Review Article Open Access
Magnetic Endoscopic Imaging: A Useful Ally in Colonoscopy
Imdadur Rahman*, Stavroula Pelitari, Philip Boger and Praful Patel
Department of Gastroenterology, University Hospital Southampton, Southampton, SO16 6YD, UK
- *Corresponding Author:
- Imdadur Rahman
Department of Gastroenterology
University Hospital Southampton
Southampton, SO16 6YD, UK
Tel: 44 23 8077 7222
Email: imd81@hotmail.com
Received date: August 17, 2015 Accepted date: September 14, 2015 Published date: September 21, 2015
Citation: Rahman I, Pelitari S, Boger P, Patel P (2015) Magnetic Endoscopic Imaging: A Useful Ally in Colonoscopy. J Gastrointest Dig Syst 5:342. doi:10.4172/2161-069X.1000342
Copyright: © 2015 Rahman I, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Magnetic endoscopic imaging (MEI) allows the configuration of the endoscope shaft to be visualised during colonoscopy. In particular, it allows the operator to confidentally recognise loop formation and subsequent loop resolution which is vital for colonoscope tip advancement and thus complete visualisation of the colon. Although generally accepted as a useful aid during colonoscopy, it is not universally available either due to cost or this facility is not available or compatible with all manufactured endoscopes. The data on its utility with regards colonoscopy performance outcome measures is mixed but overall likely to be beneficial. Its main value probably relates to colonoscopy training and its value may be realised with the large expansion in workforce required with the recent introduction of bowel cancer screening. Further work in this area is required. The manufacturer suggests some minor limitations in use because of potential interference with implanted electronic device, but its safety overall is well recognised.
Keywords
Endoscopic; Colonoscopy
Background and Introduction
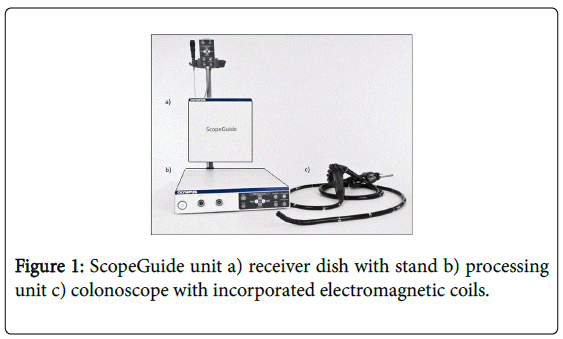
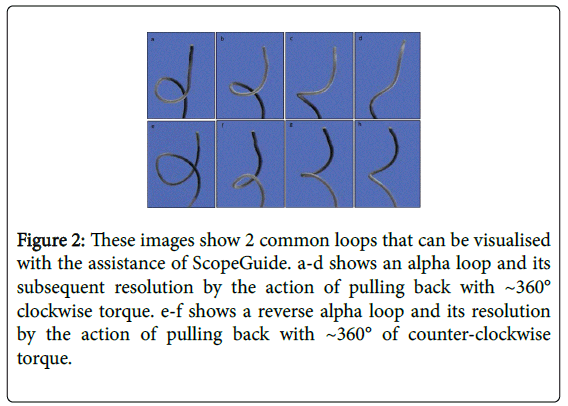
Colonoscopy is undertaken worldwide and is now the set standard for the assessment of the colon. Quality control requirements by endoscopy regulators, such as the joint advisory group in gastrointestinal endoscopy (JAG) in the UK, have mandated the need for institutions undertaking these procedures to record performance outcome measures. A marker of such performance is the caecal intubation rate, however, reports have shown considerable variation between individuals and institutions [1]. There have been several reasons given for failure to reach the caecum. One of the commonest factors elucidated in quality assurance audits is recurrent colonic looping leading to a consequent lack of advancement of the endoscope tip, and subsequent patient discomfort [1]. Measures to appreciate colonoscopic positioning in the past required fluoroscopy, however, its use was cumbersome, posed a radiation risk and views were suboptimal [2,3]. In 1993, Bladen et al. described a non-radiological technique for three dimensional imaging of the colonoscope, magnetic endoscopic imaging (MEI) [4]. This was then further developed by Olympus® into a mobile unit called ‘endoscopic position detecting unit’ or more commonly known as ‘Scopeguide®’. This technology provides a real time three-dimensional image of the colonoscope as it passes through the colon. The basic principle relies on the generation of pulsed low intensity magnetic fields generated from electromagnetic generator coils positioned at regular intervals within the colonoscope. This is then picked up by sensors on a receiver dish which allow calculation of the precise position and orientation of the colonoscope. The image is displayed in anteroposterior or lateral views (or both views together) on the endoscope monitor adjacent to the colonic lumen image (Figure 1). This enables loops to be visualised and loop resolution to be performed under direct vision as the endoscopist can appreciate the type and extent of looping. The direction and degree of rotational manoeuvres that will subsequently be required to straighten out the specific loop formation can then be logically undertaken (Figure 2).
