DL2, 3DL3 ). 29 pairs of primers were used to amplify all the KIR genes. DRB1 was used as an internal control. PCR (polymerase chain reaction) primers and reaction conditions were followed as described previously [32].
Statistical analysis
Data were analyzed by Pearson’s Chi-Square test and Fisher's exact test using SPSS software (Statistical Package for the Social Sciences), version 16, p< 0.05 was considered as significant. On the basis of each KIR gene, the odds ratios between different KIR genes and groups were calculated for disease and control groups.
Results
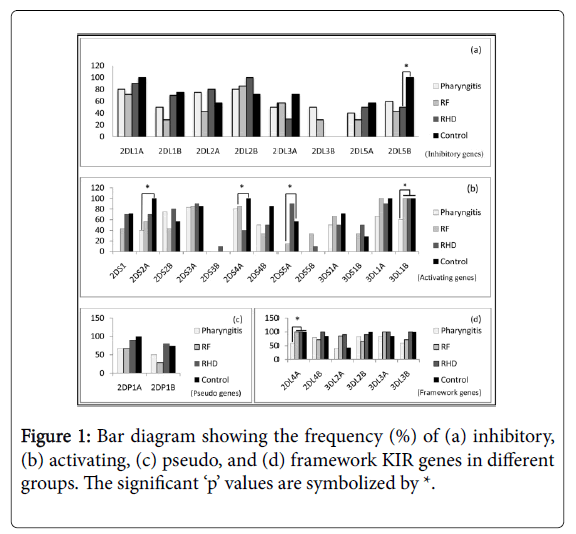
To assess the role of KIR in RF/RHD pathogenesis, three disease groups- pharyngitis, RF and RHD were included in the study. KIR genotyping was done in all the disease groups and correlated with age and sex matched control. Different frequencies in terms of presence of specific KIR genes were observed in the study group (Table 1). Genotyping data when expressed statistically using linear-by-linear distribution, elicited that the frequency of activating KIR2DS4A (p=0.035) and inhibitory KIR2DL5B (p=0.044) were less in RHD compared to the control. 2DS5A , another activating KIR was found to be more frequent (p=0.014) in RHD than pharyngitis. Besides, activating KIR2DS2A (p=0.045) was in increased frequency in pharyngitis compared to control. Activating gene KIR3DL1B , and a framework gene KIR2DL4A were found to be significantly less frequent (p=0.034) in pharyngitis than the other groups. However, we did not find any significant association of pseudo genes in different groups. The framework genes were found to be conserved in all the study groups (Figure 1). The statistical odds revealed the possibility to develop each disease stage on the basis of a specific type of KIR genotype. Higher odd values of 3DL2A (12.000 and 8.000 respectively in RHD and RF), 2DS5A (6.750 in RHD) were observed compared to control (Table 2).
| Serial Number | KIR gene types | KIR genes | Disease Groups (%) | Control (%) | p-values between each groups | ||
|---|---|---|---|---|---|---|---|
| Pharyngitis | RF | RHD | Healthy | ||||
| -1 | -2 | -3 | -4 | ||||
| 1 | 2DL1A | 80 | 71.4 | 90 | 100 | NS | |
| 2 | 2DL1B | 50 | 28.6 | 70 | 75 | NS | |
| 3 | 2DL2A | 75 | 42.9 | 80 | 57.1 | NS | |
| 4 | Inhibitory | 2DL2B | 80 | 85.7 | 100 | 71.4 | NS |
| 5 | 2DL3A | 50 | 57.1 | 30 | 71.4 | NS | |
