Low-frequent Repetitive Transcranial Magnetic Stimulation (rTMS) inAdolescents with Tourette Syndrome
Received: 19-Apr-2017 / Accepted Date: 18-May-2017 / Published Date: 24-May-2017 DOI: 10.4172/2572-4983.1000S1013
Abstract
Objective: The pathophysiology of Tourette syndrome (TS), a chronic motor and vocal tic disorder remains unknown, however abnormalities in basal ganglia-thalamo-cortical circuits presumably play an important role. Repetitive transcranial magnetic stimulation (rTMS), a non-invasive method for modulation of cortical activity, has been applied in different ways in patients with TS.
Methods: Open-label pilot study of active rTMS. Four adolescents with TS participated in the pilot study, two females and two males. The patients fulfilled DSM IV criteria for TS, and had tried psychological and/or pharmacological therapy without effects on symptoms. The rTMS treatment consisted of 10 treatment sessions Monday to Friday during a two-week period. Follow-up was done one, three and six months after finishing the treatment with rTMS.
Results: There was clinically significant improvement in TS symptoms with benefits lasting up to 6 months in two of the patients. In addition, improvement in ADHD was seen in one patient, and improvement in OCD symptoms in another. There were no side effects.
Conclusions: Low-frequency rTMS may be effective in children with TS. Further studies using rTMS in TS are warranted. Careful consideration of target regions and stimulation parameters, longer follow-up, and use of a double-blind, sham-controlled design may allow us to draw founded conclusions in the future.
Keywords: Gilles de la Tourette Syndrome; rTMS; Children
Background
Tourette syndrome (TS) onset during childhood implies that there are both motor and vocal tics [1]. TS may have a chronic course with continuation into adulthood. Since the condition is more common than previously thought (6/1.000 in school children), it is important that physicians in different specialties are aware of the syndrome and its treatment [2]. The TS seems to be a disturbance centrally in the brain including the basal ganglia, particularly the striatum, and parts of the limbic system, although sensorimotor cortex regions also are involved. Some of the transmitters are not working effectively; primarily dopamine, serotonin and norepinephrine are involved in TS. Lack of these or a reduced effect of them in certain parts of the brain result in incorrect impulse control, and hence the typical symptoms of TS arise. These transmitters are also important in compulsive symptoms, impulsiveness, and are involved in motor function and attention [3-5]. Almost all children with TS suffer from other mental disorders in addition to the symptoms of TS, such as ADHD, autism spectrum disorders, depression, learning problems and compulsion. In addition, children with TS have cognitive problems and poor selfesteem, but there are also children who are quite gifted. It is therefore very important to identify individuals with TS and give them adequate medical care, and support socially and in school [6-8].
The most common current treatment modalities are pharmacological and psychological treatment. Pharmacological treatment does not always help, and the drugs used have a lot of side effects as well as weight gain, type II diabetes mellitus, hyperlipidemia, myocarditis, sexual side effects, etc. Another difficulty is that the most adverse effects have been studied in adults [4,9].
Transcranial magnetic stimulation (TMS) is a newly developed tool for assessing functionality of the central nervous system (CNS). After Baker et al demonstrated its value in humans in 1985 [10]. Single and paired-pulse TMS have proven useful in detecting clinical and subclinical abnormalities in a large array of neurological and neuropsychiatric disorders including Tourette's syndrome, obsessive compulsive disorder, depression, schizophrenia, bipolar disorders and ADHD among others [11-15]. There are a lot of studies related to the treatment or diagnosis with TMS of young patients with various neurological or psychiatric diagnoses.
