Magnitude and Associated Factors of Neonatal Near Miss among Neonates Delivered at Alert Comprehensive Specialized Hospital, Addis Ababa, Ethiopia, 2022: A Cross Sectional Study
Received: 22-Feb-2023 / Manuscript No. JPCH-23-89896 / Editor assigned: 24-Feb-2023 / PreQC No. JPCH-23-89896 (PQ) / Reviewed: 10-Mar-2023 / QC No. JPCH-23-89896 / Revised: 05-May-2023 / Manuscript No. JPCH-23-89896 (R) / Published Date: 12-May-2023
Abstract
Background: Neonatal “near misses” are newborns with severe complications at birth or during the neonatal phase who survived. It is critical to identify neonatal “near miss” cases and correct contributing factors. To ascertain the magnitude and associated factors of neonatal near misses among neonates delivered at alert’s comprehensive and specialized hospitals.
Materials and Methods: An institution based cross sectional study was conducted among 377 neonates who were delivered from March to April 2022. A face to face interviewer administered a structured questionnaire that was supplemented with checklists from maternal and neonatal medical records. The collected data was entered into Epi- Data version 4.6 and analyzed with statistical package for social sciences version 26.0. Using binary logistic regression, bivariable and multivariable analyses were performed to identify factors associated with neonatal near misses and a P-value of 0.05 at a 95% confidence interval was declared statistically significant.
Results: The overall magnitude of the neonatal near miss was 30.7% (95% CI: 26.3–35.7). Having a monthly income below the poverty line (AOR: 2.88, 95% CI: 1.37, 6.06), a previous history of neonatal death (AOR: 13.5, 95% CI: 6.67, 27.48), a cesarean section delivery (AOR: 2.56, 95% CI: 1.30, 5.06) and not taking iron with folic acid during pregnancy (AOR: 3.32, 95% CI: 1.58, 6.97) were statistically associated with a neonatal near miss.
Conclusion: The magnitude of the neonatal near misses was high. It was associated with low monthly income, a previous history of neonatal death, cesarean section deliveries and not taking iron with folic acid during pregnancy.
Keywords:
Keywords
Neonatal; Near miss; Magnitude; Alert hospital; Ethiopia
Introduction
The neonatal period is defined as the period from the birth of the newborn to 28 days of life postpartum. This period was highly important for the survival of the new born and that left them highly vulnerable to death [1]. The neonatal period lasts from birth to the first 28 days and is divided into three stages: Very early (first 24 hours), early (24 hours to 7 days) and late neonatal period (7 days to 28 days) [2].
The mortality of neonates in low and middle income countries carries an excessive risk of death and accounts for three quarters of neonatal deaths [3,4]. Less than 1% of these deaths occur in developed countries, while 98% of all neonatal deaths occur in developing countries and Sub-Saharan African countries hold the highest burden of neonatal near misses and deaths [5].
In Sub-Saharan Africa (SSA), the neonatal mortality rate was 28 deaths per 1,000 live births and a child born in this region is 10 times more likely to die in the first month than a child born in a high income country [6]. Of the neonatal deaths in the SSA, 50% occurred in just five countries: Ethiopia, Nigeria, the DR Congo, Tanzania and Uganda. Until now, there has been no standard definition for the identification of the criteria for Neonatal Near Miss (NNM) cases. The development of criteria to identify Neonatal Near Miss (NNM) cases is challenged by the absence of a gold standard definition for near miss cases, but the maternal near miss definition that was undertaken in 2009 enhanced the establishment of understanding for the development of definitions and criteria for NNM [7].
CLAP recommends pragmatic criteria such as birth weight of less than 1750 g, Apgar score of less than 7 at 5 minutes of life and gestational age of less than 33 weeks. Management criteria include nasal continuous positive airway pressure, any intubation during the first 27 days of life, parenteral therapeutic antibiotics (up to 7 days and before 28 days of life), phototherapy within the first 24 hours of life, the use of vasoactive drugs, anticonvulsants, surfactants, blood products and steroids for refractory hypoglycemia, cardiopulmonary resuscitation and any surgical procedure. They also proposed some management criteria that had not previously been considered, such as the use of antenatal steroids, parenteral nutrition and congenital malformations [8].
