Magnitude of Post-Partum Hemorrhage among Women Who Received Postpartum Care at Bedele Hospital South West, Ethiopia, 2018
Received: 03-Oct-2018 / Accepted Date: 29-Oct-2018 / Published Date: 05-Nov-2018 DOI: 10.4172/2376-127X.1000396
Abstract
Excessive bleeding after childbirth is a leading cause of maternal deaths worldwide, has gained international attention among medical and research communities for decades. Postpartum hemorrhage has long and short term impacts like, chronic illness, disability, increased risk of death and/or poor growth and development of their children, hepatic dysfunction, respiratory distress syndrome and renal failure and postpartum hemorrhage continues to be the leading single direct cause of maternal mortality worldwide.
Objective: To assess magnitude of post-partum hemorrhage among women who received postpartum care at Bedele hospital Southwest, Ethiopia, 2018.
Method: Institutional based cross sectional study design was employed and systematic sampling technique was used to select study participants. The total sample (200) were selected from mother’s chart every six interval and from the selected charts, the data was collected by using well prepared check list. Pre-test was performed to evaluate the appropriateness of instrument and after data collection it was processed and analyzed in a line of its objective and frequency and percentage of the result were presented in tables, graphs and narrative forms.
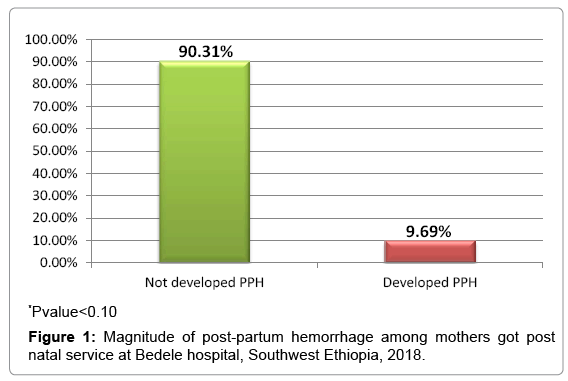
Result: Out of the total 200 charts, 196 charts were included in the study which gives 98% of response rate. The Magnitude of postpartum hemorrhage among women who got post natal service at Bedele hospital was 19 (9.69%). According to this study the postpartum hemorrhage was more prevalent among age group ≥ 35 and <20 years old. Among mothers who encountered postpartum hemorrhage were 13 (68 %) 4 (21%) and 2 (11%) give birth at hospital, health center and home respectively.
Conclusion and recommendation: The magnitude of postpartum hemorrhage was high despite many women receiving uterotonic during delivery of the babies. To reduce the prevalence of postpartum hemorrhage every health care provider conducting delivery have to performs active management of third stage of labor, manual removal of retained placenta.
Keywords: Postpartum-hemorrhage; Magnitude; Bedele hospital
Abbreviations
AAU: Addis Ababa University; AMTSL: Active Management of Third Stage Labor; ANC: Ante-Natal Care; APH: Ante Partum Hemorrhage; EDHS: Ethiopian Demographic Health Survey; WHO: World Health Organization; MCH: Mother and Child Health; MDG: Millennium Development Goal; MMR: Maternal Mortality Rate; LNMP: Last Normal Menstrual Period; PPH: Postpartum Hemorrhage; SVD: Spontaneous Vaginal Delivery; TBA: Traditional Birth Attendant.
Introduction
Excessive bleeding after childbirth is a leading cause of maternal deaths worldwide, has gained international attention among medical and research communities for decades [1].
Postpartum Hemorrhage (PPH) is a loss of 500 mL or more of blood during and after vaginal delivery or a blood loss greater than 1000 mL through a cesarean section. Any amount of blood loss during childbirth that compromises the hemodynamic status of the patient also constitutes PPH [2].
PPH is caused by many reasons, the commonest being uterine atone, which is responsible for 80% of the cases. Risk factors for uterine atone includes: Prolonged first and/or second stage of labor, augmented labor, retained placenta, placental accrete, multiple pregnancy, poly hydramnios and uterine fibroids. Multiparty and precipitate labor also promotes uterine atone. Uterine atone, retained products of conception, trauma in genital tract and coagulation abnormalities are important causes of PPH [3-5].