Figure 2: These images show 2 common loops that can be visualised with the assistance of ScopeGuide. a-d shows an alpha loop and its subsequent resolution by the action of pulling back with ~360° clockwise torque. e-f shows a reverse alpha loop and its resolution by the action of pulling back with ~360° of counter-clockwise torque.
MEI Use in Clinical Practice
It was proposed that the use of this device could improve caecal intubation rates, caecal intubation times and even patient comfort. This was demonstrated in the first randomized controlled trial (RCT) of MEI on colonoscopy performance in adults [5]. This study compared colonoscopy using MEI against conventional colonoscopy without. There was significant improvement overall in caecal intubation rates of 100% v 90% (p=0.01) between the MEI and non- MEI group, and a significant reduction of caecal intubation times by 23% (p=0.01) in inexperienced endoscopist and 14% (p=0.04) in experienced endoscopists. However, more recent studies have demonstrated conflicting results. Of the 11 RCTs that have been published since, comparing MEI to conventional endoscopy (when using the same colonoscope) only one has shown higher caecal intubation rates [6], two have shown better caecal intubation times [7,8], one has shown the need for less sedation [8] and three have shown that patient comfort scores were better with MEI [7-9]. A recent meta-analysis of all RCTs. which included a total of 4470 patients, found that MEI was associated with a significantly lower risk of failed caecal intubation (a risk difference of 4%, 95 %CI 0 % -7 %; P = 0.03), lower caecal intubation times (mean difference of 0.58 minutes, 95 %CI 0.28 - 0.88; P < 0.001) and lower pain scores as estimated by visual analogue scale (mean difference 0.45 cm, 95 %CI 0.03- 0.86; P = 0.03) compared with conventional colonoscopy [10]. However, there was considerable heterogeneity amongst the trials and it is arguable whether such difference in caecal intubation times and pain scores are clinically significant. Furthermore, when sensitivity analysis of high quality studies were performed there was no statistical differences in any outcome measures.
One of the larger RCTs on MEI (n=810) did however reveal that in less experienced endoscopists the caecal intubation rate was significantly better in those using MEI compared to standard colonoscopy [11]. In addition the need for assistance with the procedure from a senior colleague was significantly less in the group utilising MEI (19% v 40%, p=0.02). This may lead to the conclusion that the benefit of the device may be more of a training tool for trainee endoscopists through identification of loops, as shown by similar performance improvements in this group in other cohort studies [12-14].
The recording of the subjective measure of trainee and trainer satisfaction is often overlooked and not recorded in studies. As the dynamics of the colon can be visualised, there can be a more logical discussion between the trainer and trainee, to resolve an issue of lack of tip advancement or patient discomfort. In practice, trainees appear to be more satisfied with the use of MEI during colonoscopy. One explanation for this is that it enables the trainer to explain the decision making required to facilitate tip advancement without taking the colonoscope over from the trainee.
In addition to loop recognition, the three dimensional image of the colonoscope generated by MEI can assist in identifying the location of the tip of the scope. This can be useful for documenting where routine biopsies or polyps are taken from as well as aiding in identifying the location of colonic tumours, the latter which in the past has demonstrated inconsistency with surgical findings in as much as in 21% of cases with conventional colonoscopy [15]. A study by Ellu et al which used MEI to locate colonic tumour location, found that MEI had a 94% concordance with surgery, compared to computed tomography which only correctly identified locations in 83% of case [16].