In addition to this, in Ethiopia, attempts were made to assess the magnitude of neonatal mortality. In 2016, about 87,000 neonates died each year within the first 28 days of life after birth and the rate of mortality was among the highest in the world [9]. The trend of mortalities also increased from 29 in the Ethiopian Demographic Health Survey (EDHS 2016) to 30 in the Ethiopian Min Demographic Health Survey (EMDHS 2019) per 1000 live births, respectively [10].
The consequences of an undiagnosed and untreated neonatal near miss were severe, and various literature indicates that NNM is a condition in which newborns develop complications during the neonatal period, resulting in a nearly higher prevalence of neonatal and infant death and cognitive and neurological development impairment in infants and childhood [11].
Despite the fact that neonatal near misses are preventable and treatable with effective care during pregnancy, delivery and postpartum care, the magnitude of neonatal near misses in Ethiopia increased from 29 to 30 per 1000 live births in 2019. The magnitude of neonatal near miss and its factors were not addressed in clinical experiences and studies around the world that show the neonate’s health suffers serious consequences due to physiological, pathological and immunity status that lead to permanent and temporal cognitive and neurological impairment in infants and children. Therefore, the aim of this study was to assess the magnitude of neonatal near misses and associated factors among neonates delivered at Alert comprehensive specialized hospital, Addis Ababa, Ethiopia [12].
Materials and Methods
Study design, study area and period
An institutional based cross sectional study design was employed. The study was conducted in Alert comprehensive specialized hospital, which was one of the public hospitals found in Addis Ababa, which is the capital city of Ethiopia, from March 1st 2022, up to April 15th 2022, among neonates admitted to neonatal intensive care. In the west of Addis Ababa, an alert comprehensive specialized hospital was discovered. It is 11 kilometers from the piazza and has an estimated total catchment population of 866506. Which offers obstetrics and gynecologic services to mothers and newborns and which has 11 catchment areas from governmental HC and 4 hospitals with 11 beds and 3 deliveries Koch from delivery ward and 2 gynecological operation tables, 61 postpartum beds and 1 bed in the emergency room?. In this hospital, there are 9 senior specialists, 90 midwives, 38 nurses, 5 general practitioners and 5 seniors in the NICU. It provided NICU service. The service included phototherapy service, Kangaroo Mother Care (KMC), neonatal ICU, septic service, maternal side service and neonatal outpatient service. There will be 1980 neonatal admissions and 180 neonatal deaths beginning with the 2020 year of service.
Population
Source population: All live born neonates are delivered at alert comprehensive specialized hospital.
Study population: All live born neonates delivered at alert comprehensive specialized hospital during the study period.
Sample population: All systematically selected neonates delivered at alert comprehensive specialized hospital during the study period.
Eligibility criteria
Inclusion criteria: All live birth neonates delivered in the hospitals during the study period.
Exclusion criteria: Those mothers who gave birth at home and were critically ill during the data collection time were excluded from the study and neonates who were referred from other health care institutions that were outside of the study hospitals were also excluded.
Sample size determination
The sample size was determined using the single population proportion formula. The following assumption was considered: Prevalence of neonatal near miss among neonates: 33.4%. 95% levels of confidence (Z=1.96), 5% marginal error (d=0.05) and 10% for rate of non-response.
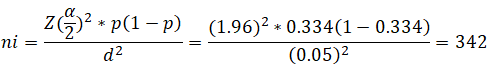
Where;
ni=Initial sample size.
Z=Confidence interval’s standardized normal distribution curve value.
P=Prevalence of neonatal near misses.
d=Margin of error.
After adding a 10% non-response rate, the final sample size was 377.
Sampling technique and procedure
During the study period, that means from March 1st to April 15th, 2022, the total number of live birth deliveries at alert comprehensive specialized hospital will be 720. Then the study units were selected using a systematic random sampling technique at every Kth interval, which were every two newborns. K (skip interval) was calculated as follows: By dividing the source population by the total sample size, K=720÷377≈2. Then the first neonate with mothers who were eligible was selected by lottery and this continued every K interval until the sample size was achieved.
