Research Article Open Access
Knowledge of Birth Preparedness and Complication Readiness and Associated Factors among Health Care Providers in Benin City, Edo State
Obi Andrew Ifeanyichukwu1* and Okojie Hilda Obehi1,21Department of Community Health, University of Benin, Benin
2Department of Community Health, University of Benin Teaching Hospital, Benin
- *Corresponding Author:
- Obi Andrew Ifeanyichukwu
Department of Community Health, University of Benin
Benin City, Edo State, Benin
Tel: 2348023447122
E-mail: andrew.obi@uniben.edu
Received Date: November 23, 2015; Accepted Date: September 26, 2016; Published Date: September 30, 2016
Citation: Ifeanyichukwu OA and Obehi OH (2016) Knowledge of Birth Preparedness and Complication Readiness and Associated Factors among Health Care Providers in Benin City, Edo State. J Preg Child Health 3: 278. doi:10.4172/2376-127X.1000278
Copyright: © 2016 Ifeanyichukwu OA, et al. This is an open-access article distributed under the terms of the Creativ Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Pregnancy and Child Health
Abstract
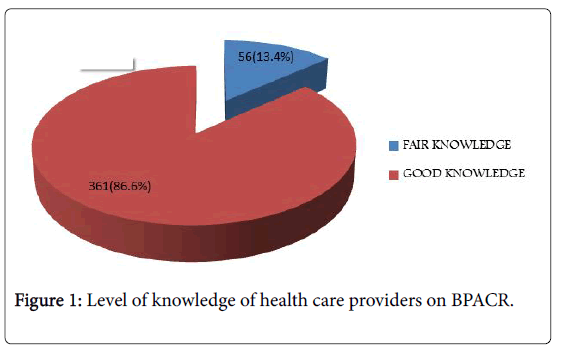
Nigeria accounts for 14% of global estimates of maternal mortalities. The role of health care providers remains indispensable to addressing obstetric emergencies by knowledgeable and appropriately skilled obstetric care services. This study was carried out to assess knowledge of birth preparedness and complication readiness (BPACR) and associated factors among health care providers (HCPs) in Benin City, with a view to improving HCPs knowledge for enhanced obstetric service delivery. Materials and Method: A community based analytical cross sectional study was conducted, involving researcher administration of pretested structured questionnaires to 417 consenting HCPs from selected health facilities in Benin City. Data collected was sorted for completeness, coded, entered and analysed using SPSS version 20.0 statistical software with statistical significance set at p˂0.050 and 95% confidence interval. Results: The mean age of respondents studied was 33.8 ± 8.0 (34.2± 6.9 years and 33.6 ± 8.3) years for male and female HCPs respectively. In relation to knowledge of BPACR, 361 (86.6%) HCPs had good knowledge while 56(13.4%) had fair knowledge. Awareness of BP (OR=2.328; 95%CI=1.176-4.609; p=0.015), training received on BP (OR= 0.207; 95%CI=0.077-0.558; p=0.002) and educational status (OR =0.342; 95%CI=0.143- 0.821; p=0.016) were significant predictors identified among HCPs as influencing knowledge on BPACR. Conclusion: Majority of HCPs studied had good knowledge of BPACR. There is need to sustain health care provider knowledge of this strategy through regular training and retraining programs on BPACR for improved maternal and child health service delivery.
Keywords
Benin City, Birth preparedness and complication readiness, Knowledge, Health care providers
Introduction
Globally, an estimated 358 000 maternal deaths occurred worldwide in 2008 with developing countries accounting for 99% (355, 000) of these deaths [1]. The situation is most dire for women in Sub-Saharan Africa, where 1 in every 16 women die of pregnancy related causes during her lifetime, compared with only 1 in 2,800 women in developed regions [2,3]. Nigeria contributes 14% of global estimates of maternal mortality; maternal mortality is an important indicator for reproductive health programs and services in any country [3].
Every pregnant woman faces the risk of sudden, unpredictable complications that could end in injury or death to mother and or to her child; these complications cannot be reliably predicted in 15% of pregnant women hence, it is necessary to employ strategies to overcome such problems as they arise. Lack of advance planning for use of skilled birth attendants for normal births and particularly inadequate preparation for rapid action in the event of obstetric complications/emergencies, are well documented factors contributing to delays in receiving skilled obstetric care [4].
