Maternal Outcome of Pregnant Mothers with Hypertensive Disorder of Pregnancy at Hospitals in Wolaita Zone, Southern Ethiopia
Received: 18-Apr-2018 / Accepted Date: 08-May-2018 / Published Date: 15-May-2018 DOI: 10.4172/2376-127X.1000375
Abstract
Introduction: Hypertensive disorder of pregnancy (HDP) is a common and very severe medical disorder specific to pregnancy. The aetiology of the condition is unknown, but it is more commonly seen in primigravida and grandmuiltpara women, in association with multiple pregnancies and pre-existing medical problem such as essential hypertension, renal disease, diabetes mellitus and obesity.
Objective: To assess maternal outcome of pregnant mothers with hypertensive disorder of pregnancy from June 20 to November 20 at hospitals in Wolaita zone Southern Ethiopia.
Method: Institutional based cross sectional study design was conducted. All pregnant mothers with hypertensive disorder of pregnancy were included. Regular supervision and follow up was made. Data was entered into Epi info version 7 by investigators and was transported to SPSS version 20 for analysis. Bivariate and multivariate analysis was used to identify factors associated with maternal outcome.
Results: A total of 225 study subjects were included in the study of which majority of them were multiparous. Preeclampsia and eclampsia were the most common causes of maternal insults either during pregnancy or at the time of deliver. Being nulliparous was about three times more likely to develop poor maternal outcome when compared to being multiparous (AOR 3.45 (95% CI (0.043-15.152)).
Conclusion and recommendations: Hypertensive disorder of pregnancy is associated with increased risk of maternal adverse outcome. Therefore, close follow up of all laboring mother and provision of antihypertensive agent as per protocol is very important to control the impact of high blood pressure.
Keywords: Hypertension; Maternal outcome; Pregnancy
Abbreviations
ANC: Antenatal Care; BP: Blood Pressure; HDP: Hypertensive Disorder of Pregnancy; PIH: Pregnancy Induced Hypertension
Introduction
Hypertensive disorder of pregnancy (HDP) is a common and very severe medical disorder specific to pregnancy. The aetiology of the condition is unknown, but it is more commonly seen in primigravida and grandmuiltpara women, in association with multiple pregnancies and pre-existing medical problem such as essential hypertension, renal disease, diabetes mellitus and obesity [1].
According to Working Group of National High Blood Pressure Education Program, the hypertensive disorders can be classified into four types: 1) Gestational hypertension 2) Preeclampsia and Eclamptic syndrome 3) Preeclampsia syndrome superimposed on chronic hypertension 4) Chronic hypertension [2].
Despite of its major negative implications, its origin remains doubtful and the disease process is ultimately reversed only by delivery. However, evidence accumulated in the past 20 years indicates that abnormal placentation is one of the initial events. Preeclampsia is a syndrome complex induced by pregnancy after 20 weeks of gestation and characterized by development of high blood pressure associated with edema or proteinuria or both. Eclampsia is a preeclampsia with convulsion [3].
Hypertension is one of the commonest complications of pregnancy and is a common cause of fetal and maternal morbidity [4]. It is the third leading causes of maternal deaths next to haemorrhage and sepsis. The global incidence of HDP ranges from 5-10% of all pregnancies with a mortality rate of 5.5%. In African countries such as South Africa, Egypt, Tanzania and Ethiopia vary from 1.8% to 7% [5].
Therefore, it is very important to assess maternal outcome of pregnant mothers with hypertensive disorder of pregnancy in order to devise different strategies that helps to reduce maternal morbidity and mortality.
Materials and Methods
Study area and period
The data was collected from June 20 to November 20, 2014 at hospitals in Wolaita Zone. The administrative city of Wolaita Zone is Wolaita Soddo which is located at 334 Km away from Addis Ababa along the main highway that leads Arbaminch via Hosanna. There are three functional hospitals zone of which one is governmental hospital and the two are private hospital. Wolaita Soddo Hospital (WSTRH) is one of the governmental hospital located to the eastern part of municipality approximately 2 km from the center of the town. It was established in 1920 E.C. The hospital serves about three million people with a very wide catchments area of about 250 km radius. It has 150 beds and two operational theatres and have four major departments, Obstetrics and Gynecology, paediatrics, Internal medicine and surgery and four minor department, Psychiatry, ophthalmology, dentistry and followup clinics for chronic illness like TB, HIV/ADIS, diabetes mellitus the main diagnostic modalities in the hospital are: Routine laboratory investigation, radiological service, Gynecology and Obstetrics has maternal and child health (MCH) clinic, where pregnant women are having follow-up.
Study design
Hospital based cross-sectional study design was employed.
Source population
All pregnant mothers in Wolaita zone and other catchments area.