Postpartum hemorrhage has long and short term impacts like chronic illness, disability, increased risk of death and/or poor growth and development of their children, hepatic dysfunction, respiratory distress syndrome and renal failure [3,6,7]. Postpartum hemorrhage (PPH) continues to be the leading single direct cause of maternal mortality worldwide. In China, PPH is the most common serious obstetric complication and the leading cause of maternal mortality, accounting for 49.9% of maternal death [8].
Sub-Saharan Africa had the highest Maternal Mortality Rate (MMR) at 500 maternal deaths per 100 000 live births. Ethiopia is one of the few countries that account for most of the maternal deaths, others include India, Nigeria, Democratic Republic of the Congo, Pakistan, Sudan and Indonesia [2].
According to 2016 Ethiopian Demographic Health Survey (EDHS), the maternal mortality rate of Ethiopia is 412/100,000 live births [9]. Postpartum Hemorrhage (PPH) remains to be the leading cause of maternal mortality in developing countries like Ethiopia. The problem is worse in the rural setting where there are not proper facilities and trained health workers to administer injectable utero tonics, which are the standard treatment for PPH. Using community Health Extension Workers (HEWs) or Traditional Birth Attendants (TBAs) trained in the use of easier to use technologies could prevent PPH in rural Ethiopia [2,9]. Some unpublished documents claim PPH contributes 25%-30% of maternal deaths in Ethiopia [10].
Thus it is very crucial to assess the prevalence of postpartum hemorrhage in order to minimize the mortality and morbidity of women due to postpartum hemorrhage and its complication.
Method and Materials
Study area and period
The study was conducted in Oromia region, Buno Bedele zone, at Bedele hospital from April 01-15/2018. Bedele is the capital town of Buno Bedele zone located at South west of Ethiopia and is found about 488 km from Addis Ababa, the capital city of Ethiopia. The hospital provides preventive, curative and diagnostic services to Bedele town Community and referral for surrounding health center.
The study design
Institutional based cross sectional study design was used.
Source and study population
All mothers who delivered and visited (labor and gynecology ward) at Bedele hospital during postpartum period from October 15, 2017 to April 15, 2018 considered as source of population and postpartum mothers who selected during study period considered as study population.
Inclusion and exclusion criteria
The patient records which have clearly documented charts were included in the study while charts with incomplete data of woman who receive postpartum care at Bedele hospital during a six month period were excluded.
Sample size and sampling techniques
Sample size determination: The sample size was determined by using single population proportion formula by considering the following assumption: d=margin of error of 5% with 95% confidence interval, proportion of post-partum 17% (10), by considering 10% of none response rate the total sample size was 200 charts.
Sampling techniques: All unique medical registration numbers of clients who had got postnatal care from October 15 to April 15, 2017/18 were selected from the delivery registration and log books by using systematic sampling technique every six interval. The selected unique medical registration number was coded and the selected cards were taken from the card room.
Operational and term definition
Postpartum hemorrhage: As clinical diagnosis of postpartum hemorrhage can be primary PPH or secondary PPH.
Primary postpartum hemorrhage: Is blood loss within 24 h after birth which involves heavier bleeding and is more likely to result in maternal morbidity and mortality.
Secondary post-partum hemorrhage: Is bleeding which occur after 24 h to 6 weeks after birth.
Data collection tools
A structured, pretested questionnaire was used for data collection. The questionnaire has five parts: Socio demographic characteristics, obstetric history, ante partum obstetric events, intra partum obstetric events and peri natal characteristic which were believed to address the objective.
Data collection procedure
The information was gathered from cards by using formally prepared check-lists to be filled by data collectors. The required data was collected from the charts by considering carefully all the variables stated in the socio demographic and obstetric data with attention to avoid any redundancy.
Data analysis
After completion of data collection the information was cleared, data were checked for completeness, missing value and compiled on the hand tally and descriptive analysis were used and the result was presented using tables, figure and narrative.
Data quality control
The quality of data was controlled starting from development of the questionnaire, questionnaire was developed after reviewing different literatures and questions was selected to meet the objective. Data were collected from charts using formally prepared check-list. Any error found during the process was corrected immediately. The principal investigator checked each questionnaire immediately. Any error which was found during the process was corrected immediately after data collection completed. Data quality was assured by performing pre-test to evaluate the appropriateness of data collection instrument.