Data collection tool, persons and procedures
Data were collected using standardized, validated and semi structured questionnaires’ with interviews. The tool was developed/ adapted from previous related literature done in Ethiopia [13-18]. But the questions that assessed the outcome variable were adopted from standardized, validated and reliable sources [19]. The tool has generally three parts involving maternal and paternal socio demographic characteristics, reproductive and obstetric history and medical history during pregnancy and new-born characteristics. One B.Sc. holder midwife was recruited for data collection and one B.Sc. holder midwife was recruited for supervisory activities, which communicated on a regular basis with data collectors to ensure that the data collection procedure was followed. Data was collected through face to face interviews with the neonates’ mothers and standard data extraction checklists from the medical record were used to collect the data. Near miss events were identified by data collectors from neonates’ medical records according to the criteria of CLAP. The tool used to assess the outcome variables (NNM) has good internal reliability with an overall Cronbach’s alpha of 0.80.
Study variables
Dependent variable: Neonatal Near Miss (NNM).
Independent variables
Socio demographic factors: Maternal age, marital status, occupational status, maternal educational status, paternal educational status, educational status and monthly income.
Obstetric factors: Parity, history of still birth, history of abortion, history of neonatal death, history of preterm birth, ANC follow up, mode of delivery (C/S, vaginal, instrumental, PROM, chronic illness and anemia.
Newborn factors: Fetal presentation, sex of newborn, weight of newborn and congenital anomaly.
Operational and term definitions
Neonatal near miss: NNM was considered when the newborn faced at least one of the following proposed criteria but survived.
Pragmatic criteria: Birth weight <1750 g, gestational age <33 weeks, 5th minute Apgar score <7.
Management criteria: Absence of regular breathing, bradycardia <80 bpm, respiratory rate >70 bpm, positive pressure ventilation, nasal CPAP, intubation for suctioning, use of corticosteroids, within 24 hours inability to sucking, use of vasoactive drugs, neural tube defect, recurrent seizure, anuria lasting more than 6 hours, bilirubin level greater than 10 mg/dl within 24 hours, phototherapy in the first 24 hours, there is jaundice. Hgb <10 g/dl, WBC <4000 cells/mm3, blood glucose level <40 mg/dl in 24 hours, first week surgery 64134 weeks gestation, temperature 6 hours-12 hours <35°C.
Prolonged labor: It is considered when the labor, after the latent phase of first stage of labor, exceeds 20 hours in primigravida or >14 hours in multipara mothers.
Prolonged Rapture of Membranes (PROM): It is considered rupturing of membranes lasting longer than 18 hrs [20].
Still birth: The death of fetuses weighing at least 1000 gm or 28 weeks of gestation or more.
Data quality control
A pre-test was done on 38 (10%) of the sample population before the actual data collection at Yekatit 12 hospital. As a result of the pretest modification on logical sequence, any ambiguity, as well as missed points, was added into the final version of the questionnaire.
Two day training for data collectors and supervisors was given by the principal investigator to make them familiar with data collection tools, various ethical issues, data collection methodologies and the objectives of the study. During the data collection, the supervisors reviewed the completed questionnaires for critical information. Additionally, the principal investigator routinely reviewed the consistency, completeness and cleanliness of the files that the data collector sent.
Data processing and analysis
After the data was collected and entered in Epi-Data version 4.6, it was exported to SPSS version 26 and checked for completeness, cleaned and coded. Descriptive statistics were performed to describe the study participants’ characteristics. The Variance Inflation Factor (VIF) was used to determine if there was correlation between two or more independent variables and it was tolerated when VIF 5 was used. The goodness of fit of the model was tested by Hosmer and Lemeshow and it was found to be 0.21. Both bivariate and multivariate logistic analyses were used to assess the association between each independent variable and the outcome variable.
All variables with a p-value <0.25 at 95% CI in the binary logistic regression model were transformed into the final multivariable logistic analysis in order to control all potential confounding variables. The Odds Ratio (OR) with 95% Confidence Interval (CI) was calculated to assess the strength of the association factors influencing neonatal near miss. In this study, a variable with a p-value of <0.05 was considered statistically significant. Finally, the data was organized and presented using text, tables and figures.
