Life Style Modification and Weight Loss Cure Obesity, Metabolic Syndrome, Non-Alcoholic Fatty Liver Disease and Vitamin D Deficiency
Received: 31-Jul-2018 / Accepted Date: 04-Sep-2018 / Published Date: 14-Sep-2018 DOI: 10.4172/2165-7904.1000372
Keywords: Vitamin D and obesity; Vitamin D and NAFLD; Vitamin D; Metabolic syndrome; Weight loss
Background
There is a global prevalence of vitamin D deficiency-insufficiency concordant with the rise of metabolic syndrome-obesity and NAFLD prevalence.
It is now conclusively recognized that obesity and metabolic syndrome causes stimulation of immune system and sustain a chronic inflammatory state in all tissues, especially in islet cells, brain, liver, gut and muscle [1-3]. NAFLD begins with simple fat accumulation in the hepatocytes called Hepatic steatosis, then it triggers oxidative stress and inflammation of the hepatocytes called steato-hepatitis and finally to cellular apoptosis, fibrosis and cirrhosis of liver [4-6].
Though NAFLD has been long recognized as a part of metabolic syndrome but vitamin D deficiency which is increasing pari-passu has rarely been identified as a part of Metabolic syndrome-Obesity- NAFLD-Deficiency complex (MOND syndrome). Hepatologists have acknowledged NAFLD as a leading cause of chronic liver disease worldwide. In a recently concluded work, our group has identified that reversal of fatty liver by weight loss or mere moderate physical activity without weight loss improves vitamin D level in blood [7]. So modern day epidemic of Vitamin D deficiency is due to this MOND syndrome and it could be completely cured by life style modification. The guideline of Endocrine Society is similar for management of NAFLD, where only life style modification and probably vitamin E have been recommended for management of NAFLD [8]. Professional academic bodies (AGA, AASLD, ACG) have recommended, from research evidence, that Life Style Modification improves NAFLD and NASH [9]. Loss of body weight by 3%-5% improves Steatosis and a 10% weight loss improves hepatic necro-inflammation [9,10].
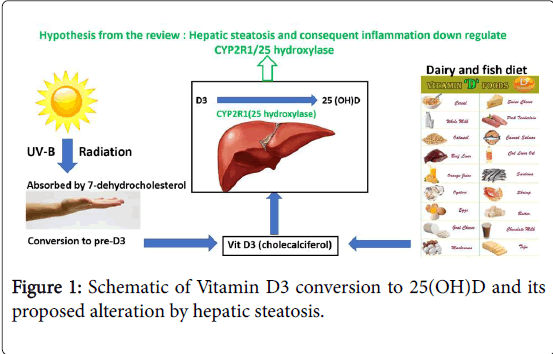
The vitamin D3 produced by skin or consumed in diet e.g dairy products and fish are metabolized in the liver to its proactive form 25- hydroxy vitamin D3, [25(OH)-D] by 25 hydroxylases, a p-450 enzyme. So, with life style modification and loss of body weight in NAFLD subjects, there is an improvement of hepatic pro-inflammatory state, which leads to conversion of vitamin D3 to its intermediary active from 25(OH)D.
