LONG-TERM EFFICACY OF PHOTODYNAMIC THERAPY IN CHRONIC TONSILLITIS: REDUCING RECURRENCE AND AVOIDING SURGERY
Received: 01-May-2025 / Manuscript No. jpcm-25-162928 / Editor assigned: 03-May-2025 / PreQC No. jpcm-25-162928(PQ) / Reviewed: 27-May-2025 / QC No. jpcm-25-162928 / Manuscript No. jpcm-25-162928(R) / Published Date: 31-May-2025
Abstract
Background: Recurrent tonsillitis presents a significant clinical challenge, often requiring surgical intervention when antibiotic therapy fails. Antimicrobial photodynamic therapy (aPDT) has emerged as a promising non-invasive alternative, offering effective microbial load reduction and symptomatic relief without contributing to antibiotic resistance. Methods: assessed the efficacy of aPDT in patients over 18 years old diagnosed with pharyngotonsillitis caused by Streptococcus beta-hemolyticus (SBH). Participants were divided into three groups [1], aPDT alone [2], aPDT combined with anti-inflammatory drugs, and [3], aPDT combined with antibiotics. Patients were monitored for 12 months to evaluate infection recurrence and the need for surgical intervention. Results: The group treated with aPDT alone exhibited no recurrences throughout the 12-month follow-up period, making it the most effective approach. In contrast, patients receiving aPDT combined with anti-inflammatory drugs or antibiotics experienced higher recurrence rates, particularly within the first two months. Importantly, all patients initially recommended for tonsillectomy avoided surgery, with the highest impact observed in the aPDT + antibiotics group (45.5% avoided surgery). Conclusion: aPDT demonstrates significant efficacy in reducing recurrent tonsillitis episodes and preventing surgical intervention. The findings suggest that aPDT, particularly when used as a standalone treatment, can serve as a viable and non-invasive alternative to conventional therapeutic approaches, addressing both infection recurrence and antimicrobial resistance concerns.
Keywords:
Keywords
Photodynamic Therapy; Tonsilitis; Antibiotic; Pain; Infectious diseases
Introduction
Infectious diseases are frequently associated with antibiotic therapy (ATB), as these drugs have been the primary treatment option for bacterial infections for decades. However, their effectiveness does not always meet expectations, mainly due to antimicrobial resistance (AMR), a global public health challenge. The uncontrolled use of antibiotics increases selective pressure on bacteria, accelerating their ability to acquire resistance mechanisms, which can render treatments ineffective [1]. Consequently, finding effective alternatives to antibiotic therapy has become an urgent need, especially for recurrent infections such as chronic tonsillitis. Antibiotics require several conditions to be effective [1], a specific target within the bacterial cell [2], an optimal concentration reaching the infection site, and [3], no degradation or structural modification of the drug [2]. However, chronic tonsillitis is often characterized by persistent infection of the tonsils, and its recurrence is closely linked to antimicrobial resistance. Some cases of tonsillitis decrease in frequency over time, while others persist for life. Additionally, diagnosis is frequently delayed or overlooked due to subtle clinical manifestations and the lack of confirmatory laboratory tests [3].