Ethical consideration
The study was carried out after getting approval from the ethical clearance committee of Mizan Tepi University and it was forwarded to medical director then to record keepers or staffs. The names of mothers were not be included in the check-list rather a unique identification number was used. Accordingly, the concern of study subjects for confidentiality was assured.
Results
Out of the total 200 charts, 196 charts were included in the study which gives 98% of response rate. 81 (41.8%) participants were found between 20-24 age groups. More than half 116 (59.2) of the participants were live in Bedele town. Majority 172 (87.7%) of the participants gave birth in the hospital and most of participants 185 (94.4%) were married by their marital status (Table 1).
| Variable | Age in group | Frequency | Percentage (%) |
|---|---|---|---|
| Age of mother | <20 | 17 | 8.67 |
| 20-24 | 82 | 41.8 | |
| 25-29 | 71 | 36.2 | |
| 30-34 | 18 | 9.18 | |
| >35 | 8 | 4.08 | |
| Address | Bedele town | 116 | 59.2 |
| Out of Bedele town | 80 | 40.8 | |
| Place of delivery | Hospital | 172 | 87.7 |
| Health Center | 17 | 8.67 | |
| Home | 7 | 3.57 | |
| Marital status | Married | 185 | 94.4 |
| Single | 4 | 2 | |
| Divorced | 5 | 2.55 | |
| Separated | 2 | 1 |
Table 1: Socio-demographic characteristics of the study participants among women who got postnatal service birth at Bedele hospital, South West, Ethiopia, 2018.
Magnitude of postpartum hemorrhage
The magnitude of postpartum hemorrhage among women got post natal service at Bedele hospital was 19 (9.69%). According to this study the postpartum hemorrhage more prevalent among age group ≥ 35 and <20 years old. Among mothers encountered postpartum hemorrhage were 13 (68 %), 4 (21%) and 2 (11%) give birth at hospital, health center and home respectively (Figure 1).
Obstetrics characteristics
Majority 126 (64.3%) of participants had parity between two to four. Regarding gestational age, majority 173 (88.3%) of the participants were give birth at term and 168 (85.7%) of them had antenatal follow up. Most 184 (93.9%) of the study participants hadn’t history of previous abortion and only 10 (5.10%) and 9 (4.6%) had history of previous caesarian section and PPH respectively (Table 2).
| Variable | Categories | Frequency | Percentage (%) |
|---|---|---|---|
| Parity | 1 | 58 | 29.6 |
| 02 Apr | 126 | 64.3 | |
| ≥ 5 | 12 | 6.12 | |
| Gestational age in weeks | <37 | 8 | 4.08 |
| 37-42 | 173 | 88.3 | |
| >42 | 10 | 5.1 | |
| Unknown | 5 | 2.55 | |
| ANC follow up | Yes | 168 | 85.7 |
| No | 28 | 14.3 | |
| History of abortion | Yes | 12 | 6.1 |
| No | 184 | 93.9 | |
| History of previous caesarian section | Yes | 10 | 5.1 |
| No | 186 | 94.9 | |
| History of previous PPH | Yes | 9 | 4.6 |
| No | 187 | 95.4 |
Table 2: Obstetric characteristics among mothers who attended post natal service at Bedele hospital, Southwest, Ethiopia, 2018.
Obstetrics complication during current pregnancy and labour
Out of the total study participants, only 8 (4.1%) and 9 (4.6%) of them developed placenta abruption and placenta previa respectively. Most 188 (95.9%) of the participants were singleton birth. Among study participant, 12 (6.12%) of women had obstructed labor and 31 (15.2%) of them faced prolonged labour during current labour. Among mothers developed PPH, 3 (15.8%) and 5 (26.3%) encountered obstructed labour and prolonged labour respectively (Table 3).
| Variable | Categories | Frequency | Percentage (%) |
|---|---|---|---|
| Placenta abruption | Yes | 8 | 4.1 |
| No | 188 | 95.9 | |
| Placenta previa | Yes | 9 | 4.6 |
| No | 187 | 95.4 | |
| Status of pregnancy | Singleton | 188 | 95.9 |
| Twin | 8 | 4.1 | |
| Obstructed labour | Yes | 12 | 6.12 |
| No | 184 | 93.87 | |
| Prolonged labour | Yes | 31 | 15.2 |
| No | 165 | 84.2 |
Table 3: Distributions of obstetric complication during current pregnancy and labour among study participants at Bedele hospital, South west Ethiopia, 2018.