Results
Socio demographic characteristics of the study participants
A total of 377 mothers and live birth neonates who were delivered in comprehensive specialized hospitals were reviewed in this study, with a response rate of 361 (94.8%) and 16 (4.25%) of participants were excluded due to incomplete maternal or neonatal data records. The mean age of the mother was 27.1 (SD: 4.5) years, with minimum and maximum ages of 18 and 42, respectively. Among the study participants, 233 (46.5%) were within the age group of 25 years-34 years. Of the participants, 330 (91.4%) were urban residents. In terms of marital status, 346 (95.8%) were married, 163 (45.2%) had a high school diploma or higher and 191 (52.9%) work for the government. Regarding the paternal educational status, 120 (33.2%) attended college or above and 115 (31.9%) work as government employees. Of the study participants, 292 (80.1%) had an average monthly income above the poverty line (Table 1).
| Characteristics | Frequency (n) | Percentage (%) |
|---|---|---|
| Age in years | ||
| 18-24 | 101 | 28.0 |
| 25-34 | 233 | 64.5 |
| ≥ 35 | 27 | 7.5 |
| Residence | ||
| Urban | 330 | 91.4 |
| Rural | 31 | 8.6 |
| Marital status | ||
| Married | 346 | 95.8 |
| Single | 15 | 4.2 |
| Educational level of mother | ||
| No formal education | 7 | 1.9 |
| Primary | 108 | 29.9 |
| Secondary | 83 | 23.0 |
| Diploma and above | 163 | 45.2 |
| Occupation status of mother | ||
| Government employed | 191 | 52.9 |
| House wife | 31 | 8.6 |
| Merchant | 73 | 20.2 |
| Daily laborer | 46 | 12.7 |
| Others@ | 20 | 5.6 |
| Paternal educational status | ||
| No formal education | 6 | 1.7 |
| Primary (1-8) | 118 | 32.7 |
| Secondary | 117 | 32.4 |
| Collage and above | 120 | 33.2 |
| Paternal occupation | ||
| Government employed | 115 | 31.9 |
| Merchant | 70 | 19.4 |
| Private employed | 51 | 14.1 |
| Daily worker | 101 | 28.0 |
| Others# | 21 | 6.6 |
| House hold monthly income | ||
| Below poverty line | 69 | 19.1 |
| Above poverty line | 292 | 80.9 |
Note: Key-Others@-student, private employed and others#- farmer, student.
Table 1: Socio demographic characteristics study participants at alert comprehensive specialized hospitals, Addis Ababa, Ethiopia, 2022 (n=377).
Obstetrics and gynecologic characteristics of the participants
More than half of the participants (188 or 52.1%) were multigravida, having given birth 2 times-4 times. Regarding the abortion histories of the mothers, 46 (12.7%) had at least one history of abortion and 16 (4.4%) had a history of stillbirth. Of those study participants, 76 (21.1%) and 90 (24.9%) had histories of and neonatal death, respectively. In terms of mode of delivery, the majority of women (196 or 54.3%) had spontaneous vaginal deliveries, with 101 or 28%, having a caesarean section and also according to the findings, 218 (60.4%) of the newborns had a normal presentation and more than half of the other 199 (55.1%) were female (Table 2).
| Characteristics | Category | Frequency | Percentage % |
|---|---|---|---|
| Parity | Primiparous | 112 | 31.0% |
| Multiparous | 188 | 52.1% | |
| Grand multiparous | 61 | 16.9% | |
| History of abortion | Yes | 46 | 12.7% |
| No | 315 | 87.3% | |
| History of still birth | Yes | 16 | 4.4% |
| No | 345 | 95.6% | |
| History of preterm birth | Yes | 76 | 21.1% |
| No | 285 | 78.9% | |
| History of neonatal death | Yes | 90 | 24.9% |
| No | 271 | 75.1% | |
| Mode of delivery | SVD | 196 | 54.3% |
| Instrumental | 64 | 17.7% | |
| CS | 101 | 28.0% | |
| Fetal presentation | Normal | 218 | 60.4 |
| Mal-presentation | 143 | 39.6 | |
| Sex of neonate | Male | 162 | 44.9 |
| Female | 199 | 55.1 |
Table 2: Obstetrics, gynecologic characteristics of study participants in alert comprehensive specialized hospitals, Addis Ababa, Ethiopia, 2022 (n=377).
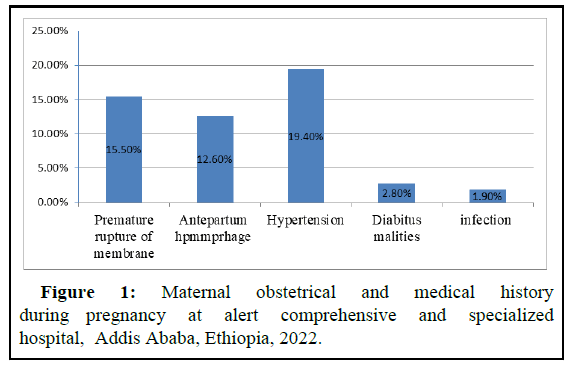
Maternal obstetrical and medical history during pregnancy
In this study, out of 361, 15.5% of the mother’s experienced premature rupture of membranes and 12.6% of the mothers developed antepartum hemorrhage of the mothers, 19.4% had pregnancy related or chronic hypertension and 2.8% had gestational or pre-gestational diabetes mellitus. Only 7 (1.9% of mothers) became infected (Figure 1).