One of the most significant challenges in treating chronic tonsillitis is the formation of bacterial biofilms. These microbial structures adhere to the surface of the tonsils and protect bacteria from host immune responses and antibiotics, increasing their resistance up to 1,000 times compared to planktonic cells [4]. Studies estimate that 65-80% of bacterial infections involve biofilm formation, which significantly complicates treatment [5]. Biofilms follow a well-defined developmental process: initial adhesion, microcolony formation, biofilm maturation, and dispersion, making them highly adaptable and persistent. Their presence contributes to the chronic nature of infections and increases the likelihood of recurrence even after antibiotic therapy [6]. Given these challenges, alternative antimicrobial strategies are crucial. Photodynamic therapy (PDT) has historical roots in medical applications dating back to Ancient Greece, Egypt, and India, though it’s clinical use remained limited until the 20th century. In 1900, Raab observed that microorganisms exposed to specific dyes and light underwent cell death, laying the foundation for modern photodynamic therapy (PDT) [7]. The principle of PDT is based on the activation of a photosensitizer (PS) with light at a specific wavelength in an oxygen-rich environment, generating reactive oxygen species (ROS) that induce microbial destruction [8]. Antimicrobial photodynamic therapy (aPDT) has emerged as an innovative and effective technique capable of eliminating bacterial pathogens without inducing resistance [9]. Unlike antibiotics, aPDT disrupts biofilms and prevents bacterial recolonization, making it a promising approach for recurrent pharyngotonsillitis [10]. Additionally, aPDT is non-invasive, fast, and easy to apply in outpatient settings, contributing to improved patient quality of life, especially for those who have experienced recurrence despite multiple antibiotic treatments [11]. Recurrent tonsillitis is defined as at least six or more infections per year, one or more respiratory infections per month, or three or more infections of the lower respiratory tract annually [12]. The standard diagnostic approach involves rapid antigen detection tests (RADT) or throat culture for Streptococcus pyogenes, guiding appropriate treatment selection. However, the overuse of antibiotics in these cases can further drive bacterial resistance, reducing treatment effectiveness [13]. Given the high recurrence rates and the limitations of antibiotic therapy, this study aims to evaluate the efficacy of aPDT in treating recurrent pharyngotonsillitis, monitoring its effects over a 12-month period and assessing its potential to reduce recurrence and the need for surgical intervention.
Methodology
Participant Selection and Study Design
The study was conducted at the Photodynamic Therapy Unit of Hospital Santa Casa in São Carlos, State of São Paulo, Brazil. The research protocol was approved by the Human Research Ethics Committee of Hospital Santa Casa (CAAE number: 61720922.9.0000.8148). Adult participants aged 18 years or older from São Carlos/SP, Brazil, who presented clinical signs and symptoms consistent with pharyngotonsillitis (FT) were invited to participate. Screening was performed by a medical professional specializing in otorhinolaryngology. Subsequently, patients underwent routine laboratory procedures at the Photodynamic Therapy Unit (IFSC-USP), located at Santa Casa de Misericordia de São Carlos. All participants provided written informed consent in accordance with Brazilian law 466/2012.
Inclusion and Exclusion Criteria
Eligibility criteria for participation included being over 18 years of age, presenting signs and symptoms of pharyngotonsillitis, and testing positive for Streptococcus pyogenes (SBH). Exclusion criteria were as follows: no history of pharyngotonsillitis in the past two months, current use of antibiotics (ATB), pregnancy, lactation, or having an oncological condition.
Clinical Evaluation and Follow-Up
Patients presenting clinical signs and symptoms of FT, such as fever, erythema, exudate, sore throat, headache and pain, were evaluated based on inclusion and exclusion criteria. Included patients provided a sample from the tonsil region using a swab for rapid detection of SBH. After undergoing photodynamic therapy (aPDT), a clinical reassessment was conducted to observe changes in signs and symptoms following treatment. This reassessment took place at 48 hours and 30 days post-treatment, with patient follow-up continuing for 12 months via telephone contact and self-reported symptom updates.
Antimicrobial Photodynamic Therapy
A total of 38 patients were included in the study and allocated into three defined groups:
- Group 1 (n = 15): Patients using anti-inflammatory or analgesic medications with persistent sore throat, treated concurrently with aPDT.
- Group 2 (n = 11): Patients on antibiotics who had undergone multiple treatment attempts with various medications but continued to exhibit persistent FT symptoms. These patients received aPDT in combination with antibiotics.
- Group 3 (n = 12): Patients presenting FT symptoms without prior use of any medication, receiving exclusive aPDT treatment.