| 6 | 2DL3B | 50 | 28.6 | 0 | 0 | NS | |
| 7 | 2DL5A | 40 | 28.6 | 50 | 57.1 | NS | |
| 8 | 2DL5B | 60 | 42.9 | 50 | 100 | 0.044* (between groups 3 and 4) | |
| 9 | 2DS1 | 0 | 42.9 | 70 | 71.4 | NS | |
| 11 | 2DS2A | 40 | 57.1 | 70 | 100 | 0.045* (between groups 1 and 4) | |
| 12 | 2DS2B | 75 | 42.9 | 80 | 57.1 | NS | |
| 13 | 2DS3A | 83.3 | 85.7 | 90 | 85.7 | NS | |
| 14 | Activating | 2DS3B | 0 | 0 | 10 | 0 | NS |
| 15 | 2DS4A | 80 | 85.7 | 40 | 100 | 0.035*(between groups 3 and 4) | |
| 16 | 2DS4B | 50 | 33.3 | 50 | 85.7 | NS | |
| 17 | 2DS5A | 0 | 14.3 | 90 | 57.1 | 0.014* (between groups 2 and 4) | |
| 18 | 2DS5B | 0 | 33.3 | 10 | 0 | NS | |
| 19 | 3DS1A | 50 | 66.7 | 50 | 71.4 | NS | |
| 20 | 3DS1B | 0 | 33.3 | 50 | 28.6 | NS | |
| 21 | 3DL1A | 66.7 | 100 | 90 | 100 | NS | |
| 22 | 3DL1B | 60 | 100 | 100 | 100 | 0.034*(between groups 1 and other groups) | |
| 23 | Pseudo | 2DP1A | 66.7 | 66.7 | 90 | 100 | NS |
| 24 | 2DP1B | 50 | 28.6 | 80 | 75 | NS | |
| 25 | Framework | 2DL4A | 60 | 100 | 100 | 100 | 0.034* (between group 1 and other groups) |
| 26 | 2DL4B | 80 | 71.4 | 100 | 85.7 | NS | |
| 27 | 3DL2A | 40 | 85.7 | 90 | 42.9 | NS | |
| 28 | 3DL2B | 83.3 | 66.7 | 90 | 100 | NS | |
| 29 | 3DL3A | 83.3 | 100 | 100 | 85.7 | NS | |
| 30 | 3DL3B | 60 | 71.4 | 100 | 100 | NS | |
Table 1: Frequencies of KIR genes among the study groups.
The overall findings also revealed that few KIR genes possessed 100% expression in the disease groups. RHD group possessed 100% frequency of inhibitory KIR2DL2B , activating KIR3DL1B and framework KIR2DL4A , KIR2DL4B , KIR3DL3A , KIR3DL3B genes. Similarly, RF patients exhibited 100% frequency of activating KIR3DL1A , KIR3DL1B and framework 2DL4A , KIR3DL3A . On the other hand, several genes were not detectable in the disease groups. We observed that various activating KIR genes (2DS1 , 2DS3B , 2DS5A , 2DS5B and 3DS1B ) were absent in pharyngitis group. Besides, RHD group also showed absence of inhibitory KIR2DL3B and activating KIR2DS3B , KIR2DS5B. Activating KIR2DS3B was present only in RHD groups (10%) (Table 1 and Figure 1).
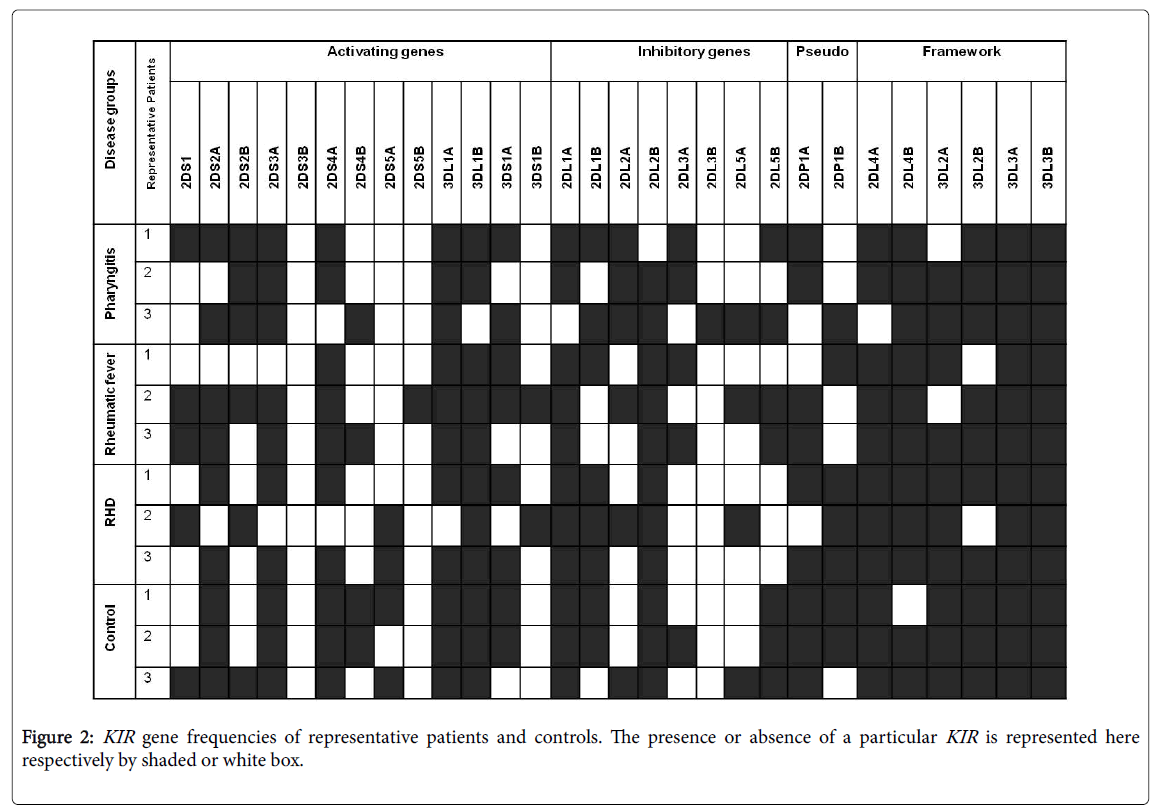
The overall data revealed a marked decrease of activating genes in pharyngitis and an increase in RHD group (Table 2 and Figure 2). Interestingly, we also observed that frequency of pseudo genes were low in pharyngitis and RF when compared to RHD and control.