Why is there a discrepancy in performance outcome measures?
Some of the reasons for the differences in study outcomes not showing statistical differences is likely as a consequence of studies being underpowered, with an overestimate of the effect size of MEI which is likely to be less over recent years as the standard of colonoscopy has improved [1]. It is also not clear if endoscopist in the studies that were undertaking colonoscopy with MEI had received training on image and loop recognition and whether the process of loop reduction under direct vision was thoroughly understood. Each individual has a finite capacity of working memory to process information and it is hence plausible that if the near maximum is reached by the basic task, such as a challenging colonoscopy, any additional information is likely not to be processed [17]. We know from other skill acquisition studies that additional stimuli, such as the image from ScopeGuide, could in fact be detrimental to the performance of the operator if the visual stimulus is not understood [18]. In addition, experienced endoscopist who are already high performers may already be receiving proprioceptive stimulus on the configuration of the colonoscope without the additional need of a visual stimulus for guidance. These endoscopist are also likely to have a long established methodology, which is imprinted into their long term memory, which would require extra demands on their cognition to process and undertake the procedure in an alternative way, and hence derive no benefit from the use of MEI [19].
Safety Concerns
There is very minimal safety concerns with MEI, but, as with other devices that generate an electromagnetic field it is currently contraindicated for use in patients with implantable electronic medical devices such as permanent cardiac pacemakers or implantable cardioverter defibrillators. This is as a result of concerns that MEI may interfere with the device causing some sort of dysfunction. However, this worry seems to be unfounded and hypothetical and recent research conducted by Corbett et al suggests that no such interference occurs. A 100 patients with implanted cardiac devices had a colonoscope, which employed MEI, placed on their abdomen over their clothing [20]. Cardiac monitoring and device interrogation was undertaken before, during and after this procedure, which lasted for 2 minutes. For all patients there was no evidence of interference with the device leads or change in programming from exposure to the electromagnetic field generated by the MEI unit. Although there were several limitations to this preliminary study, such as the relatively minimum exposure time and procedure occurring outside the colon, it does suggest that its use is likely to be safe in patients with implantable cardiac devices. In addition, there are several domestic devices that are deemed safe for use in this category of patients that actually have a higher electromagnetic field generated, such as an induction hob cooker [21]. However trials in a real time setting with patient’s undergoing colonoscopy employing MEI would need to occur before firmer conclusions are drawn and recommendations made.
Conclusion
MEI is not in general routine practice on all endoscopy procedures, in part because they are expensive to purchase and require the use of specialised equipment. However, with the growing pressure to train a greater number of generic healthcare endoscopists, the additional cost may thus be justified. Other endoscope manufacturers, such as Pentax®, are in the development phase of incorporating MEI into their colonoscopes. It is hence very likely that this technology becomes increasingly embedded in day to day colonoscopy practice in the future. However, it is important when any such new technology is employed that it is done so with a thorough understanding of how to utilise its maximum potential, as mentioned in this review.
References
- Gavin DR, Valori RM, Anderson JT, Donnelly MT, Williams JG, et al. (2013) The national colonoscopy audit: a nationwide assessment of the quality and safety of colonoscopy in the UK.Gut 62: 242-249.
- Cirocco WC, Rusin LC (1996) Fluoroscopy. A valuable ally during difficult colonoscopy.SurgEndosc 10: 1080-1084.
- Williams CB, Laage NJ, Campbell CA, Douglas JR, Walker-Smith JA, et al. (1982) Total colonoscopy in children.Arch Dis Child 57: 49-53.
- Bladen JS, Anderson AP, Bell GD, Rameh B, Evans B, et al. (1993) Non-radiological technique for three-dimensional imaging of endoscopes.Lancet 341: 719-722.