Review
Acute deficiency and insufficiency of vitamin D are gaining momentum across the globe, more so over the last two decades. It is rampant even in sun-drenched regions of the world and in ethnic communities known for high fatty fish consumption. The prevalence of vitamin D deficiency in India has been reported as 50% to 90% in different published studies [11,12]. Our group observed the prevalence of vitamin D insufficiency- deficiency is 90% to 100% in non-diabetic and diabetic population respectively [7]. The comparable prevalence in diabetic and non-diabetic population is explained by the fact that the non-diabetic group is full of prediabetic and metabolic syndrome subjects with Body Mass Index (BMI) in the obese compartment. Hence, it is indirect evidence that obesity and metabolic syndrome may be the main etiopathogenic factor of vitamin D deficiency in the index population [13]. According to endocrine society clinical practice (ECSP) recommended guidelines obese children and adults should receive two to three times more vitamin D for their age [14]. Information explaining this higher necessity for vitamin D in this group of subjects is scarce. A possible reason is sheer increase of body weight. In that case there should be some weight-based dosing nomogram. The other possible cause could be the existence of vitamin D resistance in obese and overweight metabolic syndrome subsets which necessitates two to three times more vitamin D [15]. In a study published in The American journal of Clinical Nutrition, Wortsman et al. have attributed the obesity-associated vitamin D insufficiency to the decreased bioavailability of vitamin D3 from cutaneous and dietary sources following its deposition in body fat compartments [16]. Compston et al. postulated that obese individuals suffer from vitamin D deficiency due to decreasing exposure to solar ultraviolet (UV) radiation, the latter being indispensable for the cutaneous synthesis of vitamin D3 [17]. An alternate explanation of the deficiency inducing mechanism is the enhanced production of the active vitamin D metabolite 1, 25-dihydroxyvitamin D, higher concentrations of which exert negative feedback control on the hepatic synthesis of 25(OH)- D [18]. Contrary to these observations, Mercedes Clemente-Postigo and others have observed in a recent study the reduction of 25(OH)-D levels in prediabetic and diabetic subjects in comparison to normoglycemic subjects. This reduction is independent of BMI and is closely related to glucose metabolism variables. The authors suggest that vitamin D deficiency is associated more with carbohydrate metabolism than with obesity [19]. So, from the aforementioned articles, it is clear that obese and metabolic syndrome subjects are more susceptible to vitamin D deficiency but whether obesity causes this directly or indirectly through glucose intolerance is not clear. Next, we attempt to delve deeper into the vitamin D metabolism.
Sun exposure causes ultraviolet-B emanation which is absorbed by 7-Dehydro-cholesterol in the skin, converts it first to previtamin D3, and then to vitamin D3 (cholecalciferol). This vitamin D3 is also available in the diet, mainly in dairy products and fish. The vitamin D3 is metabolized in the liver to its proactive form 25-hydroxy vitamin D3, by 25 hydroxylases, a p-450 enzyme. Among the different hydroxlases responsible for 25 hydroxylation CYP2R1 is the principal enzyme, because homozygous mutation of this enzyme results in vitamin D deficiency [20]. The circulating 25(OH)-D is then converted to its active form 1:25 dihydroxy vitamin D or Calcitriol in the kidneys [21-23]. In kidney diseases due to less 1 alpha hydroxylase activities, less vitamin D3 is synthesized leading to vitamin D deficiency of chronic kidney diseases.
Liver disorder and vitamin D status
In a study conducted at university of Tennessee health science center, Satheesh Nair et al. found prevalence of vitamin D deficiency upto 92.4% in patients of different liver diseases [24]. Similar was the observation in a Spanish study, where 93% of patients with liver diseases had low vitamin D level [25]. So, it is proposed through this review article that liver disorders by impaired 25 hydroxylation causes low circulating level of 25-(OH)D (Figure 1). In a recent article, published in world journal of hepatology, Monjur Ahmed stated that prevalence of NAFLD in western countries is 30% and it is steadily increasing in diabetic and obese subjects to 70% and 90% respectively [26]. In another study in a Chinese population, Jeremy Lok Wei et al. have found prevalence of NAFLD in non-obese subjects 19.3% as compared to three fold raised prevalence in obese subjects of 60.5% [27]. In a review article, Byrne et al. of Southampton University stated NAFLD as the most common cause of chronic liver disease in Western countries. They predicted NAFLD would be the most frequent indication for liver transplantation by 2030 [28].