Quintana published in 2005, a review of all the scientific studies that were published on children aged fewer than 18, and he found 48 studies that were published during 1993-2004, with a total of 1, 034 children under the age of 18 years studied. None of these children have had any serious side effects [16]. Both the obsessive compulsive disorders and TS may benefit from TMS treatment through a likely reduction in the specific inhibition of the cerebral cortex. Data reported from a PET study showed increased release of dopamine in the caudate nucleus in persons with TS [17]. Long, slow trains of rTMS (about 1 Hz) delivered to the motor cortex can temporarily reduce corticospinal excitability [18]. Nothing is known for sure about the method's mechanism of action on Tourette syndrome. The degree of efficacy of rTMS treatment of tics varies between studies, but one should keep in mind that conditions vary including respect to the treatment given. There are some studies that suggest post effects [19-22], and others who do not have any significant effect on tics [23,24]. An Italian study, published in 2006, examined whether lowfrequency rTMS was able to normalize the overactive motor cortex, thereby improve tics and compulsive symptoms. Clinical improvement was seen already after one week of treatment. During the second week of treatment statistically significant improvement in the various assessment tools used was obtained.
Improvement of symptoms persisted at the 3 months follow-up. Also normalization of motor cortex activity was obtained. None of the participants had any side effects from the treatment [25]. In an open label 12 weeks cohort pilot study by Kwon et al., 1 Hz rTMS was applied over the SMA (Supplemental Motor Area) for 10 days [22]. At the end of each day subjects completed objective ratings of ADHD, mood, anxiety, tics, and side effects. Statistically significant reductions were seen in the Yale Global TS Severity Scale over the 12 weeks of the study. Le et al. tested the effect of 1 Hz rTMS upon the SMA in 25 children with TS (aged less than 16 years) for 20 days [21]. Results document a significant improvement of clinical symptoms. Interestingly, the benefits lasted for up to 6 months in 68% of subjects. Adverse effects that may occur after rTMS treatment are mild and transient, such as muscle tension, headache and sore throat. Ringing in the ears and temporary hearing loss may occur. Memory problems and cognitive defects are very rare and always temporary. It is described that rTMS can induce seizures in approximately 1 per 1, 000 or less while there is no risk of developing epilepsy.
Aims of the study
The current pilot study aimed at answering these questions: 1. Does rTMS have a therapeutic effect in Tourette's syndrome? 2. If so, how long duration have any positive effects of treatment series with rTMS? 3. What side effects are there with rTMS treatment?
Materials and Methods
Inclusion criteria for patients were: Individuals (15-19 years) meeting the DSM-IV criteria for TS, which have had a pharmacological and/or psychological treatment without any significant effect of symptoms in the study. Persons with a history of epilepsy, skull trauma or metal material in the body were excluded.
The study was approved by the Ethical Committee at the University of Uppsala. Four adolescents with TS participated in the pilot study, two males and two females, aged from 15 years 5 months to 18 years 3 months (median 16 years). The oldest was a male with Tourette syndrome (TS) and obsessive compulsive disorder (OCD), who had been receiving pharmacological treatment with sertraline.
The other male had TS, severe stuttering and attention deficit disorder (ADD). He had been receiving pharmacological treatment with metylphenidate. One girl had TS and OCD and the other girl had, in addition to TS, attention deficit hyperactivity disorder (ADHD). Both girls had previously been treated with different pharmacological drugs, however without satisfying effects. In those with continued pharmacological treatment there was no change of this in connection with the study.
Procedure
Before treatment
One month before the beginning of rTMS treatment, the participants underwent clinical examination by a paediatric neurologist (NK), and visited the neurophysiologic laboratory to get acquainted. At this time also thresholds to hand muscles (abductor pollicis brevis muscle on left and right side) were obtained by single pulse TMS. The patients were asked, by help of their parent/s, to fill in forms regarding severity of their tics TSSS (TSSS: Tourette Syndrome Severity Scale), developed by Shapiro and Shapiro [26], which includes a composite clinical rating of severity comprising five factors.
Scores for the five items are summed and converted to a qualitative global severity rating. The scoring of tic severity ranges from 0 (none) to 9 (very severe). The TSSS is simple to use, appears valid, is highly reliable when used by physicians and provides an overall index of tic severity. Hyperactivity was measured with the parent’s version of the Conners scale [27]. Conners Scale is widely used in ADHD research and comprises ten items pertaining to inattention and hyperactivity. A four step response format (0-3) was used for each item, and scale scores were computed as the sum of item scores. The possible range was 0-30, with higher scores indicating higher hyperactivity level.