| KIR genes | Odd ratios in the disease groups against control? | |||
|---|---|---|---|---|
| Pharyngitis | RF | RHD | ||
| Inhibitory gene | 2DL2A | 2.25 | - | 3 |
| 2DL2B | 1.6 | 2.4 | - | |
| Activating gene | 2DS2B | 2.25 | - | 3 |
| 2DS3A | - | 1 | 1.5 | |
| 2DS5A | - | - | 6.75 | |
| 3DS1B | - | 1.25 | 2.5 | |
| Pseudo gene | 2DP1B | - | - | 1.333 |
| Framework gene | 3DL2A | - | 8 | 12 |
Table 2: Odd values of selected KIR genes among the different disease groups.
Discussion
NK cell, an important arm of innate immunity, acts as a bridge between the host innate and adaptive immune response during infection [34]. Regulation of NK cell function tremendously alters the host adaptive immune response in different autoimmune disorders [23-31]. The putative functions of NK cell can be explained by the complex and discrete associations of their receptor molecules. NK cell expresses KIR on their surface, which plays a detrimental role in the trafficking of adaptive immune response by targeting different class of HLA ligands [8]. The extensive diversity of KIR genes among the different population as well as in the diseases has already been reported [34]. KIR gene variation is also observed in autoimmune diseases [23-31]. But, there are no such studies, which show the association of KIR genes in the RF/RHD pathogenesis. Hence, in the present study, we have reported the variation of different KIR genes in the early and late onset of the disease i.e. from pharyngitis to RF/RHD.
A wide diversity in KIR gene distribution was observed among the disease groups (Figure 1). Activating and inhibitory genes of KIR have the potential to differentially regulate the function of NK cells [10]. Short cytoplasmic domain of the activating KIR contains basic acids,which interact with the acidic or negatively charged amino acids of DAP12 (12KDa) and provides signals to ITAM (immunoreceptor tyrosine based activation motif) to produce kinase enzymes. These enzymes activate the NK cells, which are cytotoxic to the target cells and release numerous proinflammatory and regulatory cytokines [IFN-γ, TNF-α, IL-1, IL-5, IL-10, IL-12 IL-13, IL-15, IL-18, granulocyte macrophage colony stimulating factor (GM-CSF)] and chemokines [macrophage inflammatory proteins (MIP-1α, MIP-1β), IL-8, and RANTES] [35]. Besides, the elevated level of cytokines like TNF-α, IFN-γ, IL-10, IL-6, IL-4 in RF/RHD is already reported [36,37].