Epidemic of vitamin D deficiency is concomitant to the epidemic of NAFLD
It is clear from the above articles that obesity-metabolic syndrome and NAFLD are increasing unrestrained in both developing and developed countries over the last few decades. Keeping pace with it, Vitamin D deficiency is also increasing. There is high possibility of inter-relationship of these two health hazards of the modern era. We have found statistically significant relationship between Vitamin D deficiency and higher body mass index [7,13]. Also, we have found high prevalence of elastography proved NAFLD in Vitamin D deficient cohorts. So, obesity, metabolic syndrome and consequent NAFLD cause derangement of normal 25 hydroxy vitamin D synthesis in the liver leading to the decreased circulating 25(OH)D (Figure 1). In one of the intervention study reduction of body weight by life style modification increases Vitamin D level without any supplementation [29]. In another subset of subjects in the above-mentioned study we have seen that thirty minutes of moderate physical activity without weight loss also increases serum vitamin D level significantly.
Conclusion
Vitamin D is a novel biomarker of NAFLD
Low vitamin D level is an important biomarker of obesity-metabolic syndrome and NAFLD. Mere supplementation of vitamin D in case of insufficiency normalizes blood level but does not normalize the underlying malady, probably pro-inflammatory state, behind it, necessitating prolonged supplementation of vitamin D and accepting long term grave complications of NAFLD. NAFLD begins with simple fat accumulation in the hepatocytes called Hepatic steatosis. If not taken care of, it leads to oxidative stress and inflammation of the hepatocytes called steatohepatitis and finally to cellular apoptosis, fibrosis and cirrhosis of liver. Life style modification and reduction of body weight can significantly adapt the normal physiology and deter the development of more deleterious complications of NAFLD. Vitamin D supplementation without addressing the basic pathogenesis of deficiency (which is the usual practice) not only mask the important warning sign of this biomarker but also lead to all possible complications of NAFLD i.e. chronic liver disease and cirrhosis. So, one should not jump for replacement if there is no alteration of calcium-phosphate-PTH axis rather, advise life style modification. To conclude, we will revisit the famous words of a stalwart:
“The doctor of the future will no longer treat the human frame with drugs, but rather will cure and prevent disease with nutrition”-Thomas Edison.
References
- Gregor MF, Hotamisligil GS (2011) Inflammatory mechanisms in obesity. Annu Rev Immunol 29: 415-445.
- Johnson AR, Milner JJ, Makowski L (2012) The inflammation highway: Metabolism accelerates inflammatory traffic in obesity. Immunol Rev 249: 218-238.
- Saltiel AR, Olefsky JM (2017) Inflammatory mechanisms linking obesity and metabolic disease. J Clin Invest 127: 1-4.
- Jou J, Choi SS, Diehl AM (2008) Mechanisms of disease progression in nonalcoholic fatty liver disease. Semin Liver Dis 28: 370-379.
- Masarone M, Rosato V, Dallio M, Gravina AG, Aglitti A, et al. (2018) Role of oxidative stress in pathophysiology of nonalcoholic fatty liver disease. Oxid Med Cell Longev 2018: 9547613.
- Del Campo JA, Gallego P, Grande L (2018) Role of inflammatory response in liver diseases: Therapeutic strategies. World J Hepatol 10: 1-7.
- Chakraboty J KD, Chakraborty S, Chakraborty R, Samanta C (2016) Study of prevalence of vitamin D deficiency in India, in diabetic and non-diabetic population along with its relationship with different variables like BMI, calcium phosphate, PTH, FT4 and TSH. Annual National Conference of Association of Physicians of India.
- Zhu JZ, Hollis-Hansen K, Wan XY, Fei SJ, Pang XL, et al. (2016) Clinical guidelines of non-alcoholic fatty liver disease: A systematic review. World J Gastroenterol 22: 8226-8233.
- Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, et al. (2018) The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology 67: 328-357.
- Dudekula A, Rachakonda V, Shaik B, Behari J (2014) Weight loss in nonalcoholic Fatty liver disease patients in an ambulatory care setting is largely unsuccessful but correlates with frequency of clinic visits. PloS one 9: e111808.