The antibiotics administered included Azithromycin, Benzylpenicillin Benzathine, Amoxicillin, and Potassium Clavulanate. Anti-inflammatory and analgesic medications included Dipyrone, Paracetamol, Cetoprofen, Ibuprofen, and Nimesulide. Patients selected for aPDT received a lozenge- based formulation made of gelatin containing photosensitizers (PS), specifically natural curcumin at a concentration of 0.75 mg/mL, provided by PDT Pharma (PDT Pharma, Cravinhos, São Paulo, Brazil). After the patient sucked the curcumin lozenge for approximately 3 minutes (estimated time until complete dissolution), the oral cavity was illuminated with a blue light-emitting diode (LED) system at a wavelength of 450 nm (Patent: BR10201601347) with an intensity of 20 mW/cm² and energy density of 2.4 J/cm². The equipment was manufactured by MM Optics (MMOptics, São Carlos, São Paulo, Brazil).
Results
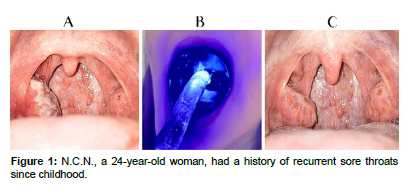
[Figure 1] N.C.N., a 24-year-old woman, had a history of recurrent sore throats since childhood. She reported an average of two infections per year and frequent episodes of inflammation occurring once or twice a month, although without progression to infection. During the anamnesis, the patient reported her main complaints as sore throat, hyperemia and hypertrophy of the oropharynx/tonsils, fever above 38°C, bleeding, neck pain, back pain, body aches, and headache. Upon measuring vital signs, the following parameters were recorded: a temperature of 38.1°C (even after intravenous dipyrone administration), a heart rate of 102 bpm, oxygen saturation of 97%, and blood pressure of 120/80 mmHg. On physical examination, the tonsils were observed to have crypts—small cavities that can trap food, bacteria, and mucus, promoting the formation of tonsillar stones, also known as tonsilloliths or "white spots" in the throat. Additionally, the presence of exudate, edema, hyperemia, and a darker-colored plaque was identified.
It is possible to compare images A and C and observe that, before the treatment with antibiotics concomitant with photodynamic therapy, the patient had a significant bacterial load in the tonsillar crypts, along with hyperemia, edema, and exudate plaques. After the antibiotic treatment and just one application of PDT, the tonsil appears free of exudate plaques, with a noticeable reduction in bacterial load, hyperemia, and edema.
[Table 1] presents the results of the pre-intervention model, which represents the conventional treatment strategies adopted prior to the implementation of antimicrobial photodynamic therapy (aPDT). The data are divided into two categories: antibiotic-based interventions and non-antibiotic-based interventions, which included only anti-inflammatory and/or analgesic treatments. Among the 32 patients who underwent an antibiotic-based intervention, 40.62% (n = 13) did not experience recurrence, while 59.38% (n = 19) had recurrent infections. In contrast, among the 6 patients treated with non-antibiotic-based interventions, only 16.67% (n = 1) remained recurrence-free, whereas 83.33% (n = 5) developed recurrent infections. These results indicate that antibiotic-based interventions provided a 2.4-fold reduction in recurrence rates when compared to non-antibiotic interventions. However, despite this improvement, nearly 60% of patients in the antibiotic group still experienced recurrence, highlighting a persistent clinical challenge.
| Antibiotic-based intervention | Non-antibiotic-based intervention | |
|---|---|---|
| Total | 32 | 6 |
| Patients did not present recurrence | 13 (40.62%) | 1 (16.67%) |
| Patients presented recurrence | 19 (59.38%) | 5 (83.33%) |
Table 1: Results of the pre-intervention model before the use of aPDT.