Intra-partum and postpartum events
From the total study participants, 176 (89.8%) of participants delivered through vagina and 183 (93.4%) of labour started spontaneously. Only 15 (7.6%) and 18 (9.2%) of participants faced prolonged third stage of labour and genital tract trauma respectively. Regarding third stage of labour, most of mothers 191 (97.4%) managed with active management of third stage of labour and majority 141 (69.1%) of new born weight were in the normal range (Table 4).
| Variable | Categories | Frequency | Percentage (%) |
|---|---|---|---|
| Mode of delivery | Vaginal | 176 | 89.8 |
| Caesarian section | 20 | 10.2 | |
| Onset of labor | Spontaneous | 183 | 93.4 |
| Induced | 13 | 6.6 | |
| Prolonged 3rd stage labor | Yes | 15 | 7.6 |
| No | 181 | 92.4 | |
| Genital tract trauma other than episiotomy | Yes | 18 | 9.2 |
| No | 178 | 90.8 | |
| Uterine rupture | Yes | 6 | 3.1 |
| No | 190 | 96.9 | |
| Uterine atone | Yes | 13 | 6.6 |
| No | 183 | 93.4 | |
| Active management of 3rd stage of labor | Yes | 191 | 97.4 |
| No | 5 | 2.6 | |
| Fetal weight in gram | <2500 | 30 | 14.7 |
| 2500-3999 | 141 | 69.1 | |
| ≥ 4000 | 21 | 10.3 | |
| Unknown | 12 | 5.9 |
Table 4: Distribution of study participants in their intra-partum and post-partum events, Southwest, Ethiopia, 2018.
Discussion
This study found that the magnitude of postpartum hemorrhage among mothers received postpartum care at Bedele hospital was 9.69. In this study the magnitude of postpartum hemorrhage was higher than the studies done in Amhara region (Desse referral hospital (5.8%) and Australia (4.4%) [11,12]. The discrepancy might be due to study area difference, the degree of prenatal, intra natal, postnatal care socioeconomic status could be a reason.
In this study, the magnitude of PPH was lower than the studies done in Pakistan (21.3%), Ethiopia, Gonder town (18%) and, Black lion and Gandhi hospitals (19.9%) [13-15]. The difference might be due the current health police of Ethiopia focus on the prevention of maternal and child death. Postpartum hemorrhage is the leading cause maternal mortality, so any interventions given for mothers during pregnancy, labour and delivery and postpartum reduce the occurrence of postpartum hemorrhage.
As this study revealed that the magnitude of postpartum hemorrhage is consistent with the studies done in Uganda (9%), Tanzania (11.9%) and global prevalence (10.5%) [2,15,16]. In Ethiopia now days, the government provides focused ANC for pregnant women based on evidence. Therefore pregnant women get interventions based on their problems. During ANC follow-up, potential risks for pregnancy related complications including PPH are predicted and interventions like, ironfolate supplementation, nutritional provision are important actions to reduce PPH.
In this study, prolonged labour and prolonged third stages of labour were highly proportional with postpartum hemorrhage. This finding is in line with other study done in other country. As the duration of labor increases the risk of developing PPH also increases. Prolonged labor will also cause uterine atone and uterine atone is the most leading cause of postpartum hemorrhage.
Greater parity 8 (42%), being primi parous which accounts 6 (32%), Advanced maternal age greater than 35 years and younger age less than 20 years have high proportion of postpartum hemorrhage. This finding is supported by different literatures [17]. As parity and maternal age in advance increases the pregnancy complications increases and chance uterine atone which cause post-partum hemorrhage also occur as age of mother increases in advance.
Limitation of this study is inappropriate documentation in some of the charts used and also poor quality of referral paper. Since the study was a hospital based study the results of the study may not show the true picture of the problem in the community.
