Magnitude and Associated Factors of Epilepsy among HIV Seropositive Children in Public Health Facilities of Mekelle City, Tigray, Ethiopia: Institutional Based Cross-Sectional Study Design
Received: 18-Dec-2023 / Manuscript No. JPCH-23-123036 / Editor assigned: 21-Dec-2023 / PreQC No. JPCH-23-123036 (PQ) / Reviewed: 04-Jan-2024 / QC No. JPCH-23-123036 / Revised: 09-Jan-2025 / Manuscript No. JPCH-23-123036 (R) / Published Date: 16-Jan-2025
Abstract
Background: Epilepsy is a common, non-specific manifestations of neurological illnesses associated with HIV infection. With regular HIV care and management the prevalence of epilepsy could be reduced to 2%-4%, otherwise it increased to 20%. Epilepsy is associated with infections of the brain and with neurological deficits due to direct effects of the neurotropic virus and other HIV complications.
Objective: The purpose of this study was to assess the prevalence and associated factors of epilepsy among HIV seropositive children in public health facilities of Mekelle city.
Method: A facility based cross sectional study was carried out in public health facilities of Mekelle city, Tigray, North Ethiopia. Two hundred twenty two HIV infected children were recruited using systematic random sampling. Logistic regression was conducted to identify the associated factors of epilepsy. Variables with P-value<0.25 in binary logistic regression were transferred to multivariable logistic regression and variables with P-value less than 0.05 at 95% level of significance were considered as significantly associated.
Result: The study revealed that prevalence of HIV associated epilepsy was 5%, 95% CI (2.789-8.653). Most (99.1%) of the respondents were acquired the infection from their mother. Ten (90.91%) of the respondents were in WHO clinical stages of III and IV, 72.7% had CD4 count <200 cells/ml, 63.6% had HIV complication, 36.45 were not started ART, 27.3% had risk factors and 18.2% had history of epilepsy. Place of residence, rural has AOR=5.759, 95% CI (1.073-30.908), care giver sex, male has AOR=5.806 (1.006-33.51), illiterate care giver, AOR=10.183, child who live in adoption had AOR=14.981, as well as pre-epilepsy which has AOR=13.118 and having risk factors epilepsy, AOR=13.337 were the factors which increased epilepsy at p-value<0.005. On the other hand, ethnicity, religion child’s age, level of education, means of HIV transmission, care givers work and monthly income have significance association with epilepsy.
Conclusion and recommendation: The prevalence of epilepsy was more in boys than girls. CNS complications were more common among children with HIV and seizures as compared to those with HIV and no seizures. Prevention of HIV complications and strategies for the prevention of epilepsy in HIV positive individuals will be help full.
Keywords: Magnitude, Associated factor, Epilepsy, HIV seropositive children
Abbreviations
AIDS: Acquired Immune Deficiency Syndrome; ANECCA: African Network for the Care of Children Affected by HIV/AIDS; ART: Anti-retroviral Treatment; CNS: Central Nervous System; CI: Confidence Interval; DC: Data Collector; EEG: Electro Encephalo Gram; EFY : Ethiopian Fiscal year; ETB: Ethiopian Birr; FMOH: Federal Ministry of Health; GCAE: Global Campaign against Epilepsy; HIC: High-Income Countries; HIV: Human Immune Deficiency Syndrome; IBE: International Bureau for Epilepsy; ILAE: International League against Epilepsy; Kg: Kindergarten; Km: Kilometers; LAMIC: Low and Middle Income Countries; MUCHS: Mekelle University, College of Health Science; M: Meter; OI: Opportunistic Infection; PI: Principal Investigator; WHO: World Health Organization
Introduction
Epilepsy is a disorder characterized by repeated, two or more seizures of unknown immediate causes. It also defines as problem of the brain, which is characterized by an enduring tendency to generate seizures and has neurobiological, cognitive, psychological, as well as social consequences. The “definition of epilepsy requires the occurrence of at least one epileptic seizure” An individual who experience, at least one epileptic seizure of the last 2 to 5 years regardless of anti-epileptic drug treatment is classified as active epilepsy [1].
Epilepsy is a common chronic neurological problem, especially in sub-Saharan Africa, which knows no environmental, social, ethnic, sex and age preference. Approximately 50 million peoples live with epilepsy worldwide. Moreover epilepsy accounts 0.49% of the overall burden of disease to the globe.
The incidence of HIV epidemic is one of the most health problems, by which human beings have suffered from in recent history. An estimated of 3.3 million children are living with HIV worldwide; 3.1 million of them are from sub-Saharan Africa. Even though the exact prevalence of HIV in children of Ethiopia is not known, currently there are estimates of 134,586 children under 14 years live with HIV/ AIDS [2].
Epilepsy is common, non-specific manifestations of neurological illnesses associated with HIV infection, because the Central and Peripheral Nervous System (CNS/PNS) is the target site of preference for HIV. Over 50% of children develop Human Immunodeficiency Virus (HIV) associated neurological disorders at some point during the course of infection.
In the presence of regular HIV care and management the prevalence of seizures/epilepsy is reduced to 2%-4%, whereas in the absences of proper care and management the prevalence increased to 20%. Epilepsy in HIV positive children is associated with infections of the brain and with neurological deficits due to direct effects of the neurotropic virus.
The cause of seizure in HIV patient is usually unknown. However, seizure may result from brain lesions (most frequently cerebral toxoplasmosis or tuberculoma, meningitis) and metabolic disturbances.
The biomedical burden of epilepsy can be significant, but for many the social consequences might be just as extreme with epilepsy victims suffering from social rejection and economic and physical vulnerabilities.
Statements of the problem
Epilepsy is largely widespread childhood neurologic disorder, and major public health problems, which affects around 50 million people worldwide, 80% of those are from developing countries and children consist of about half of the burden. However, children and adolescents in Low and Middle Income Countries (LAMIC) constitute 35 to 50% of the population.
The prevalence of epilepsy is high in many low and middle income countries, particularly in sub-Saharan Africa, like Ethiopia. It is more than twice that of High-Income Countries (HIC).
The incidence of seizures in the HIV population varies depending on a patient’s immune status. Even though, seizure can occur at any clinical stages of the disease, it more commonly occurs in the advanced stages of HIV.
Epilepsy in HIV positive patient has a variety of underlining contributing factors. The most common causes of epilepsy in HIV positive populations are CNS opportunistic infections commonly, toxoplasmic encephalitis, followed by cryptococcal meningitis and primary CNS lymphoma, and HIV neurotoxicity. Moreover, medications used for the treatment of HIV or Opportunistic Infection (OI) and pre-existing disorders could be result in seizure or epilepsy and those neurological complications are common, even in the era of effective Anti-Retroviral Treatment (ART).