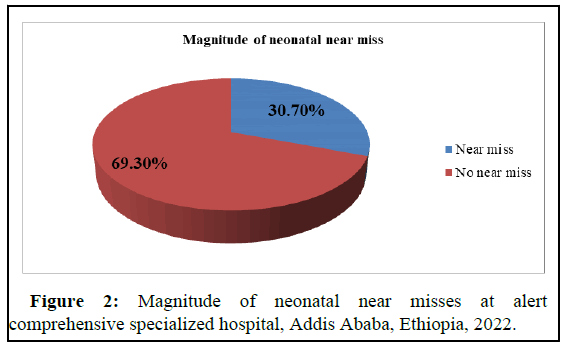
Magnitude of neonatal near misses
The overall magnitude of neonatal near misses among new born babies delivered at alert comprehensive specialized hospital in Addis Ababa was 111 (30.7%), 95% CI: 26.3, 35.7) (Figure 2).
Factors associated with neonatal near miss
Bivariate analysis was used in this study to identify variables associated with neonatal near miss with a p-value less than 0.25. In binary logistic regression analysis, eleven independent variables were associated with neonatal near miss, including household monthly income, parity, previous history of abortion, history of preterm birth, history of neonatal death, mode of delivery, fetal presentation, PROM in this pregnancy, APH, iron intake and history of chronic pregnancy induced hypertension.
The odds of a neonatal near miss were 2 times (AOR: 2.88, 95% CI: 1.37, 6.06) higher among mothers with monthly household income below the poverty line as compared to those who had monthly income above the poverty line. Mothers who had previously experienced neonatal deaths had a 14 fold increased risk of neonatal near miss than mothers who had no previous history of neonatal near miss (AOR: 13.5; 95% CI: 6.67, 27.48).
The odds of a neonatal near miss were 3 times higher (AOR: 2.56, 95% CI: 1.30, 5.06) and highly statistically significant among mothers who delivered their babies via caesarean section versus mothers who delivered their babies naturally. The odds of a neonatal near miss were 3 times higher among mothers who do not take iron with folic acid during pregnancy than those mothers who take iron with folic acid during pregnancy (AOR: 3.32, 95% CI: 1.58, 6.97) (Table 3).
| Variables | Neonatal near miss | ||||
|---|---|---|---|---|---|
| Yes (%) | No (%) | COR (95% CI) |
AOR (95% CI) |
P-value | |
| House hold monthly income | |||||
| Below poverty line | 40 (58.0) | 29 (42.0) | 4.29 (2.48-7.42) |
2.88 (1.37-6.06) |
0.005 |
| Above poverty line | 71 (24.3%) |
221 (75.5) |
1 | 1 | |
| Parity | |||||
| Primiparous | 24 (21.4) | 88 (78.6) | 1 | 1 | |
| Multiparous | 49 (26.1) | 139 (73.9) | 1.29 (0.74-2.25) | 0.83 (0.41-1.67) | 0.604 |
| Grand multiparous | 38 (62.3) | 23 (37.7) | 6.05 (3.04-12.0) | 1.50 (0.57-3.91) | 0.407 |
| History of neonatal death | |||||
| Yes | 69 (76.7) | 21 (23.3) | 17.9 (9.94-32.28) |
13.54 (6.67-27.48) | 0.001 |
| No | 42 (15.5) | 229 (84.5) | 1 | 1 | |
| History of preterm birth | |||||
| Yes | 38 (50.0) | 38 (50.0) | 2.90 (1.98-4.57) | 0.63 (0.24-1.64) | 0.352 |
| No | 73 (25.6) | 212 (74.4) | 1 | 1 | |
| History of abortion | |||||
| Yes | 26 (56.5) | 20 (43.5) | 3.51 (1.86-6.63) | 1.16 (0.35-3.77) | 0.804 |
| No | 85 (27.0) | 230 (73) | 1 | 1 | |
| Fetal presentation | |||||
| Normal presentation | 47 (21.6) | 171 (78.4) | 1 | 1 | |
| Mal presentation | 64 (44.8) | 79 (55.2) | 2.94 (1.85-4.67) | 1.63 (0.87-3.06) | 0.123 |
| Mode of delivery | |||||
| SVD | 35 (17.9) | 161 (82.1) | 1 | 1 | |
| Instrument assisted | 21 (32.8) | 43 (67.2) | 2.24 (1.18-4.24) | 1.16 (0.48-2.77) | 0.739 |
| Cesarean section | 55 (54.5) | 46 (45.4) | 5.50 (3.21-9.39) | 2.56 (1.30-5.06) | 0.007 |
| Premature rupture of membrane | |||||
| Yes | 31 (55.4) | 25 (44.6) | 3.48 (1.94-6.26) | 0.81 (0.24-2.72) | 0.739 |