The high recurrence rates, even with antibiotic use, suggest that conventional antibiotic therapy alone is not sufficient to achieve long-term infection resolution. This persistence could be attributed to bacterial resistance mechanisms, biofilm formation, or incomplete pathogen eradication. Biofilms, in particular, are known to shield bacterial colonies from antimicrobial agents, making infections significantly harder to eliminate. In contrast, the non-antibiotic-based group demonstrated even worse outcomes, with only one patient avoiding recurrence. This reinforces that symptomatic treatment with anti-inflammatory or analgesic drugs alone is insufficient for managing recurrent tonsillitis, as it does not directly target the bacterial load responsible for the infection. These findings underscore the limitations of conventional therapeutic approaches and highlight the need for alternative or adjunctive treatments. The introduction of aPDT offers a promising non-invasive and effective strategy by directly eliminating biofilms, reducing microbial load, and avoiding resistance development. Given the high recurrence rates observed in both groups, aPDT emerges as a potential complementary or standalone solution for improving patient outcomes and reducing the necessity for surgical intervention in cases of recurrent tonsillitis.
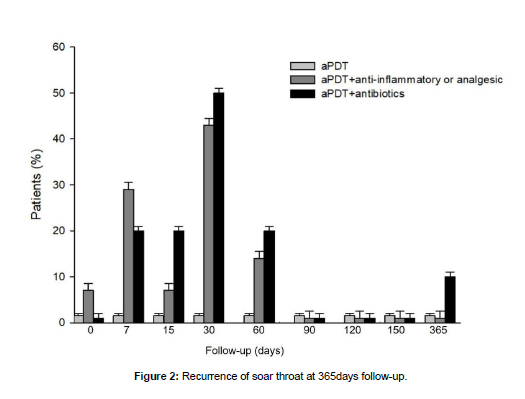
[Figure 2] illustrates the recurrence of throat pain among patients undergoing antimicrobial photodynamic therapy (aPDT) over a one-year follow-up period, comparing its effects when used alone or in combination with anti-inflammatory, analgesic, or antibiotic treatments. The data reveal that patients treated with aPDT combined with anti-inflammatory and analgesic medications exhibited a continuous increase in recurrence rates during the first two months, with notable peaks at 7 days and 1 month. Similarly, patients receiving aPDT combined with antibiotics experienced recurrence episodes between 7 days and 2 months, with peaks observed at 7, 15, and 30 days, as well as a delayed peak at the 12-month mark.
In contrast, the group treated with aPDT alone showed no recurrence at any point during the one-year follow-up period, highlighting its potential as the most effective strategy for long-term symptom control. The absence of recurrence in this group suggests that aPDT alone may provide a more robust and sustained therapeutic effect, possibly due to its biofilm-disrupting properties and ability to eliminate bacterial loads without inducing resistance.
These findings reinforce the limitations of adjunctive pharmacological treatments, as both anti-inflammatory/analgesic and antibiotic combinations with aPDT resulted in higher recurrence rates, particularly in the early months following treatment. The delayed recurrence peak observed in the aPDT + antibiotic group at 12 months may indicate a long-term bacterial recolonization effect, emphasizing the need for alternative or maintenance strategies.
Overall [Figure 2] underscores the superior efficacy of aPDT as a standalone treatment for recurrent pharyngotonsillitis, demonstrating its potential to minimize recurrence and reduce the dependence on conventional pharmacological interventions.
[Table 2] presents the impact of antimicrobial photodynamic therapy (aPDT) on the necessity for tonsillectomy among patients with recurrent tonsillitis, following a one-year intervention and follow-up period. The data demonstrate a significant reduction in the number of patients requiring surgical intervention across all treatment groups.
| Patients out list for tonsillectomy | Patients on list for tonsillectomy | Patients did not require tonsillectomy procedures | |
|---|---|---|---|
| aPDT + Antiinflammatory and Analgesic | 64% | 36% | 100% |
| aPDT + antibiotic | 54.5% | 45.5% | 100% |
| aPDT | 75% | 25% | 100% |
Table 2: Results of the aPDT use regarding patients listed for tonsillectomy procedure.