A child who diagnosed with epilepsy faces considerable challenges, especially when the seizure is poorly controlled. First and foremost, the child affects by the seizure itself or it might be disabling and interfere with the child’s ability to learn. Seizure also results with stigma and lack of knowledge about the condition can negatively affect social and psychological function.
The WHO acknowledges epilepsy among 10 leading causes of disease burden for developing countries, in 2020. Similarly, the African declaration on epilepsy acknowledges epilepsy as a healthcare priority which should be go along with the national plan of action of each country.
Throughout the past 15 years’ clarification of the diversity of epilepsy in children and the management of epilepsy is improved through, sign-symptom based and EEG diagnosis, and better etiological diagnosis, especially supported by neuroimaging. Proper control of seizures helps to improve the quality of life in these patients who are already suffering from epileptic disease. Childhood epilepsy requires integrated medical, educational, community services, and its treatment spans acute and disability medicine.
The investigators tried to review different literatures, so that, even though multiple studies done on prevalence and associated factors of epilepsy among the normal population in different parts of the world, but there are no similar published studies done on children living with HIV/AIDS, especially in resources poor countries like Ethiopia.
As the investigators level of knowledge there was lack of information on the prevalence and associated factors of epilepsy in HIV positive children in developing countries, especially in SSA. Similarly, there is no published data on prevalence and associated factor of epilepsy in HIV positive children in Ethiopia. Then the purpose of this study was to assess the prevalence of epilepsy and associated factors among HIV seropositive children in public health facility of Mekelle city [3].
Significance of the study
The magnitude and variety of neurological complications of Human Immunodeficiency Virus (HIV-1) infection in children are under described in resources poor countries like Ethiopia. There is lack of information about the prevalence of epilepsy in HIV infected children in resources poor countries, especially in sub-Saharan African countries. To the levels of the investigators knowledge no published studies were available on prevalence and associated factors of epilepsy in HIV positive children in Ethiopia, as well as in Tigray.
Psychiatric nurses and other health professionals could be used the result of this study in their day to day activities to minimize the burden and to strength the prevention and treatment practices of epilepsy in HIV seropositive children.
The finding could be provide policy makers, researchers, governmental and nongovernmental organizations as baseline data for future planning and advance related study [4].
Overviews of HIV and epilepsy
Approximately 40 million people live with HIV worldwide, about 50% of them are women and children’s and greater than 90% of children acquire the disease from their mother during conception, intrapartum or during breast milk feeding.
HIV is a neurotropic retro-virus which attacks the central nervous system by crossing the blood-brain barrier and infecting monocytes that result in neurological symptoms, which are widely prevalent and occurring at all stages of HIV infection. 50-90% of HIV-infected individuals develop symptomatic neurological disorder, in which the brain is the most commonly affected part of the nervous system especially in children [5].
Epilepsy in HIV/AIDS children may develop because of different factors: Infection of macrophages and microglia cells that nurture and maintain the brain directly by HIV infection, as a result the infected macrophages and microglia produce toxins that set off a chain reaction that kill brain cells. In addition to that AIDS-related cancers, like CNS lymphoma, brain abscess and opportunistic infections could also be affect the nervous system resulting in epilepsy.
Prevalence of epilepsy in HIV positive children
According to the WHO 2006, the prevalence of epilepsy varies by socioeconomic status, sex and age. It was higher in developing countries than industrialized countries; it was also higher in boys than girls.
Prevalence varies from country to country and even district to district within the same country largely depending on the methods used for data collection. Due to the difference in the risk factors and the programs used to control the parasitic diseases and interventions to improve antenatal and perinatal care, the prevalence also varies in sub Saharan Africa.
Although epilepsy can occur in all age groups, the highest prevalence rates are most often found in children and young people, resulting in low educational achievement and high rates of unemployment.
The prevalence rates of psychiatric disorders in HIV positive children reported in published studies vary widely from region to region, studies have shown a proportional increase in epileptic seizures as a functional decreased of CD4 counts that are the prevalence is higher in later stages of the infection.
Even though it depends on the stage of HIV/AIDS and treatment, the prevalence of neurologic involvement in HIV-infected children can be as high as 50%, usually in the first 2 years of life, due to the impact of HIV on the developing nervous system of children is more significant than on the developed adult nervous system, and certain cognitive deficits may occur in some infected youths.
The prevalence of epilepsy in HIV negative population is age dependent. The prevalence varies across the world which is from 0.5 to 5% and is higher in developing countries where, less than 50% of patients receive treatment. Whereas, people infected with Human Immunodeficiency Virus (HIV) have a higher burden of epileptic seizures and seem to have a high chance of recurrence. The prevalence of epilepsy in HIV positive individuals estimated to be 2% to 20%, with the increasing incidence of HIV infection, this could be an important cause for acute symptomatic seizures in the future.
HIV+ patients are at increased risk of developing seizures due to the vulnerability of the central nervous system to opportunistic infection and immune dysfunction. Since there is increased incidence of infections like meningitis, encephalitis and advanced stage of HIV infection, the incidence of epilepsy in the African countries is 8 times to that of in the developed countries.
A study conducted in Brazil on 340 HIV positive children to assess the HIV/AIDS associated childhood neurological symptom, indicated that the prevalence of seizure was 6 percent of the cases and 32.5% of cases were developed encephalopathy. The study was also shown that, 33.8% of the cases were manifested by CNS infections: Such as acute bacterial infections in 11%, cytomegalovirus in 6.8% and toxoplasmosis in 5.9% and cryptococcal infection in 5% [6].
Another study conducted in Spain to determine the clinical characteristics of seizure in HIV positive children indicated that the prevalence of epileptic seizure was 3%. Similar study conducted in South Korea to determine the epidemiology and clinical characteristics of seizures in patients with HIV infection shown that, the prevalence of epileptic seizure was 3%.
A facility based retrospective cross sectional study carried out in South Africa on 354 HIV infected children ages ranged from 6 months to 18 years indicated, that 95% of them were either world health organization stage 3 or 4 at presentation, and similarly this study confirmed that the prevalence of epileptic seizure was 7.6%. The study was also tried to identify the causes and out of the total 13% were had identifiable neurologic deficits and largely related to birth related brain injury, trauma and CNS infections.
A facility based cross sectional study conducted in specialized HIV/ AIDS care center in Kampala Uganda, to assess psychiatric disorder of 82 HIV positive adolescents who knew their HIV status, recognized seizure disorders in 8.4% of the patients.
Another facility based cross sectional study conducted in Sudan to describe the prevalence of epilepsy among Sudanese AIDS patients and to study the underlying causes and types of epilepsy in 700 AIDS patients estimates that 5.71% of the patients were had epilepsy and 50% of patients with epilepsy had generalized convulsion. This study was also tried to identify the cause of epilepsy, so that encephalitis was found to be the commonest cause of epilepsy followed by meningitis, brain abscess, CNS lymphoma and toxoplasmosis [7].