- Shah SG, Brooker JC, Williams CB, Thapar C, Saunders BP (2000) Effect of magnetic endoscope imaging on colonoscopy performance: a randomised controlled trial.Lancet 356: 1718-1722.
- Hoff G, Bretthauer M, Dahler S, Huppertz-Hauss G, Sauar J,et al. (2007) Improvement in caecal intubation rate and pain reduction by using 3-dimensional magnetic imaging for unsedated colonoscopy: a randomized trial of patients referred for colonoscopy. Scand J Gastroenterol 42: 885-889
- Szura M, Bucki K, Matyja A, Kulig J (2012) Evaluation of magnetic scope navigation in screening endoscopic examination of colorectal cancer.SurgEndosc 26: 632-638.
- Jelsness-JA¸ Rgensen LP, Lerang F, Sandvei P, Saberg T, et al. (2004) Magnetic endoscopic imaging during colonoscopy is associated with less pain and decreased need of analgesia and sedation--results from a randomized controlled trial. Scand J Gastroenterol 48: 890-895.
- Ignjatovic A, Thomas-Gibson S, Suzuki N, Vance M, Palmer N, et al. (2011) Does scope guide improve caecal intubation? A randomized controlled trial. GastrointestEndosc 73: AB307.
- Mark-Christensen A, Brandsborg S, Iversen LH (2015) Magnetic endoscopic imaging as an adjuvant to elective colonoscopy: a systematic review and meta-analysis of randomized controlled trials.Endoscopy 47: 251-261.
- Holme A, Haie O, Matre J, Stallemo A, Garborg K, et al. (2011) Magnetic endoscopic imaging versus standard colonoscopy in a routine colonoscopy setting: a randomized, controlled trial. GastrointestEndosc 73:1215-1222.
- Kaltenbach T, Leung C, Wu K, Yan K, Friedland S, et al. (2011) Use of the colonoscope training model with the colonoscope 3D imaging probe improved trainee colonoscopy performance: a pilot study.Dig Dis Sci 56: 1496-1502.
- Shah SG, Thomas-Gibson S, Lockett M, Brooker JC, Thapar CJ, et al. (2003) Effect of real-time magnetic endoscope imaging on the teaching and acquisition of colonoscopy skills: results from a single trainee.Endoscopy 35: 421-425.
- Coderre S, Anderson J, Rikers R, Dunckley P, Holbrook K, et al. (2010) Early use of magnetic endoscopic imaging by novice colonoscopists: improved performance without increase in workload. Can J Gastroenterol 24:727-732.
- Piscatelli N, Hyman N, Osler T (2005) Localizing colorectal cancer by colonoscopy.Arch Surg 140: 932-935.
- Ellul P, Fogden E, Simpson C, Buhagiar A, McKaig B, et al. (2011) Colonic tumour localization using an endoscope positioning device.Eur J GastroenterolHepatol 23: 488-491.
- Young JQ, Van Merrienboer J, Durning S, Ten Cate O (2014) Cognitive Load Theory: implications for medical education: AMEE Guide No. 86.Med Teach 36: 371-384.
- Carswell CM, Clarke D, Seales WB (2005) Assessing mental workload during laparoscopic surgery.SurgInnov 12: 80-90.
- Starkes J, Cullen J, Macmahon C (2004) A life-span model of the acquisition and retention of expert perceptual-motor performance. In: Williams AM, Hodges NJ, editors. Skill Acquisition in Sport: Research, Theory and Practice. London: Routledge 259-281.
- Corbett GD, Lim YC, Lee JC, Chernolesskiy A, Pugh PJ, et al. (2014) Safety of the colonoscope magnetic imaging device (ScopeGuide) in patients with implantable cardiac devices.Endoscopy 46: 135-138.
- Binggeli C, Rickli H, Ammann P, Brunckhorst C, Hufschmid U, et al. (2005) Induction ovens and electromagnetic interference: what is the risk for patients with implantable cardioverter defibrillators? J CardiovascElectrophysiol 16: 399-401.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 16557
- [From(publication date):
October-2015 - Aug 20, 2025] - Breakdown by view type
- HTML page views : 11904
- PDF downloads : 4653