The World Health Organization (WHO) estimates that three quarter of maternal fatalities and disabilities could be prevented if deliveries were to take place in well-equipped health facilities with suitably trained and skilled health care providers [5]. Since, 15% of pregnant women may develop obstetric complications, out of which 5% are likely to require some form of surgical/emergency intervention [6]. Hence, the need to employ cost effective intervention such as Birth Preparedness and Complication Readiness; this is a comprehensive strategy to help address delays in obtaining appropriate obstetric care and is aimed at promoting timely utilization of skilled maternal and neonatal health care; based on the theory that preparing for childbirth and being ready for complications reduces delays in obtaining care and thereby positively impacting on birth outcomes [5].
Studies have shown that despite knowledge of health intervention by HCPs the level of utilization of health services by clients remain low [3,6-8]. An Ethiopian Demographic and Health Survey [7] gave a 32.4% utilization of antenatal care (ANC) services with only 6% of all deliveries being attended to by skilled health providers. In Nigeria, Demographic and Health Survey [3] reports for 2013 reveals that although 61% of pregnant women received ANC from skilled health providers, only 36% of pregnant women delivered in health facilities while 38% of all deliveries reported were conducted by skilled health providers. Another study [8] in Rewa district of Madhya Pradesh,India to assess birth preparedness and complication readiness intervention revealed a gap between knowledge level and skills of health care providers. Less than 50% of HCPs studied had competent knowledge in relation to diagnosis and management of complication but could not implement it in real situation, this study further recommended need for repeated practical training of health care providers in standard procedures for diagnosing and management of emergencies that may occur [8].
In Nigeria, the 2013 Demographic and Health Survey [3] report showed that 39% of women do not receive antenatal care and that only 38% of births in Nigeria were conducted by skilled health care providers. Similarly, an assessment of health care providers in selected health facilities in Nigeria [6] in relation to supervision, maternal audits and use of standard protocol for maternal services revealed that although supervision takes place in about 70 % of health facilities studied, but with regard to use of standard protocol and facility based audit it was 40% and 21% respectively.
Furthermore, a study [9] in South West Nigeria to assess the level of health care providers’ knowledge in public Health facilities on the concept of emergency obstetric care and antenatal counselling services revealed that 91% of health care providers studied had poor knowledge of emergency obstetric care. Sixty three percent of respondents in this study [9] admitted that they counselled clients on the fact that all pregnancy may have risk of developing complications which they should be aware of and be prepared appropriately for. Despite claims by 75% of HCPs studied that they counselled pregnant women on danger signs of pregnancy and delivery with 40% of them also reported to have counselled their clients on complication readiness; the nonparticipant observational checklist findings however did not confirm most of the claims by the health care providers, as a lesser proportion of health care providers studied counselled their clients with the counselling session being more general than specific [9]. This study was therefore carried out to assess knowledge of birth preparedness and complication readiness (BPACR) and associated factors among health care providers in Benin City, with a view to improving health care provider knowledge for enhanced obstetric service delivery.
Materials and Method
This study was carried out in Benin City, the capital of Edo State, located in the South-South geopolitical zone of Nigeria. Benin City comprises three Local Government Areas:-Egor, Oredo and Ikpoba- Okha Local Government Areas respectively. Benin City is bounded to the west by Ovia North East Local Government Area and the North- East by Uhunmwuode Local Government Area and South by Ethiope– West Local Government Area of Delta State. It has an estimated population of 1086882 people consisting of 542545 and 544337 males and females respectively [10].
Benin is the predominant ethnic group; others include Esan, Etsako with other indigenous and non-indigenous tribes [11]. There is a high literacy rate [12] (75.6%) in the State, this is possibly due to the large distribution of public and private educational institutions. Benin City also has a local airport with a good network of roads although with variable level of motorability, especially during the rainy season when transportation can be very challenging [11]. Benin City also has a large distribution of public and private health institutions that offer a wide range of primary, secondary and tertiary health care services including maternal health services such as antenatal care, post natal care services, family planning etc. to its populace [13].