Risk factors of epilepsy
Symptomatic epilepsies are classified in to “remote” and “progressive” types, in which remote symptomatic epilepsies includes cases develop following insults resulting in static lesions, such as those attributable to conditions like stroke, head injury, or Central Nervous System (CNS) infections and progressive symptomatic epilepsy encompasses epilepsies associated with progressive illnesses (e.g. brain tumors or degenerative disease) [8].
Despite of the geographical variation which determines the common causes of seizure and acquired epilepsy in particular regions of the world, Central Nervous System (CNS) infections like, severe meningitis, viral encephalitis, malaria and neurocysticercosis, and most cases which are associated with increased mortality and morbidity are the main cause of seizures and acquired epilepsy in the developing world.
Etiology of seizures in HIV is multidirectional and includes HIV encephalopathy, opportunistic infections, metabolic factors and drugs.
A study conducted in 100 HIV seropositive American patients indicated that seizures were the presenting symptom of HIV-related illness in 18 patients, six of whom developed no other HIV-related illness until four months after the first seizure. Even though the common causes of seizure in the 100 patients were mass lesions, HIV encephalopathy and meningitis.
Similar study carried out on HIV seropositive children in India, confirmed opportunistic infections, like tuberculosis, cryptococcus’s and toxoplasmosis affecting the central nervous system, were the commonest underlying cause of seizures accounting for 93.9% of patients.
HIV encephalopathy has been reported in about 21% of HIV infected African children and the onset of this encephalopathy is related to the presence of other symptoms of HIV disease.
A facility based cross sectional study conducted in Sudan to assess the prevalence and underlying causes of epilepsy, identified that a new onset seizure occurred during the study period in 5% of subjects and the leading causes of seizures were drug toxicity in 47% of cases and intracranial lesions in 35%.
A community based cross sectional study conducted in Tanzania indicated that epilepsy was having association with the absent parents, that children who had one (mother or father) or no parent resident at home were more likely to have epilepsy. This study was also shown that epilepsy had strong association with family history of seizures (OR 5.7, 95% CI 1.02–27.5). Even though the study did not exclude the common environmental risk factors, it implies that genetic factors have a significant role in etiology of epilepsy.
Epilepsy is not just simply a seizure, it is more than that and it is often defined in practical terms, such as challenges, uncertainties and limitations in driving and independent living.
Epilepsy public problems which links with emotional and social effect for everyday living, such as violations and restrictions of both their civil and human rights.
Prompt management and prevention of acute seizures and the underlying CNS infection, correction of associated predisposing factors, and decisions regarding the appropriate choice and duration of antiepileptic therapy, and strategies for the prevention of epilepsy in CNS infections such as early anti-infective and anti-inflammatory therapy need scientific exploration is the only definitive way forward to reduce the burden of epilepsy in developing countries [9].
Conceptual frame works
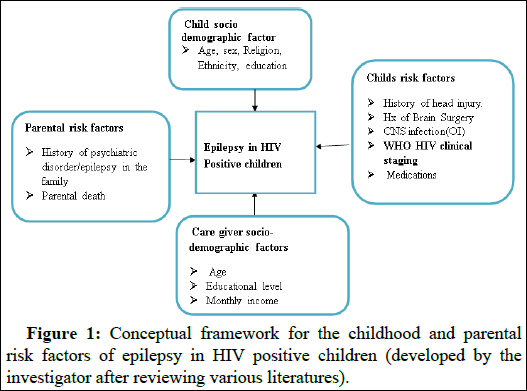
Few studies in different parts of the world reviewed that epilepsy in HIV positive children is affected by diverse factors. According to the literature review of this study the main factors were identified as care givers socio-demographic factors, parental risk factors, child socio demographic factors and risk factors. The following conceptual framework that shown, the relationship of the variables was derived from reviewing the literature of this study (Figure 1). It helps to summarize the determinant factors and to analyze the association between dependent and independent variables [10].
Figure 1: Conceptual framework for the childhood and parental risk factors of epilepsy in HIV positive children (developed by the investigator after reviewing various literatures).
Objectives
General objective: The purpose of this study was to assess the magnitude and associated factors of epilepsy among HIV seropositive children in public health facility of Mekelle city, Tigray, Ethiopia, 2020.
Specific objectives
• To determine the magnitude of epilepsy among HIV seropositive children from birth to 15 years old in public health facilities of Mekelle city, from February to May, 2020.
• To identify factors associated with epilepsy in HIV positive children from birth to 15 years old in public health facilities of Mekelle city, from February to May, 2020.
Materials and Methods
Study area and period
The study was carried out in Mekelle city, North Ethiopia, from February to May, 2018. Mekelle is located 780 km far from the capital Addis Ababa, with latitude and longitudes of 130 29’ N, 39’ E, 13.483°N and 39.457°E and at elevation of 2084 M above sea levels. The city divides in to 7 sub-cities with a total residence of 412,938, according to the 2009 EFY population estimation. Out of the total population female accounts 51.4%, male 48.6% and 60% are in the labor force. 38 percent of the total populations are children below the age of 18. The city has 3 public hospitals including Ayder referral Hospital and 10 health centers, in which, approximately there were about 700 HIV seropositive children from 0-15years old, on ART services [11].
Study design
A facility based cross sectional study was carried out in Mekelle public health facilities.
Source population: The source populations of this study were all HIV positive children who had gotten HIV care and treatment service at health facility of Mekelle city.
Study population: All sampled HIV positive 0-15 years old children, who came for Antiretroviral Therapy (ART) service or follow up during the data collection period to public health facilities of Mekelle city.
Eligibility criteria
Inclusion criteria
• HIV infected child, as witnessed by rapid test or other diagnostic procedures and clearly documented on the HIV/AIDS registration book was included in the study.
• A child who was enrolled at the hospital or clinic and who had at least two documented visits was included in the study.
• 0-8 years old children with their care givers and above 8-years old who came on the data collection period was included in the study.
Exclusion criteria
• 0-8 years’ old child’s, who came alone during the data collection period.
• Child who had incomplete record document was not included in the study.