| No | 80 (26.2) | 225 (73.8) | 1 | 1 | |
| Ante partum hemorrhage | |||||
| Poor | 24 (53.3) | 21 (46.7) | 3.00 (1.59-5.68) | 1.42 (0.47-4.28) | 0.525 |
| Moderate | 87 (27.5) | 229 (72.5) | 1 | 1 | |
| Does she taken full doe of iron with folic acid | |||||
| Yes | 72 (25.2) | 214 (74.8) | 1 | 1 | |
| No | 39 (52.0) | 36 (48.0) | 3.22 (1.90-5.44) | 3.32 (1.58-6.97) | 0.001 |
| History of hypertensions | |||||
| Yes | 32 (45.7) | 38 (54.3) | 2.26 (1.32-3.86) | 1.88 (0.87-4.06) | 0.107 |
| No | 79 (27.1) | 212 (72.9) | 1 | 1 | |
Note: Key-Bold font indicates statistical significant, at p-value <0.05, 1-Reference.
Table 3: Bi-variate and multivariable analysis of factors affecting neonatal near miss, at alert comprehensive specialized hospital, Addis Ababa, Ethiopia, 2022 (n=377).
Discussion
The overall magnitude of neonatal near misses among newborns delivered at the alert comprehensive specialized hospital in Addis Ababa was 30.7% (95% CI: 26.3-35.7) in this study. The result of this study was in line with the findings of Brazil (30.37%), Hawassa (33.4%), Debretabor (32.9%), Jimma (26.7%) and South Ethiopia (31.4%).
However, the magnitude of the neonatal near miss in this study was lower than studies done in Uganda (36.7%) and Morocco (43%). This lower neonatal near miss in this study might be due to the fact that the Uganda and Morocco studies included newborns born from mothers who had severe obstetric complications, unlike the present study. These obstetrical complications during pregnancy, labor and delivery could lead to life threatening conditions in neonates and place them in the NNM and another possible explanation may be differences in socio demographics and facility care.
Also, the result of this study was lower than the finding done in different part of Ethiopia, East Wollega 48.6% and south Ethiopia 45.1%. The possible reason might be due to the difference in the source population; the study done in Wollega involves neonates already admitted to the NICU.
On the other hand, the finding is higher than studies conducted in North Eastern Brazil 22% and other study done in Brazil 3.3%, India 8.7%, WHO 7.2%, Ghana 5.7%, Nepal 7.2% and also the magnitude of this study was higher than studies in Ethiopia, Injibara 23.3%. The possible difference might be due to differences in socioeconomic status, the instrument used for the definition of a near miss and the time of data collection. For example, studies done in southeastern and Northeastern Brazil, India, and elsewhere used solely pragmatic criteria to identify NNM, whereas this study used both pragmatic and management criteria.
This study found that neonates born to low income mothers had a 2 fold higher rate of neonatal near misses than those born to mothers with monthly incomes above the poverty line. This finding of this study was supported by studies conducted in and also supported by studies conducted in South Ethiopia and Dire Dewa. This could be due to the fact that women with high incomes may have better access to health care services and better living conditions. A study of neonatal survival reported that poor household income increased neonatal morbidity and mortality either by reducing access to effective and quality care or by increasing the rate of infection.