A community based analytical cross sectional study design was utilized for this study between February 2012 and June 2012. Researcher administered pretested structured questionnaires, adapted from the safe mother hood questionnaire [14] developed by maternal and neonatal health program of JHPIEGO was utilized for data collection in relation to socio-demographic characteristics and knowledge of birth preparedness and complication readiness among health care providers working in selected health facilities in Benin City. A minimum sample size of 403 health care providers was calculated using the Cochran formulae for simple proportion in a descriptive cross sectional study [15] based on 38% prevalence from a previous study on births attended by skilled birth attendants in Nigeria [3].
Furthermore, a multistage sampling technique was used to select HCPs for study as shown below;
STAGE 1: Selection of the 36 public and 78 private health facilities for study
From the list of operational health facilities in Benin City (i.e a total of 41 public and 122 private health facilities in Benin City as at time of study; 8 and 77; 17 and 24; 16 and 21 public and private health facilities for Egor LGA, Oredo LGA and Ikpoba – Okha LGA respectively). Based on sample size determination [15] from previous study [3] a representative sample of health facilities per LGA in the study area was obtained and selected by simple random sampling technique from the list of operational health facilities per LGA in Benin City as shown in Table A in appendix
Stage 2: Selection of health care providers from selected health facilities per LGA of study
The total population of HCPs involved in maternal care in all selected health facilities was obtained following a census of selected health facilities prior to the commencement of study proper (i.e 1096 health care providers). Sample proportionate to size of health care providers involved in maternal health care was calculated per selected health facility in relation to the calculated minimum sample size of health care providers (403 health providers) to be studied in Benin City. This is shown in Table B in appendix.
Stage 3: Based on the calculated health care providers sample size estimate per health facility, HCPs were subsequently selected by simple random sampling technique using a table of random numbers until the required number of health care providers to be selected per facility was reached
Knowledge on BPACR among HCPs was assessed based a points score system developed by researcher, this involved 80 question relating to knowledge on danger signs in pregnancy, labour, deliver, new born care and components of BPACR strategy. Every correct response was given a maximum point score of one and zero for all incorrect responses giving a maximum point score of 80, this scoring system had a reliability (Cronbach’s alpha) score of 0.758. Final categorization of level of knowledge on BPACR was based on percentage point score by respondents; having percentage score of = 49.9% was graded as poor knowledge, 50-69.9% fair knowledge and =70% good knowledge.
Data collected was sorted for completeness, coded, entered and analyzed using SPSS 20.0 statistical software with results presented as statements, frequency tables and figures. Bivariate analyses was conducted using Chi square and fishers’ exact test to identify independent variables that influenced knowledge of preparedness towards birth preparedness and complication readiness, subsequently logistic regression analysis was carried out to identify significant predictors and eliminate possible confounders. Statistical significance was set at p<0.050 and 95% confidence interval.
Ethical consideration
Ethical clearance was sought and obtained from the Ethics and Research Committee of the University of Benin Teaching Hospital, Benin City, Edo State before the commencement of the study. Institutional approval was also obtained from the Department of Hospital Services Edo State Ministry of Health, the three Local Government Areas respectively. Informed consent was sought and willfully obtained from the respondents before the commencement of the study, respondents were informed of the voluntary nature of participation in the study and that they could withdraw participation at any stage of the interview. There was no inducement (financial or otherwise) for respondents who agreed to participate in the study.
Limitation of study
Self-reporting may have introduced reporter bias as it may be difficult validating claims provided by respondents studied.
Results
The mean age of respondents studied was 33.8 ± 8.0 (34.2± 6.9 years and 33.6 ± 8.3) years for male and female HCPs respectively. Three hundred and thirty one (79.4%) of HCPs were female while 86(20.6%) were male. In relation to marital status, 243(58.9%) were married, 164(39.3%) single and 2(0.5%) divorced.
In relation to the educational status of HCPs, 374(89.7%) had completed tertiary education while 1(0.2%) had primary completed level of education. Nursing 290 (69.5%) was the predominant profession followed by Medicine 91(21.8%) and Community Health practice 36(8.6%); while in terms of designation of health care providers, 102 (24.5%) were Nurses/Midwives, 89 (21.3%) Doctors and 3 (0.7%) Community Health Officers. In relation to ethnic group of HCPs, 205 (49.2%) were Benin, 88 (21.1%) Esan, while 1(0.2%) was Igala.