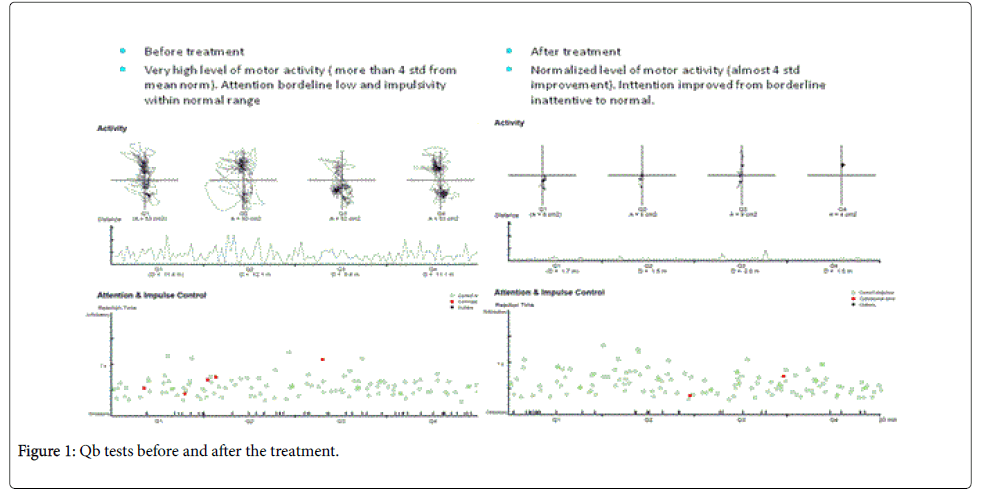
To estimate compulsory symptoms BOCS (Brief Obsessive Compulsive Scale-BOCS) was used. BOCS was created by Susanne Bejrot and is a simplification and abbreviation of the Y-BOCS and CYBOCS scales. The degree of severity of the compulsory problem is measured by six questions. Each one can give 0-4 points. The six questions touch time, obstacles difficulties, control and avoidance, and are the basis for the 24 total amounts of points in BOCS. Eight points or more indicate a time-craving treatment OCD [28,29]. The participants also performed a Qb Test-Plus, which objectively measures all three symptoms of ADHD (hyperactivity, inattention and impulsivity) [30,31].
Treatment
The rTMS treatment consisted of 10 treatment sessions Monday to Friday afternoon during a two-week period. The subject was comfortably seated during the treatment, and a pair of earmuffs was offered in order to avoid the clicking sound of TMS. Stimuli were delivered with the Mag Pro R 30 repetitive stimulator (MagVenture, Farum, Denmark), connected with a large circular coil.
Before rTMS was started, the threshold for evoking a muscle response in the right and left abductor pollicis brevis muscle (APB) was checked, and compared to thresholds obtained one month before treatment (Table 1). Thereafter rTMS started, delivering 1 pulse per second over the cortical hand area at threshold stimulation, with 600 pulses given on each side, with a short pause after each 300 stimuli to cool the coil. By visual inspection responding twitches of APB, on the left and right side respectively, was followed.
| Gender | Age (years) | Threshold %MEPto hand muscle (APB*) | Stimulation frequency (pps) | Number of stimuli per day for 10 days | Adverse effects | ||
|---|---|---|---|---|---|---|---|
| Right | Left | Right | Left | ||||
| Case 1 male | 18 | 45 | 45 | 1 | 600 | 600 | none |
| Case 2 male | 15 | 45 | 45 | 1 | 600 | 600 | none |
| Case 3 female | 16 | 50 | 50 | 1 | 600 | 600 | none |
| Case 4 female | 16 | 55 | 55 | 1 | 600 | 600 | none |
*APB: Abductor PollicisBrevis muscle;pps: Pulses Per Second; ADHD: Attention Deficit Hyperactivity Disorder
1 TS+OCD
2 TS+severestuttering+ADD
3 TS+OCD
4 TS+ADHD
Table 1: Treatment with rTMS in four subjects with Tourette syndrome.