- Londhey V (2011) Vitamin D deficiency: Indian scenario. J Assoc Physicians India 59: 695-696.
- Mehlawat U, Singh P, Pande S (2014) Current status of vitamin-D deficiency in India. Inovat Pharma Pharmacother 2: 328-335.
- Chakraboty J CS, Moitra R (2017) Study of etiopathogenesis of Vitamin D deficiency in South Asia.
- Nair R, Maseeh A (2012) Vitamin D: The “sunshine†vitamin. J Pharmacol Pharmacother 3: 118.
- Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, et al. (2011) Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 96: 1911-1930.
- Wortsman J, Matsuoka LY, Chen TC, Lu Z, Holick MF (2000) Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr 72: 690-693.
- Compston JE, Vedi S, Ledger JE, Webb A, Gazet JC, et al. (1981) Vitamin D status and bone histomorphometry in gross obesity. American J Clinic Nutri 34: 2359-2363.
- Bell NH, Epstein S, Greene A, Shary J, Oexmann MJ, et al. (1985) Evidence for alteration of the vitamin D-endocrine system in obese subjects. J Clini Investi 76: 370-373.
- Clemente-Postigo M, Muñoz-Garach A, Serrano M, Garrido-Sánchez L, Bernal-López MR, et al. Serum 25-hydroxyvitamin D and adipose tissue vitamin D receptor gene expression: relationship with obesity and type 2 diabetes. J Clin Endocrinol Metab 100: E591-E95
- Christakos S, Ajibade DV, Dhawan P, Fechner AJ, Mady LJ (2012) Vitamin D: metabolism. Rheumatic Dis Clinic 38: 1-11.
- Ross AC (2011) The 2011 report on dietary reference intakes for calcium and vitamin D. Public health nutrition 14: 938-939.
- Ross AC, Manson JE, Abrams SA, Aloia JF, Brannon PM, et al. (2011) The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: What clinicians need to know. J Clin Endocrinol Metab 96: 53-58
- Ross AC, Manson JE, Abrams SA, Aloia JF, Brannon PM, et al. (2011) The 2011 Dietary Reference Intakes for Calcium and Vitamin D: What dietetics practitioners need to know. J Am Diet Assoc 111: 524-527.
- Nair S (2010) Vitamin D deficiency and liver disease. Gastroenterol Hepatol 6: 491-493.
- Iruzubieta P, Teran A, Crespo J, Fabrega E (2014) Vitamin D deficiency in chronic liver disease. World J Hepatol 6: 901-915.
- hmed M (2015) Non-alcoholic fatty liver disease in 2015. World J Hepatol 7: 1450-1459.
- Wei JL, Leung JC, Loong TC, Wong GL, Yeung DK, et al. (2015) Prevalence and Severity of Nonalcoholic Fatty Liver Disease in Non-Obese Patients: A Population Study Using Proton-Magnetic Resonance Spectroscopy. Am J Gastroenterol 110: 1306-1314.
- Byrne CD, Targher G (2015) NAFLD: A multisystem disease. J Hepatol 62: S47-S64.
- Chakraboty J CS, Chakraborty R, Naga D (2015) Study of effect of weight reduction on Vitamin D status in obese and overweight subjects-a pilot study. J Vivekananda Inst Med Sci 38: 11-13.
Citation: Chakraborty J, Chakraborty S, Bandopadhyay A, Moitra R (2018) Life Style Modification and Weight Loss Cure Obesity, Metabolic Syndrome, Non-Alcoholic Fatty Liver Disease and Vitamin D Deficiency. J Obes Weight Loss Ther 8: 372. DOI: 10.4172/2165-7904.1000372
Copyright: © 2018 Chakraborty J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4467
- [From(publication date): 0-2018 - Nov 29, 2025]
- Breakdown by view type
- HTML page views: 3559
- PDF downloads: 908