In relation to awareness and training on birth preparedness and complication readiness, (Table 1) shows that 346(83.0%) of the HCPs were aware of the term BP; with School 294 (83.5%) and training 160 (46.2%) reported as their main source of information. In relation to training on BP 160 (38.4%) had received training with the mean frequency of training received being 0.7 ± 1.2; among which 121(75.6%) HCPs studied had received 1-2 training on BPACR.
| Variables | Frequency (n=417) | Percent |
|---|---|---|
| Age Group (Years) | ||
| 21-30 | 179 | 42.9 |
| 31-40 | 166 | 39.8 |
| 41-50 | 55 | 13.2 |
| 51-60 | 16 | 3.8 |
| =61 | 1 | 0.2 |
| Sex | ||
| Male | 86 | 20.6 |
| Female | 331 | 79.4 |
| Marital Status | ||
| Single | 164 | 39.3 |
| Married | 243 | 58.3 |
| Divorced | 2 | 0.5 |
| Separated | 4 | 1 |
| Widowed | 4 | 1 |
| Educational Status | ||
| 10 Completed | 1 | 0.2 |
| 20 Completed | 42 | 10.1 |
| 30 Completed | 374 | 89.7 |
| Category of HCP | ||
| Community Health Practice | 36 | 8.6 |
| Medicine | 91 | 21.8 |
| Nursing | 290 | 69.5 |
| Designation of HCP | ||
| Nurse/Midwife | 102 | 24.5 |
| Doctor | 89 | 21.3 |
| Community Health Officers | 3 | 0.7 |
Table 1: Socio-demographic Characteristics of Health Care Providers in Benin City, Edo State.
In relation to level of knowledge on BPACR (Figure 1)among HCPs, 361(86.6%) had good knowledge while 56(13.4%) of them had fair knowledge of BPACR. Furthermore, regarding factors associated with level of knowledge on BPACR among HCPs (Table 2), it was observed that the level of knowledge of BPACR increased significantly with rising level of education (p<0.01), a similar trend was observed in relation to designation of HCPs, and these differences was statistically significant (p<0.01).
| Variable | Frequency(n=417) | Percent |
|---|---|---|
| Awareness of birth preparedness | ||
| Yes | 346 | 83 |
| No | 71 | 17 |
| Source of information* (Multiple Response) n=346 | ||
| School | 294 | 83.5 |
| Training | 160 | 46.2 |
| Literature And Books | 148 | 42.8 |
| Superior at work | 53 | 15.3 |
| Training on BPACR | ||
| Yes | 160 | 38.4 |
| No | 257 | 61.6 |
| Frequency of Training(n=160) | ||
| 01Feb | 121 | 75.6 |
| 03Apr | 31 | 19.4 |
| >4 | 8 | 5 |
Table 2: Training and awareness of birth preparedness and complication readiness among health care providers from selected health facilities in Benin City, Edo State.
In addition, awareness of BP (p<0.01) and receiving training on BPACR (p<0.01) were significant factors associated with level of knowledge on BPACR. While increasing frequency of training received on BP (p=0.24), category of health facility were health care provider Further analysis, using multivariate logistic regression on predictors for knowledge of BPACR identified awareness of BP, educational status and training received on BPACR as significant predictors of knowledge on BPACR among HCPs; HCPs who were aware of BPACR were 2.3 worked (p=0.53), age grouping of health care provider in years (p=0.77) and marital status (p=0.19) were not significant factors associated with level of knowledge on BPACR.times more likely to have good knowledge of BPACR than those who had not heard of BP (OR=2.328; 95%(CI) = 1.176–4.609; p=0.015) (Table 3).