One of the important mechanisms behind such elevation of cytokine secretion in RHD may be the activation of NK cells through activating KIR . In contrast, our study also reveals an overall increase in the frequency of activating KIR genes (2DS1 , 2DS2 , 2DS3 , 3DS1B and 2DS5A ) in RHD group compared to RF and pharyngitis (Table 2, Figure 1). We have observed a significant association of 2DS4A in RF and 2DS5A in RHD. It suggests that the prolonged activation of NK cells persists throughout the developmental stage of RHD (Table 1). Apart from these, the lower frequency of activating KIR3DL1B in pharyngitis suggests the poor involvement of NK cell in the initial stage of GAS infection. Our data is in the agreement with the study conducted by Rosaschino et al., where they have also found a significant diminution of NK cells number in school going children having pharyngistis [38]. However, a non-significant increase of activating KIR2DS5B has also been noticed.
The high odds ratios (more than 1.000) are indicative of the possibility to develop a particular stage of disease (i.e. pharyngitis or RF or RHD) on the basis of KIR genes distribution. In here, we have observed high odd ratios of activating KIR genes (2DS2B, 2DS3A, 2DS5A and 3DS1B ) in RHD group compared to RF and pharyngitis (Table 2).
This data suggests the utmost activation of NK cells, which further results in the generation of cytotoxicity during the late stage of the disease. Moreover, it has been postulated that T cells with IL-2 secretion leads to the increased NK cell cytotoxicity, which ultimately causes the alteration in the heart valve due to fibrosis and hemodynamic changes [39].
Inhibitory KIR contains ITIM or immunoreceptor tyrosine based inhibitory motif. Tyrosine residues of ITIM are phosphorylated by kinases followed by dephosphorylation by SHP-1 (phosphatase like enzyme), which results in the inhibition of NK cell functions [40]. It has been shown that HLA class I acts as a ligand for the binding of different inhibitory KIR receptors. Inhibitory KIR genes target class-I HLA (i.e. HLA-A, HLA-B and HLA-C). Unlike HLA class-I, HLA class II is targeted by both activating and inhibitory KIR and induce signals for the elimination of target cell lacking ligands for inhibitory receptors [8]. Therefore, the interaction between receptor and ligands maintains the balance between different KIR and HLAs. In this study, we have observed a significant decrease in the frequency of inhibitory KIR2DL5B in all the disease groups compared to control. This data suggests that the NK cell inhibition is diminished due to the poor expression of its inhibitory receptor during the diseased condition. However, a non-significant increase in the frequency of inhibitory KIR2DL2A and 2DL2B has been observed in RHD.
Our study, for the first time, unveils the wide diversity in KIR genotype associated with the pathogenesis of RF/RHD in north Indian population. It is evidenced from the study that a genetic balance between activating and inhibitory receptors of KIR is associated with the autoimmune regulation of RF/RHD, which may be due to the increased frequency of activating KIR genes or decreased frequency of inhibiting KIR genes or both. Moreover, activation of NK cells may induce self-tolerance and subsequently initiate the valvular vandalism in RHD pathogenesis.
References
- Cunningham MW (2000) Pathogenesis of group A streptococcal infections. ClinMicrobiol Rev 13: 470-511.
- Carapetis JR, Steer AC, Mulholland EK, Weber M (2005) The global burden of group A streptococcal diseases. Lancet Infect Dis 5: 685-694.
- Dinkla K, Talay SR, Mörgelin M, Graham RM, Rohde M, et al. (2009) Crucial role of the CB3-region of collagen IV in PARF-induced acute rheumatic fever. PLoS One 4: e4666.