Follow-up
Follow-up was done one, three and six months after finishing the treatment with rTMS. The follow-up included a medical examination, Qb test-Plus, and filling in the same forms concerning tics, behavior and compulsion as before the treatment started.
Results
All four participants completed the treatment. No adverse effects were noted. There were no seizures, neurological complications or complaints about memory or concentration difficulties (no formal test of cognition was done). Two male youths fulfilled the follow-up at one, three and six months after treatment. One female was not able to complete the Qb test because she had so many motor tics (head shaking and turning of the upper body). The other female did not do the Qb test after 6 months because she did not want to. An overview of the results is given in Tables 2 and 3.
| Gender | Time interval | TSSS | Conners | BOCS |
|---|---|---|---|---|
| Case 1 male | Pre treatment | 8 | 2 | 17 |
| 1months after | 7 | 1 | 18 | |
| 3 monthsafter | 2 | 2 | 7 | |
| 6 monthsafter | 1 | 1 | 4 | |
| Case 2 male | Pre treatment | 5 | 8 | 1 |
| 1monthsafter | 7 | 9 | 0 | |
| 3 monthsafter | 3 | 8 | 0 | |
| 6 monthsafter | 2.5 | 6 | 1 | |
| Case 3 female | Pre treatment | 8 | 6 | 20 |
| 1monthsafter | 8 | 3 | 18 | |
| 3 monthsafter | 7 | 4 | 20 | |
| 6 monthsafter | 8 | 3 | 21 | |
| Case 4 female | Pre treatment | 8 | 20 | 6 |
| 1monthsafter | 8 | 16 | 6 | |
| 3 monthsafter | 6 | 11 | 3 | |
| 6 monthsafter | 6 | 9 | 10 |
Table 2: Outcome on TSSS, Conners scale, BOCS, in four adolescents with Tourette syndrome (TS).
| Gender | Age (years) | Motor tics | Vocal tics | ADHD/ADD | Stuttering | OCD | 1 mo.after treatment | 3 mo.after treatment | 6 mo.after treatment |
|---|---|---|---|---|---|---|---|---|---|
| Case 1 male | 18 | + | + | + | improved | improved | Normalised | ||
| Case 2 male | 15 | + | + | + | + | no change | improved | improved | |
| Case 3 female | 16 | + | + | + | no change | no change | no change | ||
| Case 4 female | 16 | + | + | + | no change | improved* | improved* |
*improved concentration
Table 3: Clinical characteristics and total outcome in four adolescents with Tourette syndrome (TS), treated with rTMS.
Case 1: An 18-year old male with TS and OCD had a clinically significant improvement, with a reduction in TSSS; he had 8 points before treatment, 2 points after 3 months, and 1 point after 6 months of treatment. BOCS scores were 17 points at the beginning, 18 points after 1 month, 7 points after 3 months and 4 points after 6 months. The Qb test and Connors scale were within the normal range both before and after treatment.
Case 2: A 15-year old male with TS, ADD and severe stuttering reported a decrease in symptom severity, from severe to moderate with significant reduction in TSSS. He had a clinically significant improvement, with a reduction in TSSS; before treatment 5 points, one month after treatment 7 points, at three months 3 points, and six months after treatment 2,5 points. Connors results were 8 points before treatment, one month after treatment 9 points, and 8 points and 6 points respectively after three and six months. According the BOCS and Qb test there was no difference before and after treatment.
Case 3: A female 16 years of age did not have any effect on the tics or compulsion, TSSS scores were unchanged (8 points before and after treatment). BOCS were 20 points before treatment and 21 points after. Conners scores were 6 points before and 3 points after treatment. She did not do any Qb test because she had so many motor tics, which made it difficult for her to sit in front of computer and complete it.
Case 4: A female 16 years of age with motor tics and ADHD scored TSSS before the treatment 8 points, one month after treatment 8 points, and three and six months after treatment 6 points respectively. BOCS were 6 points before the treatment, 6 points after one month, 3 points after three months and 10 points six months after treatment. Connors score were 20 points before treatment, one month after treatment 16 points, at 3 months 11 points and six months after the treatment 9 points. Qb tests showed an improved activity level and even better oversight. Clinically it is noticeable that she has less tics and better concentration in school (Figure 1).