In the aPDT + anti-inflammatory/analgesic group, 36% of patients were still listed for tonsillectomy, while 64% were removed from the surgical list after treatment. Similarly, in the aPDT + antibiotic group, 45.5% of patients remained on the surgical list, whereas 54.5% no longer required surgery. Notably, the highest success rate was observed in the aPDT-alone group, where 75% of patients were removed from the surgical list, with only 25% still considered for tonsillectomy. These findings highlight the significant role of aPDT in reducing the need for surgical intervention, particularly when used as a standalone treatment. The effectiveness of aPDT alone surpasses that of its combinations with pharmacological therapies, reinforcing its potential as a non-invasive, long-term solution for managing recurrent tonsillitis. Interestingly, despite variations in the percentage of patients who remained on the surgical list, the data indicate that no patient ultimately required tonsillectomy after the one-year follow-up, regardless of treatment group. This underscores the therapeutic success of all aPDT-based interventions, demonstrating their capacity to effectively manage recurrent tonsillitis and prevent surgical procedures.
Discussion
The data presented provide valuable insights into the effectiveness of various therapeutic approaches in treating recurrent throat pain, with a focus on aPDF and its combination with other interventions. Overall, reductions in FT recurrences treated with prior aPDT application remained consistent over one year [12]. Initially, an analysis of [Table 1] shows that the intervention using antibiotics (ATB) significantly reduces the recurrence rate compared to intervention without ATB. While 40.62% of patients treated with ATB did not experience recurrence, only 16.67% of patients who did not use ATB remained free from recurrence. These data reinforce the role of ATB in reducing infection recurrence, although the recurrence rate among those who used them (59.38%) remains significantly high. On the other hand, patients who used only anti-inflammatory and/or analgesics had an even higher recurrence rate, suggesting that this approach alone is less effective in controlling the infection. However, it is important to emphasize that recurrent use of ATB can lead to resistance development and compromise immunity, making infections more frequent; thus, understanding the impact of ATB on bacterial resistance is essential for developing effective technological strategies to combat this global problem [13].
[Figure 1] offers a different perspective by evaluating the effectiveness of aPDT over one year. The analysis shows that the combination of aPDT with anti-inflammatories and analgesics resulted in an increase in recurrences during the first two months, with specific peaks between 7 days and 1 month. A similar pattern is observed in the combination of aPDT with ATB, with recurrences recorded between 7 days and 2 months, as well as a new peak after one year. However, a particularly relevant finding is that the isolated use of aPDT proved to be the most effective approach, as no recurrences were observed during the one-year period analyzed. These results suggest that aPDT alone provides a long-lasting solution for patients with recurrent throat pain
Furthermore [Table 2] highlights the influence of aPDT on patients' need for tonsillectomy surgery. Notably, regardless of the approach used, 100% of patients initially indicated for surgery after one year of therapeutic intervention did not require the surgical procedure due to the excellent response to treatment involving aPDT association. The most significant impact was observed in the group that received aPDT associated with ATB, where 45.5% of patients did not undergo surgery. These results suggest that aPDT can be a viable alternative to avoid invasive surgical procedures. Therefore, the study findings demonstrate that aPDT plays an important role in reducing microbial load and recurrence rates of throat infections, being particularly effective when used alone, although combinations with ATB or anti-inflammatories may still present some recurrences. APDT emerges as a relevant therapeutic option for minimizing the need for surgery and improving patients' quality of life.