The odds of NNM were 14 times higher among neonates’ mothers who had a history of neonatal death as compared to their counterparts. A facility based, unmatched case control study design in Guji and Borena zones selected public hospitals in Southern Ethiopia supported this finding and also supported by findings from India. This congruency might be due to the fact that women who have a previous history of neonatal death might be challenged with various mental illnesses, like stress and depression, which persist long after the death of their neonate and undermine their confidence in achieving future pregnancy success. Moreover, women whose babies have been stillborn feel stigmatized, socially isolated and less valued by society and the effect could persist for the subsequent pregnancies. This indicated the need to emphasize and strengthen high quality antenatal, intrapartum and postnatal care for women and their newly born infants effectively.
When compared to spontaneous vaginal delivery, the odds of a neonatal near miss were 3 times higher and highly statistically significant among mothers who delivered their newborns via caesarean section. The result of this study was consistent with the findings of the studies done in Gamo Gofa, Southern Ethiopia, Jimma zone, southwest Ethiopia Gurage zone, which found that cesarean delivery had an increased risk of NNM. Cesarean delivery was associated with an increased risk of an Apgar score less than 7 at the 5th minute, preterm birth, low birth weight, neonatal resuscitation and admission to a Neonatal Intensive Care Unit (NICU), all of which increased the likelihood of becoming a near miss. However, this finding contradicts the Nepal finding that stated caesarean section was negatively associated with neonatal near death.
Furthermore, cesarean section newborns had less skin to skin contact with their mothers immediately after delivery, making the neonates unable to breastfeed within one hour of birth, putting the neonate at greater risk of premature birth.
The odds of a neonatal near miss were 3 times higher among mothers who do not take iron with folic acid during pregnancy than those mothers who take iron with folic acid during pregnancy. Even though there were no previous studies that supported it, not taking iron with folic acid during pregnancy indicates a lack of prenatal care. This increases congenital fetal anomalies, maternal anemia, low birth weight and preterm birth all of which are strongly linked to neonatal near misses.
Conclusion
In the study area, the magnitude of the neonatal near miss was high. This high neonatal near miss rate was found to be significantly related to household monthly income, previous neonatal near miss history, cesarean section delivery and not taking iron with folic acid during pregnancy. Pregnant women would develop themselves holistically for the care of themselves and their newborns and they would take iron with folic acid during pregnancy to prevent diseases and promote the health of the unborn fetus in order to prevent NNM.
References
- Li Z, Hsiao Y, Godwin J, Martin BD, Wakefield J, et al. (2019) Changes in the spatial distribution of the under-five mortality rate: Small area analysis of 122 DHS surveys in 262 subregions of 35 countries in Africa. PLoS One 14.
[Crossref] [Google Scholar] [PubMed]
- Santos JP, Cecatti JG, Serruya SJ, Almeida PV, Duran P, et al. (2015) Neonatal near miss: The need for a standard definition and appropriate criteria and the rationale for a prospective surveillance system. Clinics 70: 820-826.
[Crossref] [Google Scholar] [PubMed]
- Binns C, Low WY (2015) Neonatal public health: Progress and challenges. Asia Pac J Public Health 27: 688-689.
[Crossref] [Google Scholar] [PubMed]
- Zimmerman LA, Yi Y, Yihdego M, Abrha S, Shiferaw S, et al. (2019) Effect of integrating maternal health services and family planning services on postpartum family planning behaviour in Ethiopia: Results from a longitudinal survey. BMC Public Health 19: 1-9.
[Crossref] [Google Scholar] [PubMed]
- Avenant T (2009) Neonatal near miss: A measure of the quality of obstetric care. Best Pract Res Clin Obstet Gynaecol 23: 369-374.
[Crossref] [Google Scholar] [PubMed]
- Tekola AF, Baye G, Amaje E, Tefera K (2021) Neonatal near misses and associated factors among mother’s who give a live neonate at Hawassa city governmental hospitals, 2019: A facility based cross sectional study design. BMC Pregnancy Childbirth 21: 1-9.
[Crossref] [Google Scholar] [PubMed]
- Kale PL, Mello-Jorge MH, Silva KSD, Fonseca SC (2017) Neonatal near miss and mortality: Factors associated with life threatening conditions in new-borns at six public maternity hospitals in southeast Brazil. Cad Saude Publica 33.
[Crossref] [Google Scholar] [PubMed]
- McKinnon B, Harper S, Kaufman JS, Bergevin Y (2014) Socioeconomic inequality in neonatal mortality in countries of low and middle income: A multicountry analysis. Lancet Glob Health 2: e165-e173.