Discussion
This pilot study sought to discern whether there is a possible effect of rTMS in subjects diagnosed as having TS. A clinically significant improvement in TS symptoms with benefits lasting up to 6 months was seen in two of the patients, similar to that reported [19-22]. Improvement in ADHD was also seen in one patient and another one was improved in his OCD symptoms. There were no side effects of rTMS. This pilot study is the open design and the small size of the group. Making a placebo response is less likely since TS patients are recognized to have a low placebo response [32,33] in comparison to patients with other psychiatric disorders, and our patients had been ill for a long period of time and had tried many treatments previously without success. Further studies using repetitive transcranial magnetic stimulation in TS are warranted. Careful consideration of target regions and stimulation parameters, longer follow-up, and the use of a double-blind, sham-controlled design may allow us to draw founded conclusions in the future.
Declaration of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Acknowledgment
We are grateful to all parents and children who participated.
References
- American Psychiatric Association (1994) Diagnostic and statistical manual of mental disorder. In: Williams JBW, Spitzer RL (eds.) Washington DC.
- Khalifa N, Von Knorring AL (2003) Prevalence of the tic disorders and Tourette syndrome in a Swedish school population. Dev Med Child Neurol 45: 315-319.
- Groenewegen HJ, Van den HOA, Cath DC, Voorn P, Veltman DJ (2003) Does an imbalance between the dorsal and ventral striatopallidal systems play a role in Tourette’s syndrome? A neuronal circuit approach. Brain Development 25: 3-14.
- Dean W, James B, Harvey S, David JS,HirotoK (2008) Mechanisms of Dopaminergic and Serotonergic Neurotransmission in Tourette Syndrome: Clues from an In Vivo Neurochemistry Study with PET. Neuropsychopharmacology 33: 1239-1251.
- Khalifa N, von Knorring AL (2006) Psychopathology of Tourette syndrome and other tic disorders in a total population of school children. J Am Acad Child Adolesc Psychiatry 45: 11-1346.
- Kadesjö B, Gillberg C (2000) Tourettes´s Disorder:Epidemiology and comorbidity in primary school children. J Am AcadAdolesc Psychiatry 39: 548-555.
- Khalifa N, Dalan M, Rydell AM (2010) Tourette syndrome in the general child population: cognitive functioning and self-perception. Nordic Psychiatry 64: 1-11.
- Robertson MM (2000) Tourette syndrome, associated conditions and the complexities of treatment. Brain 12: 425-462.
- Barker AT, Jalinous R, Freeston IL (1985) Non-invasive magnetic stimulation of the hyman motor cortex. Lancet 1: 1106-1107.
- Transcranial magnetic stimulation (TMS) at depression (2001) SSM-rapport Nr 6.
- Frye RE, Rotenberg A, Ousley M, Pascual-Leone A (2008) Transcranial magnetic stimulation in child neurology: Current and future directions. J Child Neurol 23: 79-96.
- George MS, Belmaker RH (2000) Transcranial Magnetic Stimulation in Neuropsychiatry. American Psychiatric Press. Washington DC.
- Buchmann J, Wolters A, Haessler F, Bohne S, Nordbeck R (2003) Disturbed transcallosally mediated motor inhibition in children with attention deficit hyperactivity disorder (ADHD). Clin Neurophysiol 114: 2036-2042.
- Moll GH, Heinrich H, Rothenberger A (2001) Transcranial magnetic stimulation in child and adolescent psychiatry: excitability of the motor system in tic disorders and/or attention deficit hyperactivity disorders. Z Kinder JugendpsychiatrPsychoter 29: 312-323.
- Quintana H (2005) Transcranial magnetic stimulation in persons younger than the age of 18. J ECT 21: 88-95.