Sample size calculation and sampling procedure
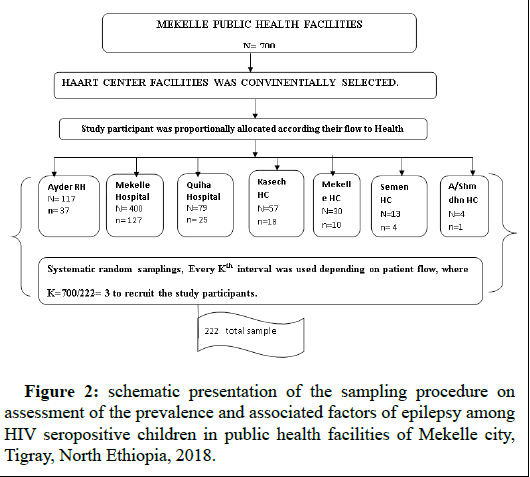
Sample size calculation: Calculation of the sample size was carried out using computer software Epi info version 7, by considering, 95% confidence level and prevalence of 7.6% taken from similar study conducted in South Africa. 3% of marginal error was used, to increase the sample size. By using the correction formula and adding 5% non-response rate the total sample size for this study was calculated to be 222 [12].
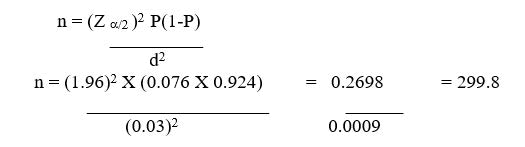
Since the total population was less than 10,000, so that correction formula was used.
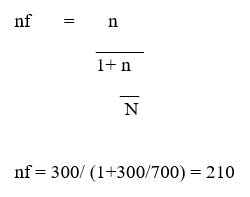
By adding 5% non-response rate the total sample size was calculated to be 222.
Where:
Z α/2=95 % confidence interval=1.96
P=Prevalence of epilepsy=0.076
N=Total population
n=required sample size
nf=corrected sample size
d=marginal error=0.003
Sampling procedure: All ART center public health facilities were selected for the study. Concerning on the flow of participants or their respective registration, systematic random sampling was used in determining the sampling interval (K), where, K=700/222=3. After selecting the random start number (a number between 1 and 3) by simple random sampling, every 3rd interval study participants were, recruited for the study until the sampling saturation was reached. Study subjects were allocated proportionally to the patient flow in the selected health facilities (Figure 2). The study were follow two phases; the first phase was conducted for assessing the prevalence of epilepsy, then after those with epilepsy again recruited for identifying the risk factors of epilepsy using semi structured interviews [13].
Figure 2: schematic presentation of the sampling procedure on assessment of the prevalence and associated factors of epilepsy among HIV seropositive children in public health facilities of Mekelle city, Tigray, North Ethiopia, 2018.
Data collection material and procedures
Interview using semi structured questionnaire was used to obtain data from the study participants. The questionnaire was primarily adopted from different literatures by the principal investigators and was translated to local language (Tigrigna) to be understood by all participants as well as the data collectors and then translated back to English by expertise.
Six data collectors, who had experience in data collection, was train for one day, prior to actual data collection. They were familiarizing with the questionnaire to be administered in the field; any un-clarity in the questionnaire was reach in consensus.
To avoid double recruitments, a list of participants’ code and their identification numbers was used to cross-check the participants before they were interviewed. The client’s corresponding file also was reviewed to obtain participants WHO, HIV clinical staging and additional available information needed for the study [14].
Variables of the study
Dependent variable: Epilepsy in HIV seropositive children.
Independent variable:
• Childs socio demographic character (age, sex, religion, ethnicity, level of education and means of HIV transmission).
• Care givers socio-demographic and economic states (age, sex, educational status, occupation and monthly income)
• Family type/care giver relation with the child (biologic, non biological, adoptive/foster).
• Child risk factors of epilepsy: Age at the starting of seizure, WHO clinical stage, CD4 level; history of head injury before, during and after birth; history of OI; CNS infections.
• Parental risk factors of epilepsy: History of psychiatric disorder/ epilepsy in the family; parental death.
Operational definitions
Epilepsy: The definition of epilepsy requires the occurrence of at least one epileptic seizure of any causes and an epileptic seizure was also defined as “a transient occurrence of signs and/or symptoms due to abnormal excessive or synchronous neuronal activity in the brain”.
A case of active epilepsy refers to a person who is either currently being treated for epilepsy or whose most recent seizure has occurred (usually) within the past 2-5 years.
HIV related epilepsy: When patients had experienced at least one episodes of seizure of any cause after HIV infection, referred to HIV related epilepsy.
Data quality assurance
Pre-testing of the questionnaire was carried out in 5% of the sample size, one week prior to the actual data collection, in public health facilities of Wukro Town, in eligible children. This was carried out to test the data collection tools, to approximate the time used to fill the questionnaire and to assess the field procedure. The difficulty and ambiguity of the questionnaire were restructured and the final version of the questionnaire was used for the data collection.
Data quality assurance was in place since questionnaire designing, data collection and data entry. Coded data obtained from the questionnaires used during the structured interviews by the data collectors were submitted to the principal investigator on daily basis and checked for any incompleteness and/or inconsistency. Daily debrief meeting between the principal investigator and the data collectors were conducted to clarify any necessary and relevant issues.
Data management and analysis
Data was entered on daily basis, checked, cleaned and analyzed using the computer software program Epi info version 7, then, transferred to statistical package for social science (SPSS-20) version 20 for analysis. Descriptive statistics, frequencies, tables, percentages, means and standard deviation, were used for the sociodemographic and clinical variables, including individual’s response. Binary logistic regression and odds ratio with 95% confidence interval was used to identify the independently associated factors with Epilepsy. Variables with P-value less than 0.25 in binary logistic regression were analyzed using multivariate logistic regression and variables with P-value less than 0.05 were considered as significantly associated [15].
Ethical considerations
The study was carried out after getting ethical clearance from institutional review boards of Mekelle University, College of Health Science (MUCHS). Supportive letter was written from Mekelle University College of health science to Tigray Regional health bureau and from Tigray Regional health bureau to respective health facilities to collect the data.
A written informed consent or verbal child assent was obtained from the study participants, by considering the purpose of the study, details of what will happen if they participated or otherwise in the study. It was also explained that participation in the study was voluntary and had no consequences on the child’s right and benefits. In addition, it was made clear that participants were free not to answer any question they were uncomfortable with. A contact detail of the principal investigator was available to the participants. Confidentiality was also guarantee and the questionnaire was coded by numbers to ensure that the participants remained acronyms.
Dissemination of the result
The study result will be submitted to Mekelle University, College of Health Science in partial fulfillment of the requirement for masters of degree in nursing. It will also be disseminated to respective public health facilities, Tigray health bureau and to FMOH. Effort also, will be made to present the study in scientific conferences and finally the finding will be published in peer-reviewed journals.