| Variable | Level of Knowledge | Total | Test Statistic | P | |
|---|---|---|---|---|---|
| Fair KnowledgeFrequency (%) | Good KnowledgeFrequency (%) | Frequency (%) n=417 | |||
| Category of health Facility | |||||
| Public | 21(14.9) | 120(85.1) | 141(100.0) | c2=0.39 | 0.53 |
| Private | 35(12.7) | 241(87.3) | 276(100.0) | ||
| Age Group(years) | |||||
| 21-30 | 26(14.5) | 153(85.5) | 179(100.0) | c2=1.14 | 0.77 |
| 31-40 | 23(13.9) | 143(86.1) | 166(100.0) | ||
| 41-50 | 5(9.1) | 50(90.9) | 55(100.0) | ||
| = 51 | 2(11.8) | 15(88.2) | 17(100.0) | ||
| Marital Status | |||||
| Single | 27(16.5) | 137(83.5) | 164(100.0) | c2=3.32 | 0.19 |
| Married | 29(11.9) | 214(88.1) | 243(100.0) | ||
| Others | 0(0.0) | 10(100.0) | 10(100.0) | ||
| Level of Education | |||||
| 10 Completed | 0(0.0) | 1(100.0) | 1(100.0) | fishers exact=16.46 | <0.001 |
| 20 Completed | 15(35.7) | 27(64.3) | 42(100.0) | ||
| 30 Completed | 41(11.0) | 333(89.0) | 374(100.0) | ||
| Designation of HCPs | |||||
| Community Health Practitioners | 8(22.2) | 28(77.8) | 36(100.0) | c2=9.54 | <0.001 |
| Doctors | 4(4.4) | 87(95.6) | 91(100.0) | ||
| Nurses | 44(15.2) | 246(84.8) | 290(100.0) | ||
| Awareness ofBP | |||||
| Yes | 34(9.8) | 312(90.2) | 346(100.0) | c2=22.69 | <0.001 |
| No | 22(31.0) | 49(69.0) | 71(100.0) | ||
| Received Training | |||||
| Yes | 6(3.8) | 154(96.2) | 160(100.0) | c2=20.92 | <0.001 |
| No | 50(19.5) | 207(80.5) | 257(100.0) | ||
| Frequency of training(n=160) | |||||
| 01Feb | 5(4.1) | 116(95.9) | 121(100.0) | fishers exact =2.91 | 0.24 |
| 03Apr | 0(0.0) | 31(100.0) | 31(100.0) | ||
| =5 | 1(12.5) | 7(87.5) | 8(100.0) | ||
Table 3: Factors associated with level of knowledge of BPACR among health care providers in Benin City, Edo State.
Also, HCPs who had secondary completed level of education were 2.9 times less likely to have good knowledge of BPACR than those with tertiary completed level of education and this difference was statistically significant (OR=0.342, 95% CI=0.143-0.821;p=0.016).Finally, HCPs who had not received training were 4.8 times less likely to have good knowledge of BPACR than those who received training (OR=0.207; 95% CI=0.077 - 0.558; p=0.002) (Table 4).
| Variable | Odds ratio | 95% CI | p |
|---|---|---|---|
| Type of Health Facility | |||
| Public Health Facility | 0.633 | 0.301-1.331 | 0.228 |
| Private Health Facility | 1 | ||
| Age group (Years) | |||
| 21-30 | 6.825 | 0 | >0.999 |
| 31-40 | 5.372 | 0 | >0.999 |
| 41-50 | 8.405 | 0 | >0.999 |
| 51-60 | 1 | ||
| Sex | |||
| Female | 1.74 | 0.337-8.989 | 0.509 |
| Male | 1 | ||
| Marital Status | |||
| Single | 0 | 0 | >0.999 |
| Married | 0 | 0 | >0.999 |
| Others | 1 | ||
| Educational Status | |||
| 10 Completed | 5.593 | 0 | >0.999 |
| 20 Completed | 0.342 | 0.143-0.821 | 0.016 |
| 30 Completed | 1 | ||
| Designation of HCPs | |||
| Community Health practitioners | 0.644 | 0.254-1.734 | 0.403 |
| Doctors | 4.428 | 0.969-20.228 | 0.055 |
| Nurse/Midwife | 1 | ||
| Awareness of BP | |||
| Yes | 2.328 | 1.176-4.609 | 0.015 |
| No | 1 | ||
| Received training on BP | |||
| No | 0.207 | 0.077-0.558 | 0.002 |
| Yes | 1 | ||
Table 4: Logistic regression model of factors predicting good knowledge of BPACR among health care providers in Benin City, Edo State.