- Strafella AP, Paus T, Barrett J, Dagher A (2001) Repetitive transcranial magnetic stimulation of the human prefrontal cortex induces dopamine release in the caudate nucleus. J Neurosci 21: 1-4.
- Speer AM, Kimbrell TA, Wassermann EM, Repella JD, Willis MW (2000) Opposite effects of high and low frequency rTMS on regional brain activity in depressed patients. Biol Psychiatry 11: 1133-1141.
- Chae JH, Nahas Z, Wasserman E, Li X, Sethuraman G (2004) A pilot safety study of repetitive transcranial magnetic stimulation (rTMS) in Tourette syndrome. Cognitive and Behavioral Neurology 17: 85-91.
- Karp BI, Wasserman EM, Porter S, Hallett M (1997) Transcranial magnetic stimulation acutely decreases motor ties. Neurology 48: 227.
- Le K, Liu L, Sun M, Xia N (2013) Transcranial magnetic stimulation at 1 Hertz improves clinical symptoms in children with Tourette syndrome for at least 6 months. J Clin Neurosci 257-262.
- Kwon HJ, Lim WS, Lim MH, Lee SJ, Hyun JK (2011) 1-Hz low frequency repetitive transcranial magnetic stimulation in children with Tourette’s syndrome. Neuroscience letters 492: 1-4.
- Munchau A, Blom BR, Thilo KV, Timble MR, Rothwell JC (2002) Repetitive transcranial magnetic stimulation for Tourette syndrome. Neurology 59: 1789-1791.
- Orth M, Kirby R, Richardson MP, Snijders AH, Rotwell JC (2005) SubthresholdrTMS over pre-motor cortex has no effect on tics in patients with Gilles de la Tourette syndrome. Clinical Neurophysiology 116: 764-768.
- Mantovan A, Lisanby SH, Pieraccini F, Ulivelli M, Castrogiovanni P (2006) Repetitive transcranial magnetic stimulation (rTMS) in the treatment of obsessive-compulsive disorder (OCD) and Tourette ´s syndrome (TS). Int J of Neuropsychopharmacology 9: 95-100.
- Shapiro A K, Shapiro ES, Bruun RD, Sweet RD (1978) Gilles de la Tourette’s syndrome. Raven Press. New York.
- Conners C (1990) Conners Rating Scales Manual, Conners Teacher Rating Scales, Conners Parent Rating Scales. Instruments for use with children and adolescents. North Tonawand, NY; Multihealth systems.
- Scahill L, Riddle MA, McSwiggin-Hardin M, Ort SI, King RA (1997) Children`s Yale-Brown obsessive compulsive scale: reliability and validity. J of the Am Academy of Child & Adolescent Psychiatry 36: 844-852.
- Bejerot S (2002) Tvångssyndrom/OCD. Nycklarpåbordet. Stockholm, Cura. Sweden.
- Sharma A, Singh B (2009) Evaluation of the role of Qb testing in attention deficit hyperactivity disorder. Arch of Disease in Childhood 94:A72.
- Brocki KC, Tillman CM, Bohlin G (2010) CPT performance, motor activity, and continuous relations to ADHD symptom domains: A developmental study. Eur J of Dev Psychology 7: 178-197.
- De La Fuente-Fernandez R, Schulzer M, Stoessi AJ (2002) The Placebo effect in neurological disorders. Lancet Neurology 1: 85-91.
- Huppert JD, Schultz LT, Foa EB, Barlow DH, Davidsson JR (2004) Differential response to placebo among patients with social phobia, panic disorder, and obsessive-compulsive disorder. Am J of Psychiatry 161: 1485-1487.
Citation: Khalifa N, Eeg-Olofsson KE (2017) Low-frequent Repetitive Transcranial Magnetic Stimulation (rTMS) in Adolescents with Tourette Syndrome. Neonat Pediatr Med 3: S1013. DOI: 10.4172/2572-4983.1000S1013
Copyright: © 2017 Khalifa N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5596
- [From(publication date): 0-2015 - Nov 29, 2025]
- Breakdown by view type
- HTML page views: 4627
- PDF downloads: 969