Results
Socio-demographic characteristics
In this study 222 HIV positive children were included by making 100% response rate. The mean (± SD) age of 10.41 ± 3.35 ranges from 9.97-10.85 years. One hundred thirty two (59.5%) were females’. However 150 (64.86%) respondents were from urban areas. Two hundred (90.1%) were Orthodox Christian followers. Two hundred nineteen (99.1%) children were acquired the infection from their mothers and one hundred fifty-two (68.5%) live with their biological parents (Table 1) [16].
| Variables | Categories | Frequency (N=222) | Percent | Total % |
| Age of the child | 0-4 | 11 (f=8, m=3) | 15.3% | 100% |
| 5-9 | 72 (f=32, m=40) | 29.7% | ||
| 10-15 | 139 (f=92, m=47) | 55% | ||
| Childs sex | Female | 132 | 59.5% | 100% |
| Male | 90 | 40.5% | ||
| Place of residence | Rural | 72 (f=39, m=33) | 32.4% | 100% |
| Urban | 150 (f=93, m=57) | 67.6% | ||
| Ethnicity | Tigray | 213 (f=126, m=87) | 95.9% | 100% |
| Others | 9 (f=6, m=3) | 4.1% | ||
| Religion | Orthodox | 200 (f=115, m=85) | 91.1% | 100% |
| Muslim | 14 (f=11, m=3) | 6.3% | ||
| Protestant | 8 (f=6, m=2) | 3.6% | ||
| Child level of education | Not started | 24 (f=11, m=13) | 10.8% | 100% |
| KG to grade one | 35 (f=20, m=15) | 15.8% | ||
| Grade two to grade four | 60 (f=29, m=31) | 27% | ||
| Grade five to grade eight | 87 (f=63, m=24) | 39.2% | ||
| Grade nine and above | 16 (f=9, m=7) | 7.2% | ||
| Means of HIV transmission | From mother | 220 (f=131,m=90) | 99.5% | 100% |
| Sharp material | 1 (f=0, m=2) | 0.5% | ||
| Sexual intercourse | 1 (f=1, m=0) | 0.5% | ||
| Child relation with care giver | Biological parent | 152 (f=93, m=59) | 81.5% | 100% |
| Relative | 45 (f=23, m=22) | 14% | ||
| Adoption | 25 (f=16, m=9) | 4.1% | ||
| Parental status of living | Both parent alive | 116 (f=68, m=48) | 52.3% | 100% |
| Only father alive | 30 (f=11, m=19) | 13.5% | ||
| Only mother alive | 37 (f=30, m=7) | 16.70% | ||
| Both parent dead | 39 (f=23, m=16) | 17.60% | ||
| Care givers age category | 25-40 | 148 (f=90, m=58) | 66.7% | 100% |
| 41-56 | 70 (f=40, m=30) | 31.5% | ||
| ≥ 57 | 4 (f=2, m=2) | 1.8% | ||
| Care givers sex | Female | 180 | 81.1% | 100% |
| Male | 42 | 18.9% | ||
| Care giver level of education | No formal education | 27 | 12.2% | 100% |
| Primary | 18 | 8.1% | ||
| Secondary | 91 | 41% | ||
| College and above | 86 | 38.7% | ||
| Care giver/parents work | Governmental employee | 36 | 16.2% | 100% |
| Self-employee | 71 | 32% | ||
| Housewife | 61 | 27.5% 11.7% | ||
| Merchant | 26 | 12.6% | ||
| Others* | 28 | |||
| Note: Others*: Commercial sex worker, daily laborer; Others: Amhara and Afar | ||||
Table 1: Distribution of socio demographic characteristics of HIV positive children and their care giver attending public health facilities of Mekelle city, North Ethiopia 2018.
Prevalence of epilepsy among HIV seropositive children
The study found that the prevalence of HIV associated epilepsy was about 5% 95% C.I (2.789-8.653). The mean (± SD) ages of the participants who had epilepsy were 9.82.78 ± 3.995, ranges from 7.13-12.50. Seven (63.64%) of the respondents were rural residents and majority of the respondents 8 (72.73%) who were had the cases were orthodox in religion Ten (90.91%) of the respondents were in WHO clinical stages of 3 and 4, 72.7% were had CD4 count <200 cells/ml, 63.6% had HIV complication, 36.45 not started ART, 27.3 5 risk factors and 18.2% were had history of epilepsy before HIV infected (Table 2) [17].
| Variable | Categories | Frequency (N=222) | Frequency of epilepsy cases (n=11) |
| Did your child ever have history of epilepsy? | No (f=128, m=84) | 212 (95.5%) | 9 (81.8%) |
| Yes (f=4, m=6) | 10 (4.5%) | 2 (18.2%) | |
| Did your child have history of falling, abnormal shaking after HIV infected (Dx of epilepsy)? | No (f=129, m=82) | 211 (95%) | 0 (0%) |
| Yes (f=3, m=8) | 11 (5%) | 11 (4.95%) | |
| Risk factors of epilepsy | No (f=129, m=82) | 211 (95%) | 8 (72.7%) |
| Yes (f=3, m=8) | 11 (5%) | 3 (27.3%) | |
| Positive family history | No (f1=30, m=84) | 215 (96.8%) | 9 (81.8%) |
| Yes (f=2, m=6) | 7 (3.2%) | 2 (18.2%) | |
| Head trauma | No (f=30, m=84) | 214 (96.4%) | 8 (91.9%) |
| Yes (f2=, m=6) | 8 (3.6%) | 3 (9.1%) | |
| What was the WHO clinical staging at the time of first seizure? | Stage-II (f=1, m=0) | 1 (0.5%) | 1 (9.1%) |
| Stage III (f=0, m=3) | 3 (1.4%) | 3 (27.3%) | |
| Stage IV (f=2, m=5) | 7 (3.2%) | 7 (63.6%) | |
| NA (f=129, m=82) | 211 (95%) | ||
| CD4 count at 1st seizure | <200 (f=2, m=6) | 8 (3.6%) | 8 (72.7%) |
| >200 (f=1, m=2) | 3 (1.4%) | 3 (27.3%) | |
| NA (f=129, m=82) | 211 (95%) | ||
| Did the child was started ART at the time of first seizure? | No (f=2, m=1) | 3 (1.4%) | 3 (1.4%) |
| Yes (f=1, m=7) | 8 (4.1%) | 8 (4.1%) | |
| NA (f=129, m=82) | 211 (95%) | ||
| Did your child have CNS complications at the time of first seizure? | No (f=2 and m=2) | 4 (1.8%) | 4 (36.4%) |
| Yes (f=1 and m=6) | 7 (3.2%) | 7 (63.6%) | |
| NA (f=129, m=82) | 211 (95%) | ||
| Encephalopathy | No | 3 (1.4%) | 3 (27.3%) |
| Yes | 3 (1.4%) | 3 (27.3%) | |
| NA | 216 (97.3%) | 4 (36.4%) | |
| Toxoplasmosis | No | 3 (1.4%) | 3 (27.3%) |
| Yes | 3 (1.4%) | 3 (27.3%) | |
| NA | 216 (97.3%) | 5 (45.5%) | |
| CNS tuberculosis | No | 5 (2.3%) | 5 (45.5%) |
| Yes | 1 (0.5%) | 1 (9.1%) | |
| NA | 216 (97.3%) | 5 (45.5%) | |
| Brain lesion/mass | No | 5 (2.3%) | 5 (45.5%) |
| Yes | 1 (0.5%) | 1 (9.1%) | |
| NA | 216 (97.3%) | 5 (45.5%) | |
| Others | No | 5 (2.3%) | 5 (45.5%) |
| Yes | 1 (0.5%) | 1 (9.1%) | |
| NA | 216 (97.3%) | 5 (45.5%) |
Table 2: Prevalence of epilepsy, in HIV seropositive children in public health facilities of Mekelle city, Tigray, Ethiopia, 2018.