[Crossref] [Google Scholar] [PubMed]
- Mehari MA, Maeruf H, Robles CC, Woldemariam S, Adhena T, et al. (2020) Advanced maternal age pregnancy and its adverse obstetrical and perinatal outcomes in Ayder comprehensive specialized hospital, Northern Ethiopia, 2017: A comparative cross-sectional study. BMC Pregnancy Childbirth 20: 1-10.
[Crossref] [Google Scholar] [PubMed]
- Mersha A, Bante A, Shibiru S (2019) Factors associated with neonatal near miss in selected hospitals of Gamo and Gofa zones, Southern Ethiopia: Nested case control study. BMC Pregnancy Childbirth 1: 1-8.
[Crossref] [Google Scholar] [PubMed]
- Obiechina N, Okolie V, Eleje G, Okechukwu Z, Anemeje O (2011) Twin versus singleton pregnancies: The incidence, pregnancy complications, and obstetric outcomes in a Nigerian tertiary hospital. Int J Women Health 3: 227.
[Crossref] [Google Scholar] [PubMed]
- Oza S, Lawn JE, Hogan DR, Mathers C, Cousens SN (2014) Neonatal cause of death estimates for the early and late neonatal periods for 194 countries: 2000-2013. Bull World Health Organ 93: 19-28.
[Crossref] [Google Scholar] [PubMed]
- Asaye MM, Gelaye KA, Matebe YH, Lindgren H, Erlandsson K (2022) Valid and reliable neonatal near miss assessment scale in Ethiopia: A psychometric validation. Glob Health Action 15.
[Crossref] [Google Scholar] [PubMed]
- Morais LR, Patz BC, Campanharo FF, Dualib PM, Sun SY, et al. (2019) Neonatal near miss among new-borns of women with type 1 diabetes mellitus. Obstet Gynecol Int 2019.
[Crossref] [Google Scholar] [PubMed]
- Tassew HA, Kassie FY, Mihret MS (2020) Neonatal near miss and its predictors among neonates delivered at Debretabor general hospital, northern Ethiopia; A retrospective analysis. Int J Pediatr 2020.
[Crossref] [Google Scholar] [PubMed]
- Wondimu M, Balcha F, Bacha G, Habte A (2021) The magnitude of neonatal near miss and associated factors among live births in public hospitals of Jimma zone, Southwest Ethiopia, 2020: A facility based cross sectional study. PLoS One 16.
[Crossref] [Google Scholar] [PubMed]
- Tekelab T, Chojenta C, Smith R, Loxton D (2020) Incidence and determinants of neonatal near miss in South Ethiopia: A prospective cohort study. BMC Pregnancy Childbirth 20: 1-13.
[Crossref] [Google Scholar] [PubMed]
- Nakimuli A, Mbalinda SN, Nabirye RC, Kakaire O, Nakubulwa S, et al. (2015) Still births, neonatal deaths and neonatal near miss cases attributable to severe obstetric complications: A prospective cohort study in two referral hospitals in Uganda. BMC Paediatr 15: 1-8.
[Crossref] [Google Scholar] [PubMed]
- Ronsmans C, Cresswell JA, Goufodji S, Agbla S, Ganaba R, et al. (2016) Characteristics of neonatal near miss in hospitals in Benin, Burkina Faso and Morocco in 2012-2013. Trop Med Int Health 21: 535-545.
[Crossref] [Google Scholar] [PubMed]
- Gutema EA, Getachew Erena M, Kasaye HK (2022) Neonatal near miss and associated factors among neonates admitted to neonatal intensive care unit of hospitals in East Wollega, Western Ethiopia, 2019. SAGE Open Med 10.
[Crossref] [Google Scholar] [PubMed]
Citation: Bitaw A, Miheretie Y, Godie Y, Mamo A (2023) Magnitude and Associated Factors of Neonatal Near Miss among Neonates Delivered at Alert Comprehensive Specialized Hospital, Addis Ababa, Ethiopia, 2022: A Cross Sectional Study. J Preg Child Health 10: 594.
Copyright: © 2023 Bitaw A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 2472
- [From(publication date): 0-2023 - Dec 23, 2025]
- Breakdown by view type
- HTML page views: 2069
- PDF downloads: 403