- Cooper MA, Fehniger TA, Caligiuri MA (2001) The biology of human natural killer-cell subsets. Trends Immunol 22: 633-640.
- Mandelboim O, Davis DM, Reyburn HT, Valés-Gómez M, Sheu EG, et al. (1996) Enhancement of class II-restricted T cell responses by costimulatory NK receptors for class I MHC proteins. Science 274: 2097-2100.
- Bihl F, Pecheur J, Bréart B, Poupon G, Cazareth J, et al. (2010) Primed antigen-specific CD4+ T cells are required for NK cell activation in vivo upon Leishmania major infection. J Immunol 185: 2174-2181.
- Artola RT, Mihos CG, Santana O (2011) The immunology of mitral valve stenosis. Int J Interferon Cytokine Mediator Res 3: 1-8.
- Srivastava RM, Savithri B, Khar A (2003) Activating and inhibitory receptors and their role in natural killer cell function. Indian J BiochemBiophys 40: 291-299.
- Toor D, Leal K, Kumar R, Sharma YP, Chakraborti A (2012) Association of HLA-DRB1*14 with rheumatic heart disease patients from Chandigarh, North India. Biomarkers 17: 160-165.
- Raulet DH, Held W (1995) Natural killer cell receptors: the offs and ons of NK cell recognition. Cell 82: 697-700.
- Pegram HJ, Andrews DM, Smyth MJ, Darcy PK, Kershaw MH (2011) Activating and inhibitory receptors of natural killer cells. Immunol Cell Biol 89: 216-224.
- Ljunggren HG, Kärre K (1990) In search of the 'missing self': MHC molecules and NK cell recognition. Immunol Today 11: 237-244.
- Watzl C (2003) The NKG2D receptor and its ligands-recognition beyond the "missing self"? Microbes Infect 5: 31-37.
- Groh V, Rhinehart R, Randolph-Habecker J, Topp MS, Riddell SR, et al. (2001) Costimulation of CD8alphabeta T cells by NKG2D via engagement by MIC induced on virus-infected cells. Nat Immunol 2: 255-260.
- Taveirne S (2011) Inhibitory receptors specific for MHC class I educate murine NK cells but not CD8alphaalpha intestinal intraepithelial T lymphocytes. Blood 118: 339-347.
- Rajagopalan S, Long EO (2010) Antagonizing inhibition gets NK cells going. ProcNatlAcadSci U S A 107: 10333-10334.
- Hsu KC, Liu XR, Selvakumar A, Mickelson E, O'Reilly RJ, et al. (2002) Killer Ig-like receptor haplotype analysis by gene content: evidence for genomic diversity with a minimum of six basic framework haplotypes, each with multiple subsets. J Immunol 169: 5118-5129.
- Uhrberg M, Valiante NM, Shum BP, Shilling HG, Lienert-Weidenbach K, et al. (1997) Human diversity in killer cell inhibitory receptor genes. Immunity 7: 753-763.
- Valiante NM, Uhrberg M, Shilling HG, Lienert-Weidenbach K, Arnett KL, et al. (1997) Functionally and structurally distinct NK cell receptor repertoires in the peripheral blood of two human donors. Immunity 7: 739-751.
- Wilson MJ, Torkar M, Haude A, Milne S, Jones T, et al. (2000) Plasticity in the organization and sequences of human KIR/ILT gene families. ProcNatlAcadSci USA 97: 4778-4783.
- Martin AM, Freitas EM, Witt CS, Christiansen FT (2000) The genomic organization and evolution of the natural killer immunoglobulin-like receptor (KIR) gene cluster. Immunogenetics 51: 268-280.
- Gomez-Lozano N, Vilches C. (2002) Genotyping of human killer-cell immunoglobulin-like receptor genes by polymerase chain reaction with sequence-specific primers: An update. Tissue Antigens 59: 184-193.
- de Smith AJ, Walsh KM, Ladner MB, Zhang S, Xiao C, et al. (2014) The role of KIR genes and their cognate HLA class I ligands in childhood acute lymphoblastic leukemia. Blood 123: 2497-2503.