Associated/Risk Factors of Epilepsy
As shown in the multi variable analysis below, fourteen of the 22 variables did not show significant association with epilepsy in HIV seropositive children at 5% level of significance. Of these respondents’ age, religion, ethnicity, child level of education and means of as well as parental age, work and monthly income were not significant at 0.25 level of significance and were excluded from multivariable analysis. After checking the multi colinearity, multivariable logistic regression was done using the backward conditional method of regression by considering 8 variables in to account simultaneously.
The majority of variables which were shown significant association with epilepsy in bivariate logistic regression analysis were also persevered as significant in the multivariable analysis. These covariates were, place of residence, child relation with the care givers/parental living status, care givers sex, care givers level of education, pre epilepsy and Risk factors of epilepsy, were shown overall significant association with epilepsy at 5% level of significance and P-value <0.05.
The result of the study noted that, the odds of being rural inhabitant and HIV positive were 5.759 times higher, in having epilepsy than of child who live in urban area and HIV positive at P-value 0.041 and (AOR=5.759, 95% CI (1.073-30.908)).
Similarly the finding of the study acknowledged that, parental status of alivement or child’s relation with his/her care givers was shown significantly association with the developing of epilepsy in HIV positive children, a child who live with his/her biological parents were lower odds than a child who live with relative or in adoption (AOR=0.067, 95% CI (0.008-0.529) and P=0.010) and a child who live in adoption had higher odds in developing epilepsy at p value<0.010 and AOR=14.981, 95% CI (1.891-118.7).
The finding of the study also, revealed that history of Epilepsy shown a statistical significant relation with HIV associated epilepsy (p-value=0.014). The study indicated that, children who had pre epilepsy had 13.118 times higher odds of developing epilepsy compared to those children who did not have pre-epilepsy. In addition to that the result of the study recognized that, the odds of child having risk factors of epilepsy other than HIV was 13.337 times more associated with the developments of epilepsy than those without the risk factors (Table 3) [18].
| Variables | Frequency | COR (95% CI) | AOR (95% CI) | P-value | |
| Childs sex | Female | 132 (59.5%) | 0.238 (0.061-0.925)* | 0.038 | |
| Male | 90 (40.5%) | 4.195 (1.082-16.271)* | |||
| Residence | Rural | 72 (32.4%) | 3.931 (1.112-13.896)* | 5.759 (1.073-30.908) | 0.041 |
| Urban | 150 (67.6% | 0.254 (0.072-0.899)* | 0.173 (0.032-0.932) | ||
| Child relation with the care giver | Biological | 152 (68.5%) | 0.198 (0.042-0.946)* | 0.067 (0.008-0.529) | 0.01 |
| Relative | 45 (20.3%) | 3.610 (0.865-15.060) | 0.185 (0.019-1.759)+ | ||
| Adoption | 25 (11.3%) | 5.045 (1.058-24.071) * | 14.98 (1.891-118.7) | 0.01 | |
| Care givers sex | Female | 180 (81.1%) | 0.255 (0.074-0.881)* | 0.172 (0.030-0.994) | 0.05 |
| Male | 42 (18.9%) | 3.919 (1.136-13.525)* | 5.81 (1.006-33.510) | ||
| Care givers level of education | No formal education | 27 (12.2%) | 9.545 (1.734-52.549)* | 10.183 (1.395-74.334) | 0.022 |
| Primary | 18 (8.1%) | 8.4 (1.293-54.591) | 10.642 (1.195-94.801) | 0.034 | |
| Secondary | 91 (41%) | 0.049 (0.005-0.440) | 0.022 (0.002-0.318) | 0.005 | |
| ≥ College | 86 (38.7%) | 0.105 (0.019-0.577)* | 0.098 (0.013-0.717) | 0.022 | |
| History of epilepsy | No | 212 (95.5%) | 0.177 (0.033-0.985)* | 0.076 (0.010-0.598) | 0.014 |
| Yes | 10 (4.5%) | 5.639 (1.043-30.475)* | 13.118 (1.672-102.90) | ||
| Risk factors | No | 211 (95%) | 0.105 (0.023-0.473)* | 0.075 (0.008-0.662) | 0.02 |
| Yes | 11 (5%) | 9.516 (2.116-42.785)* | 13.337 (1.512-117.675) | ||
| Positive family Hx | No | 215 (96.8%) | 0.109 (0.019-0.642)* | 0.080 (0.008-0.847) | 0.036 |
| Yes | 7 (3.2%) | 9.156[1.559-53.775]* | 12.432 (1.181-130.904) | ||
| Head trauma | No | 214 (96.4%) | 0.065 (0.013-0.319)* | 0.054 (0.006-0.514) | |
| Yes | 8 (3.6%) | 15.45 (3.131-76.228)* | 18.572 (1.945-177.339) | ||
| Note:*p value <0.05 in bivariate analysis and +p value>0.05 | |||||
Table 3: Bivariate and multivariable logistic regression analysis result for significant variables (p ≤ 0.25) in bivariate analysis in Mekelle city public health facilities, North Ethiopia, 2018.
Discussion
This study was intended to assess the prevalence and associated factors of epilepsy among HIV positive children, for the purposes of knowing, as well as challenging the burden and associated factors of epilepsy in HIV positive children [19].
Out of the total 222 study participants, incorporated in the study, 11 (5%), children, were epilepsy, in 95% C.I, ranges from (2.789%-8.653%). Of them 3 (27.3%) female and 8 (72.7%) male children were found to be with epilepsy, even though there was age difference in the respondents, this result was consistent with the study conducted earlier in Sudan, this consistency might be due to similarity in study design and study area.
The prevalence of epilepsy was found higher in boys than girls (AOR=4.195, 95%, C.I, (1.082-16.271) and P-value=0.026) this result is in consistent with the result published previously by WHO.