Conclusion
This study demonstrates that antimicrobial aPDT is a promising and effective alternative for reducing the recurrence of throat infections and minimizing the need for surgical interventions. The findings suggest that aPDT alone provides superior long-term infection control, while its combination with antibiotics may further enhance its efficacy in preventing recurrences and reducing the necessity for tonsillectomy. The significance of this therapeutic approach is particularly relevant in the current healthcare landscape, where antimicrobial resistance (AMR) poses a major global challenge, compromising the effectiveness of conventional antibiotic treatments. Unlike antibiotics, aPDT does not induce resistance, making it a sustainable and innovative strategy for managing recurrent infections. By directly targeting bacterial loads and disrupting biofilms, aPDT enhances treatment efficacy while preserving antibiotic effectiveness for critical cases. Beyond its microbiological benefits, aPDT stands out as a non-invasive, rapid, and easily accessible intervention, making it a viable option for outpatient management of oropharyngeal infections. In an era where treatment options for recurrent infections are becoming increasingly limited, aPDT emerges as a reliable alternative that aligns with modern strategies to combat AMR. However, the findings of this study provide strong evidence supporting the clinical adoption of aPDT as a safe, effective, and sustainable therapeutic approach for controlling persistent infections. Furthermore, its integration into routine clinical practice could play a crucial role in reducing excessive antibiotic use, thereby contributing to global efforts in mitigating antimicrobial resistance. Future studies should further explore optimal treatment protocols, long-term outcomes, and broader applications of aPDT in infectious disease management.
References
- Mancuso G, Midiri A, Gerace E, Biondo C (2021) Bacterial antibiotic resistance: the most critical pathogens. Pathogens 10: 1310.
- Uddin TM, Chakraborty AJ, Khusro A, Zidan BRM, Mitra S, et al (2021) Antibiotic resistance in microbes: History, mechanisms, therapeutic strategies and future prospects. J Infect Public Health 14: 1750–66.
- Uğraş S, Kutluhan A (2008) Chronic tonsillitis can be diagnosed with histopathologic findings. Eur J Gen Med 5: 1-6.
- Inada NM, Faria G, Silva CS, Kurachi C, Bagnato VS (2020) Antimicrobial Photodynamic Therapy: Challenges and Perspectives. Photodiagnosis Photodyn Ther 29: 101611.
- Bakar MA, McKimm J, Haque SZ, Majumder MAA, Haque M (2018) Chronic tonsillitis and biofilms: A brief overview of treatment modalities. J Inflamm Res 11: 329–37.
- Correia JH, Rodrigues JA, Pimenta S, Dong T, Yang Z (2021) Photodynamic therapy review: Principles, photosensitizers, applications, and future directions. Pharmaceutics 13: 1332.
- Kolarikova M, Hosikova B, Dilenko H, Barton-Tomankova K, Valkova L, et al (2023) Photodynamic therapy: Innovative approaches for antibacterial and anticancer treatments. Med Res Rev 43: 717–74.
- Dube E (2024) Antimicrobial photodynamic therapy: Self-disinfecting surfaces for controlling microbial infections. Microorganisms 12: 1573.
- Guntinas-Lichius O, Geißler K, Mäkitie AA, Ronen O, Bradley PJ, et al (2023) Treatment of recurrent acute tonsillitis—a systematic review and clinical practice recommendations. Front Surg 10:1154307.
- Bakar MA, McKimm J, Haque SZ, Majumder MAA, Haque M (2018) Chronic tonsillitis and biofilms: A brief overview of treatment modalities. J Inflamm Res 11: 329–37.
- Duarte LMP, Santiago IDD, Blanco KC, Bagnato VVS (2024) Use of photodynamic therapy to combat recurrent pharyngotonsillitis: Three case reports. Photodiagnosis Photodyn Ther 104312.
- Soares JM, Guimarães FEG, Yakovlev VV, Bagnato VS, Blanco KC (2022) Physicochemical mechanisms of bacterial response in the photodynamic potentiation of antibiotic effects. Sci Rep 12: 25546.
- Barbosa TM, Levy SB (2000) The impact of antibiotic use on resistance development and persistence. Drug Resist Updat 3: 303-311.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Santiago IDD, Duarte LMP, Blanco KC, Carbinatto FM, Junior AEA, et al. (2025) Long-Term Efficacy of Photodynamic Therapy in Chronic Tonsillitis: Reducing Recurrence and Avoiding Surgery. J Palliat Care Med 15: 764.
Copyright: © 2025 Santiago IDD, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 825
- [From(publication date): 0-0 - Dec 09, 2025]
- Breakdown by view type
- HTML page views: 725
- PDF downloads: 100