- Van der Slik AR, Koeleman BP, Verduijn W, Bruining GJ, Roep BO, et al. (2003) KIR in type 1 diabetes: Disparate distribution of activating and inhibitory natural killer cell receptors in patients versus HLA-matched control subjects. Diabetes 52: 2639-2642.
- Levinson RD (2011) Killer immunoglobulin-like receptor genes in uveitis. OculImmunolInflamm 19: 192-201.
- Salim PH, Jobim M, Jobim LF, Xavier RM (2011) Autoimmune rheumatic diseases and their association with killer immunoglobulin-like receptor genes. Rev Bras Reumatol 51: 351-356, 362-4.
- Kimoto Y, Horiuchi T, Tsukamoto H, Kiyohara C, Mitoma H, et al. (2010) Association of killer cell immunoglobulin-like receptor 2DL5 with systemic lupus erythematosus and accompanying infections. Rheumatology (Oxford) 49: 1346-1353.
- Hou Y, Zhang C, Xu D, Sun H (2015) Association of killer cell immunoglobulin-like receptor and human leucocyte antigen-Cw gene combinations with systemic lupus erythematosus. ClinExpImmunol 180: 250-254.
- Jiao YL, Ma CY, Wang LC, Cui B, Zhang J, et al. (2008) Polymorphisms of KIRs gene and HLA-C alleles in patients with ankylosing spondylitis: possible association with susceptibility to the disease. J ClinImmunol 28: 343-349.
- Majorczyk E, Pawlik A, Luszczek W, Nowak I, Wis niewski A, et al. (2007) Associations of killer cell immunoglobulin-like receptor genes with complications of rheumatoid arthritis. Genes Immun 8: 678-683.
- Littera R, Chessa L, Onali S, Figorilli F, Lai S, et al. (2016) Exploring the Role of Killer Cell Immunoglobulin-Like Receptors and Their HLA Class I Ligands in Autoimmune Hepatitis. PLoS One 11: e0146086.
- http://www.ncbi.nlm.nih.gov/books/NBK10135/pdf/Bookshelf_NBK10135.pdf
- Kulkarni S, Martin MP, Carrington M (2010) KIR genotyping by multiplex PCR-SSP. Methods MolBiol 612: 365-375.
- Middleton D, Gonzelez F (2010) The extensive polymorphism of KIR genes. Immunology 129: 8-19.
- Lanier LL (2009) DAP10- and DAP12-associated receptors in innate immunity. Immunol Rev 227: 150-160.
- Yegin O, Coskun M, ErtuÄŸ H (1997) Cytokines in acute rheumatic fever. Eur J Pediatr 156: 25-29.
- Guilherme L, Kohler KF, Kalil J (2012) Rheumatic heart disease: Genes, inflammation and autoimmunity. RheumatolCurr Res S4.
- Rosaschino F, Albertini A, Torre R, Noseda F (1989) Various immune functions (with particular attention to NK cells) in young people with frequent episodes of pharyngitis. Boll IstSieroter Milan 68:156-166.
- Suri RK, Manjari RS, Sharma M (1998) Role of lymphocyte subsets in pathogenesis of rheumatic heart disease. Asian CardiovascThorac Ann 6: 104-107.
- Long EO (2008) Negative signaling by inhibitory receptors: the NK cell paradigm. Immunol Rev 224: 70-84.
Relevant Topics
- Antibiotics and Resistance
- Antifungal
- Antiviral therapy
- Bacteremia
- Bacterial diseases
- Broad Spectrum of Antibiotics
- Clinical Infectious Diseases
- Diagnosis of Pathogenic microorganisms
- Emerging infections
- Natural Antibiotics
- Opportunistic Pathogens
- Parasitic Diseases
- Pertussis Vaccines
- Prevention of infection
- Septicemia
- Viral Infections
- Viremia
Recommended Journals
Article Tools
Article Usage
- Total views: 12454
- [From(publication date):
August-2016 - Aug 15, 2025] - Breakdown by view type
- HTML page views : 11458
- PDF downloads : 996