The finding of the study was indicated that, 90.9% of the respondents, who were having epilepsy were either in the WHO clinical stage of 3 or 4, this is more or less comparable with the study which was conducted previously in South Africa, this similarity might be happen due to similarity in study design and study populations.
HIV associated encephalopathy was described in About 27.3% of children who were had epilepsy, the result was to some extent higher than the study conducted before, by the African Network for the Care of Children Affected by HIV/AIDS (ANECCA) which was 21%, this result of inconsistency might be due to the sample size difference and methods which was systemic review used in the first study.
The prevalence of epilepsy found in this study was higher than of the study conducted before in Spain and South Korea which was 3%, this difference might be happen due to age difference, higher risk factors in this study (n=5) and advanced technologies in the rest one.
The result of the study was lower than, the result of the study conducted earlier in Brazil which was 6%, in addition to that 45.45%of respondents of this study were developed CNS complication where, encephalopathy occurs in 27.3%, this is comparable with the study conducted earlier in cape town, toxoplasmosis in 27.3%, and 9.1%were developed cerebral Tuberculosis. Whereas in the previous study CNS complications were developed in33.8% study participants, of them 32.5% of cases were developed encephalopathy, 11% acute bacterial infections and toxoplasmosis was developed in 5.9% of the study participants.
The finding of the study was also lower than the study which was conducted previously in Kenya, Kilifi district, that nine hundred (18.3%) out of the 4,921 were had seizure/epilepsy, this difference might be occur due to early initiation of ART in this study and difference in sample size and study design.
The prevalence of epilepsy found in this study was inconsistent with the result of the study, conducted before in Cape Town, which was 11%, this discrepancy may occur due to study area and sample size difference that is the study setting in the previous study was in patient department.
The prevalence of epilepsy in this study, differ from the result of the study which was conducted formerly in South Africa which was 7.6%. This discrepancy might be due to sample size difference and early initiation of ART in this study.
The finding of this study was distinguished that epilepsy and place of residency were had significant association at 95% C.I and p-value, 0.041 and (AOR, 5.759 (1.073-30.908)), which explained that a child with HIV and rural resident has 5.759 times higher chance of epilepsy than a child who live in urban area and HIV seropositive. This result was consistent with the result of the study which was conducted previously in Turkey.
However, this study also revealed that epilepsy in HIV seropositive child has significant association with the child care giver level of education at p-value of 0.021 (AOR=9.545, 5%, C.I (1.734-52.549)), means that HIV seropositive child, who have illiterate care givers has higher probability of having epilepsy than a seropositive child and whose care giver were with educational levels of college and above.
The result of the study was noted that epilepsy has association with the child’s relationship with his/her care givers (absent parents), in which children who live with biological parent (mother or father) were less likely to have epilepsy, than a child who lives in relative and adoption (AOR=0.067 95%, C.I. (0.008-0.529)) on the other hand a child who live in adoption has higher chance of developing epilepsy than the child who live with their biological parents (AOR=14.981, 95%, C.I. (1.891-118.7)) and p value 0.010. Beside of this he result of the study was also acknowledged that, epilepsy has strong significant association with the positive family history of seizure this is similar with the community based cross sectional study previously conducted in Tanzania (AOR 5.7, 95% CI 1.02–27.5). This result of family history of epilepsy was also consistence with the case control study conducted before in Cambodia.
The finding of this study was displayed that epilepsy had strong significant association with history of head trauma at p-value 0.011, (AOR=18.572 (95% C.I=1.945-177.339)). This finding is in congruent with the result of the study which was carried out before in Iran and South Africa, this might be occur due to similar population used in both studies.
Although HIV associated CNS complications were had not significant association with the risk of epilepsy, because of it did not analyzed with logistic regression and odds ratio, majority of the respondents were had CNS complications, this result is more or less comparable with the finding of the study which was previously conducted in Iran and South Africa, this similarity may be due to use of similar study design and study participants.
The result of the study also exposed that history of pre-existing epilepsy before HIV infection was significantly related with HIV associated epilepsy. These children who were had pre-existing epilepsy have 13.118 times high probabilities of having HIV associated epilepsy than those children without pre-existing epilepsy. Even though the age group of the respondent were had difference, this result is in consistent with the study conducted before in Korea.
This study indicated that one (9.1%) the respondent’s causes of epilepsy was idiopathic or HIV itself means that the child had no risk factors or HIV associated complications, this result is consistent with the retrospective study carried out previously in New York city.
Even though it was not significant at 95% level of significant, the study revealed that, Ten (90.91%) of the respondents were in WHO clinical stages of III and IV, 72.7% were had CD4 count<200 cells/dl, 36.45 not started ART, 27.3 5 risk factors, 18.2% were had history of epilepsy before HIV infected and 63.6% had HIV complication. Of them 3 were had brain encephalopathy, 3 toxoplasmosis, 1 cerebral tuberculosis, as well as 1 child was had brain lesion.
The finding of this study revealed that means of HIV transmission was not significantly associated with epilepsy that is p>0.05 this result is inconsistency with the result of the systemic review which was conducted previously in Germany, this inconsistency might be due to the participants age difference and the method used, which was systemic review in the previous one [20].
Strength of the study
• Prior training of data collectors, regular supervision by the principal investigator and using pretested data collection tool.
• The study was used both primary and secondary data type.
• High response rate to survey interviews.
Limitation of the study
• Since this study was cross sectional and quantitative types of study it does not confirm definitive cause and effect relationship. Therefore it was better if prospective qualitative approach and other methods were also engaged to reconnoitre additional associated factors.
• This study was done in the public health facilities, thus results might not be generalizable to the entire population in the catchment area.
• The study was done in limited areas of public health facilities; it was better to expand and included both at facility and community levels.
Conclusion
The prevalence of Epilepsy among HIV seropositive children was found to be 5%. This study has also observed that the prevalence of epilepsy was higher in boys than girls. Similarly the prevalence was higher in rural than urban residence. It was revealed that, place of residence, child relation with the care giver, care givers sex and level of education, as well as previous history of epilepsy and risk factors of Epilepsy other than HIV/AIDS were the factors that had association with epilepsy in HIV infected children.
Age, religion, ethnicity level of educations of the child, care givers age, job and monthly income were not found to be statistically associated of epilepsy. CNS complications were more common among children with the advanced stages of HIV/AIDS and seizures. Therefore the finding in this study support a need for caution and regular monitoring of antiretroviral agents and use of antiepileptic drug, concurrently for optimal seizure control.
Recommendations
Based on the results of the study the following recommendations are forwarded.
For government and policy makers: It would be better if they provide special attention and they incorporate epilepsy in HIV positive individual to the health care plan.