Discussion
In Africa inadequate human resources for health and health facilities, poor citing of health facilities with inadequate health service coverage are notable challenges plaguing the health system [5]. The health care system in developing countries is characterized by misplaced priorities propagated by corruption, these are well documented factors reported to influence health care service delivery [16,17]. Inadequately trained and skilled health work force that are knowledgeable to render intended health care services to the populace remains a major challenge reported compounding delays in providing skilled health care services, especially in life threatening emergencies [18]. Antenatal care has been reported to provide window of opportunities for information, education and communication by skilled health care providers to pregnant women; so they can be adequately and appropriately empowered with reliable and verifiable information to make informed choices about their health and significant others under any situation they find themselves especially during life threatening emergencies.
This study identified that most of the health care providers studied had good knowledge of BPACR; this was significantly influenced by increasing educational status, awareness and training received in relation to BP. This high level of good knowledge on BPACR among HCPs is an important finding as HCPs who are well informed about the BPACR strategy or any other health intervention could be better informed and knowledgeable about health intervention to disseminate same and inform pregnant women who in turn can become better equipped to make prompt decision during emergency situation.
This study finding is similar to reports from other studies [18-20] in North and South Ethiopia which showed that recently delivered women received antenatal care from skilled health care providers had most of their deliveries by skilled providers.
This study also identified that training received on BP was a significant predictor of good knowledge of BPACR among HCPs, as HCPs who were trained were better knowledgeable about BPACR. This finding buttresses the importance of training and need for training and retraining programmes; as cost effective and useful strategy to enhance knowledge base of health care providers in relation to maternal health issues or any other health intervention, which in turn could impact positively on the knowledge base of their clients to empower them make informed decisions and seek health care services promptly as occasion may warrant. This could in turn positively influence maternal health outcomes by enhancing utilization of skilled care services among pregnant women and significant others. Improved utilization of health intervention in this regard has been reported in previous studies [19-21]. It is also very important to note that if knowledge of health care providers is poor; this could negatively impact on the health seeking behaviour and level of acceptance of health intervention by clients and potential clients.
This finding on good knowledge of BPACR among HCPs identified in this study is in contrast to findings reported from a study [9] in Ile- Ife South Western Nigeria which revealed a poor knowledge among health care providers on the concept of Emergency Obstetric Care. This finding is worrisome as majority of these health care providers reported in the study [9] to have conducted counselling and health education sessions for pregnant women on BPACR during ANC sessions and as such could have communicated wrong information to unsuspecting clients and these can negatively influence their knowledge base and their decision making ability in taking up appropriate health intervention and making informed decision under emergency situation.
Similarly, findings from other studies in Ethiopia [7] and India [8] also identified gaps existing between knowledge and skills of health care providers (HCPs), as only a low proportion of HCPs were competent in diagnosis and management of complication in pregnancy. Although HCPs studied had adequate knowledge of antenatal care they were not able to implement it in real situation. This study finding buttressed the need for repeated practical training of health care providers on standard procedures for better diagnosis and management of emergencies and complications that may occur. Furthermore, the perception of clients about the knowledge, skill of health care providers can influence the level of client utilization of health services from such centers during emergencies as identified in an Ethiopian study [8]; which reported low utilization of health care providers during emergency situation due to perceived negative impression clients have about their knowledge and competence.
This development in relation to negative impression on health care providers’ knowledge, performance and capability is very worrisome especially in developing countries, it has been reported that 99% of all maternal deaths occur in developing countries, the causes are mostly preventable [1,2]. As such pregnant women in need of care or in emergency situation may find it difficult to access skilled and knowledgeable health care providers when the need arises; this may expose unsuspecting clients’ to health care providers who lack satisfactory knowledge, competence and skill to render professional services. Such services at best could be detrimental to the health and wellbeing of mother and child, thus further compounding the already poor maternal and child health indices reported in developing countries. This is a crucial factor which must be well addressed in addition to other factors if we are to adequately appraise the reason for Nigeria failure to meet up with the MDG target of 250 maternal deaths per 100,000 live births for 2015 as we optimistically move into the era of Sustainable Development Goals (SDGs) [3,22].