Conclusion
The magnitude of postpartum hemorrhage was high despite many women receiving uterotonic at delivery of the babies. Uterine atone was the commonest cause for PPH followed by retained placenta and genital tract trauma other than episiotomy.
Ethical Approval and Consent to Participants
Written ethical approval was obtained from Mizan Tepi University research review committee. Permission was obtained from hospital manager and respective units.
Acknowledgment
We would like to express our deepest gratitude to our data collectors, hospital managers, case unites and study participants for their valuable contribution in the realization of this study. TA, DS, GA, MK and SH were developed a concept of research work, proposal development, data collection, analysis and writing findings. All authors read and approved the final manuscript.
References
- Karpati PC, Rossignol M, Pirot M, Cholley B, Vicaut E, et al. (2004) High incidence of myocardial ischemia during postpartum hemorrhage. Anesthesiology 100: 30-36.
- World Health Organization (2015) Maternal mortality fact sheet. WHO, Geneva.
- Abate T, Kebede B, Feleke A, Misganaw E, Rogers N (2014) Prospective study on birth outcome and prevalence of postpartum morbidity among pregnant women who attended for care in Gonder town, North West Ethiopia. J Androl 3: 125.
- Lutomski JE, Byrne BM, Devane D, Greene RA (2012) Increasing trends in atonics postpartum hemorrhage in Ireland: An 11-year population based cohort Study. BJOG 119: 306-314.
- Kramer MS, Berg C, Abenhaim H, Dahhou M, Rouleau J, et al. (2013) Incidence, risk factors and temporal trends in severe postpartum. Am J Obstet Gynecol 209: 1-7.
- Tort J, Rosenberg P, Traore M, Fournier P, Dumont A (2015) Factors associated with postpartum hemorrhage maternal death in referral hospitals in Senegal and Mali: A cross-sectional epidemiological survey. BMC Preg Childbirth 15: 235.
- Bhavana G, Abhishek MV, Mitta S (2016) A study of risk factor of postpartum hemorrhage and indications for caesarean section. Int J Reprod Contracept Obstet Gynecol 5: 2017-2021.
- Myles text book of obstetrics. (2009) Bennett VR (Edtn), 12th edition. Pp: 462470.
- Â Central Statistical Authority (2016) Ethiopia demographic and health survey. Central Statistical Agency, Addis Ababa and Calverton, USA.
- Gebeyehu R, Woyessa A (2012) Prevention of postpartum hemorrhage in rural Ethiopia. Pp: 13.
- Temesgen MA (2017) Magnitude of postpartum hemorrhage among women delivered at dessie referral hospital, South Woll, Amhara Region, Ethiopia. J Women's Health Care 6: 391.
- WHO, UNICEF, UNEPA, World Bank (2007) Maternal mortality in estimates developed. Geneva (Switzerland): WHO.
- Ali TS (2013) Department of community health sciences and school of nursing and midwifery, Aga Khan University, Karachi, Pakistan. J Ayub Med Coll Abbottabad 25: 1-2.
- Ononge S, Mirembe F, Wandabwa J, Campbell OMR (2016) Incidence and risk factors for postpartum hemorrhage in Uganda. Reproductive Health 13: 38.
- AbouZahr C (2003) Global burden of maternal death and disability, Br Med Bull 67: 1-11.
- Rath WH (2011) Postpartum hemorrhage-update on problems of definitions and diagnosis. Acta Obstet Gynecol Scand 90: 421-428.
- Ramakrishna J, Ganapathy S, Mahendra S (2008) After birth: Bananthana in rural Karnataka. Proceedings of reproductive health in India: New evidence and issues ministry of health and population.
Citation: Gudeta TA, Kebede DS, Negeri GA, Dow MK, Hassen S (2018) Magnitude of Post-Partum Hemorrhage among Women Who Received Postpartum Care at Bedele Hospital South West, Ethiopia, 2018. J Preg Child Health 5: 396. DOI: 10.4172/2376-127X.1000396
Copyright: © 2018 Gudeta TA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 6356
- [From(publication date): 0-2018 - Dec 05, 2025]
- Breakdown by view type
- HTML page views: 4643
- PDF downloads: 1713