For the regional health bureau
• Prevention of HIV associated CNS infections and strategies for the prevention of epilepsy in HIV positive individuals such as early detection and treatment of OI.
• Strategies for prevention and treatment of epilepsy in HIV positive children will be help full.
For health care providers
• Health care providers especially these works on ART service should be aware of seizure in HIV positive individuals and should be properly managed epilepsy and other HIV associated CNS complications.
• Early detection and effective control of opportunistic infection would be helpful for prevention of epilepsy in HIV positive children.
For researchers: Caring out further prospective study should be important, to know better the significantly associated factors of epilepsy, among HIV infected individuals.
Data Availability
The data used to support the findings of this study are included in the article
Ethical Approval and Consent to Participate
Before starting the data collection process, ethical clearance was given from Aksum University Health Bureau ethical clearance committee to each selected hospital. Informed, written and signed consent was obtained from each head of every facility involved in the study and participant mothers after the purpose and benefits of the study are discussed. Participants were informed about the minimal risk that it had taking part in the study, their volunteerism and the right to leave the interview at any time they want. Confidentiality of the study participant’s information was also kept secure.
Funding
There is no funding for this research. All costs of data collection and analysis were covered by the authors.
Competing Interests
This manuscript maintains no competing financial interest declaration from any person or organization, or non-financial competing interests such as political, personal, religious, ideological, academic, intellectual, commercial or any other.
Authors’ Contributions
GK: Conceived and designed the study, analyzed the data and wrote the manuscript. HG: Involved in data analysis, drafting of the manuscript and advising the whole research paper and also were involved in the interpretation of the data and contributed to manuscript preparation. Similarly, all authors have read and approved the final version of the manuscript.
Acknowledgments
I would like to thank Aksum University, Tigray Region Health Bureau and respected hospitals health centers, study participants and data collectors for their contribution in the success of our work.
References
- Boisse L, Gill MJ, Power C (2008) HIV infection of the central nervous system: clinical features and neuropathogenesis. Neurol Clin 26: 799-819.
[Crossref] [Google Scholar] [PubMed]
- Kellinghaus C, Engbring C, Kovac S, Möddel G, Boesebeck F, et al. (2008) Frequency of seizures and epilepsy in neurological HIV-infected patients. Seizure 17: 27-33.
[Crossref] [Google Scholar] [PubMed]
- Debrock C, Preux PM, Houinato D, Druet-Cabanac M, Kassa F, et al. (2000) Estimation of the prevalence of epilepsy in the Benin region of Zinvié using the capture-recapture method. Int J Epidemiol 29: 330-335.
[Crossref] [Google Scholar] [PubMed]
- Santhosh NS, Sinha S, Satishchandra P (2014) Epilepsy: indian perspective. Ann Indian Acad Neurol 17: S3-S11.
[Crossref] [Google Scholar] [PubMed]
- World Health Organization (2006) Neurological disorders: public health challenges. World Health Organization.
- Thurman DJ, Beghi E, Begley CE, Berg AT, Buchhalter JR, et al. (2011) Standards for epidemiologic studies and surveillance of epilepsy. Epilepsia 52: 2-6.
[Crossref] [Google Scholar] [PubMed]
- Mamadou Z (2017) Peculiarities of Epileptic Seizures in Patients Living with HIV Infection a Review of the Literature. SF J Neuro Sci1 1.
- Lotfalinezhad E (2016) A short perspective on the risk profile of epilepsy in Iran. MJN 1: 1-3.
- Birbeck GL (2012) Working Together to Improve the Lives of People Affected by Epilepsy in Zambia. J High Educ Outreach Engagem 16: 175-184.
- Haileamlak A, Hagos T, Abebe W, Abraham L, Asefa H, et al. (2017) Predictors of Hospitalization among Children on ART in Ethiopia: a Cohort study. Ethiop J Health Sci 27: 53-62.
[Crossref] [Google Scholar] [PubMed]
- Mbonda PC, Kuate C, Njamnshi AK, Fogang Y, Fonsah J, et al. (2013) Etiologic aspects of epileptic seizures of recent onset in HIV-AIDS infected subjects at the Yaounde Central Hospital (Cameroon). World J AIDS. 3: 160-167.
- Tindyebwa D, Kayita J, Musoke P, Eley B, Nduati R, et al. (2004) Handbook on Paediatric AIDS in Africa by the African Network for the Care of Children Affected by AIDS.
- Kayita J, Musoke P, Eley B, Nduati R, Coovadia H, et al. (2004) Handbook on paediatric AIDS in Africa. Tindyebwa D, editor. Kampala: African Network for the care of children affected by AIDS.
- Power C, Boissé L, Rourke S, Gill MJ (2009) NeuroAIDS: an evolving epidemic. Can J Neurol Sci 36: 285-295.
[Crossref] [Google Scholar] [PubMed]
- Govender R, Eley B, Walker K, Petersen R, Wilmshurst JM (2011) Neurologic and neurobehavioral sequelae in children with human immunodeficiency virus (HIV-1) infection. J Child Neurol 26: 1355-1364.
[Crossref] [Google Scholar] [PubMed]
- Angelini L, Zibordi F, Triulzi F, Cinque P, Giudici B, et al. (2000) Age-dependent neurologic manifestations of HIV infection in childhood. Neurol Sci 21: 135-142.
[Crossref] [Google Scholar] [PubMed]
- Garg RK (1999) HIV infection and seizures. Postgrad Med J 75: 387-390.
[Crossref] [Google Scholar] [PubMed]
- Yemadje LP, Houinato D, Quet F, Druet‐Cabanac M, Preux PM (2011) Understanding the differences in prevalence of epilepsy in tropical regions. Epilepsia 52: 1376-1381.
[Crossref] [Google Scholar] [PubMed]
- Singhi P (2011) Infectious causes of seizures and epilepsy in the developing world. Dev Med Child Neurol 53: 600-609.
[Crossref] [Google Scholar] [PubMed]
- Mbuba CK, Ngugi AK, Newton CR, Carter JA (2008) The epilepsy treatment gap in developing countries: a systematic review of the magnitude, causes, and intervention strategies. Epilepsia 49: 1491-1503.
[Crossref] [Google Scholar] [PubMed]
Citation: Kidanemariam G, Gebrekidan H (2025) Magnitude and Associated Factors of Epilepsy among HIV Seropositive Children in Public Health Facilities of Mekelle City, Tigray, Ethiopia: Institutional Based Cross-Sectional Study Design. J Preg Child Health 11: 676.
Copyright: © 2025 Kidanemariam G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 381
- [From(publication date): 0-0 - Nov 21, 2025]
- Breakdown by view type
- HTML page views: 273
- PDF downloads: 108