Conclusion
Majority of health care providers studied had good knowledge of BPACR, with increasing educational status, awareness and training received on BP identified as significant predictors for good knowledge. There is need to sustain health care provider knowledge on this strategy through regular training and retraining programs on BPACR for improved maternal and child health performance.
Acknowledgement
We wish to specially appreciate all respondents who participated in this study, Research assistants, Edo State Ministry of Health, Egor,Ikpoba-Okha and Oredo Local Government councils for permission to carry out this study.
Competing Interest
We wish to state that this study is free of any competing interest and was fully sponsored by the Authors.
References
- (2010) WHO, UNICEF, UNFPA and World Bank trends in maternal mortality: 1990 to 2008: Estimates developed by WHO, UNICEF, UNFPA and The World Bank. Geneva, WHO.
- (2004) World Health Organization (WHO) United Nations Children’s Fund (UNICEF) and United Nations Population Fund (UNFPA). Maternal mortality in 2000: Estimates developed by WHO, UNICEF and UNFPA. Geneva, WHO.
- (2013) National Population Commission (NPC) and ICF International Nigeria demographic and health survey, abujanigeria and rockville, maryland, USA: NPC and ICF international.
- JHPIEGO (2001) Maternal and neonatal health (MNH) program. Birth preparedness and complication readiness: A Matrix of shared responsibilities. Baltimore, MD. JHPIEGO p: 12.
- Kimani M (2008) Investing in the health of Africa’s mothers. Afr Renewal 21: 8.
- (2010) National Primary Health Care Development Agency. The MGD –DRG funded midwives services scheme, concept, process and progress, abuja.
- (2006) Central statistics agency, Ethiopia DHS 2005. Addis Ababa, Ethiopia, ORC Macro Calverton, Maryland, USA.
- Nandan D, Kushwah SS, Dubey DK (2008) A study for assessing birth preparedness and complication readiness intervention in Rewadistrict of Madhya Pradesh pp: 1-34.
- Ijadunola KT, Ijadunola MY, Abiona CT (2010) New paradigm, old thinking: A case of emergency obstetric care in the prevention of maternal mortality in Nigeria. BMC Womens Health 10: 6.
- Federal Republic of Nigeria (2010) Priority table IV on population distribution by age and sex in states and local government areas. National population Commission, Abuja, Nigeria.
- (1999) Eni-Meg Nigeria Limited, Edo State Investors’ Guide. Eni-Meg Lagos 2-256.
- Federal Republic of Nigeria (2010) Priority Table XII on Population distribution by age and sex and literacy rate in States and Local Government Areas. National population Commission Abuja, Nigeria.
- Edo State Ministry of Health (2016) Department of Hospital services, List of Health Facilities.
- (2004) JHPIEGO Maternal and neonatal health: Monitoring birth preparedness and complication readiness, tools and indicators for maternal and newborn health. Johns Hopkins, Bloomberg school of Public Health, Center for communication programs, Family Care International.
- Cochran WG (1977) Sampling techniques New York: John Wiley & Sons.
- ENHANSE Project (2005) Reproductive health situation in Nigeria.
- Sundari TK (1992) The untold story: how the health care systems in developing countries contribute to maternal mortality. International Journal Health Service 22: 513-528.
- (2003) Nigeria Federal Ministry of Health, Reproductive health situation in Nigeria, Abuja: Federal Ministry of Health pp: 1-6.
- Hiluf M, Fantahun M (2007) Birth preparedness and complication readiness among women in Adigrat town, north Ethiopia. Ethiop J Health Dev 22: 14-20.
- Agarwals S, Sethi V, Srivastava K, Jha KP, Baqui AH (2010) Birth preparedness and complication readiness among slum women in Indore City, India. J Health PopulNutr 28: 383-391.
- World Health Organization, United Nations Children’s Fund (2003) Antenatal care in developing countries: Promises, achievements and missed opportuinities. An analysis of trends and differentials, 1990-2001. WHO Geneva.
- (2013) United Nations Economic Commission for Africa Report on Progress in achieving the MDGs in Africa, Addis Ababa, Ethiopia. UNECA.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 13257
- [From(publication date):
October-2016 - Sep 01, 2025] - Breakdown by view type
- HTML page views : 12039
- PDF downloads : 1218