Study population
All pregnant mothers with HDP and those who gave birth at hospitals Wolaita zone from June 20 to November 20, 2014, SNNPR and Ethiopia.
Sample size determination and sampling technique
Census was used to include all pregnant mothers with HDP and those who gave birth/s at hospitals in Wolaita zone.
Data collection instruments and procedure
Pretested checklist or formats prepared in English and then translated to Amharic was used as data collection instrument. Training was given to data collectors and supervisors. During data collection three Bsc and seven diploma holder nurses were involved as supervision and data collection, respectively.
Data compilation
Once the data have been collected and checked for completeness and accuracy, it was sorted, categorized and summarized. Then, enter the data into the computer using developed data entry format, coded for each category of variables and checked for errors.
Data quality control
Data collectors was trained on each items included in the questionnaires. The developed questionnaires were translated to Amharic then back to English to see consistency of questionnaire. Supervisors cross checked for completeness and accuracy of data on daily basis.
Data processing and analyzing
The data was entered in to Epi info version 7 and transported to SPSS version 20 for further analysis. During the analyses p-value and/or 95% Confidence Interval (CI) of OR (odds ratio) was used to judge the significance of the associations. The results were presented in narrative, tables and graphs.
Ethical consideration
After approval of proposal, a letter of support and permission was obtained from Wolaita Soddo University research ethical review committee and given to Hospitals in Wolaita zone. The advantage and purpose of the study was explained to the participants. Then, for confidentiality of information a written consent was given to the participants and it should be used only for the study purpose. We don’t write the name of the participants so that information obtained was kept confidential.
Operational definition
Antenatal care: Is a medical and general care that is provided to pregnant women during pregnancy.
Mild pre-eclampsia: Two readings of diastolic blood pressure 90- 110 mm Hg, 4-6 h apart, after 20 weeks of gestation and with Proteinuria of >300 mg/l in 24 h or up to 2+ and with/without edema.
Severe pre-eclampsia: Diastolic blood pressure is equal or greater than 110 mm Hg after 20 weeks of gestation. There may be severe headache, blurred vision, epigastria pain, hyperreflexes, oligouria (urinary output equal or less than 400 mls/24 h), Proteinuria (protein equal or greater than 5 g/24 h, dipstick +++), increased weight (equal or more than 1000 g/week and the patient is conscious.
Good outcome: If the pregnant mothers didn’t develop any complication either during the course of pregnancy or delivery.
Poor outcome: If the pregnant mothers developed any complication either during the course of pregnancy or delivery.
Results
Personal and socio-demographic characteristics
Of the total 225 cases, the highest number of cases 49.8% (n=112) were belonged to the age group of 25-29 year followed by age group between 30-34, (28.88).The mean average is 28 (minimum 20 and maximum 38). None of them has history of exposure to alcohol drinking and smoking. Majority of pregnant mothers with HDP has ANC-follow up and most of them were multigravida and primigravida respectively (Table 1).
| Variable | Category | Frequency | Percentage |
|---|---|---|---|
| Age | 20-24 | 28 | 12.44 |
| 25-29 | 112 | 49.78 | |
| 30-34 | 65 | 28.88 | |
| 35-39 | 20 | 8.90 | |
| Gravida | Primigravida (1) | 95 | 42.2 |
| Mutigravia (2-4) | 116 | 51.6 | |
| Grand multigravida (>5) | 14 | 6.2 | |
| Address | Urban | 94 | 41.8 |
| Rural | 131 | 58.2 | |
| Ethnicity | Wolaita | 185 | 82.2 |
| Gamo | 15 | 6.7 | |
| Hadiya | 18 | 8 | |
| Alaba | 4 | 1.8 | |
| Other | 3 | 1.3 | |
| Educational level | University | 16 | 7.1 |
| College | 33 | 14.7 | |
| High school | 36 | 16 | |
| Intermediate school | 4 | 1.8 | |
| Primary school | 62 | 27.6 | |
| No illiterate | 74 | 32.9 | |
| ANC follow up | Yes | 191 | 84.9 |
| No | 34 | 15.1 |
Table 1: Personal and socio-demographic characteristics of pregnant mothers with hypertensive disorder of pregnancy from June 20 to November 20, at hospitals in Wolaita zone, Southern Ethiopia.
Current types of HDP
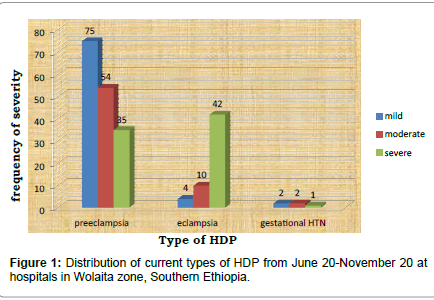
Of all pregnant mothers who gave births at hospitals in Wolaita zone, 72.9% (n=164) were preeclampsia, 25.8% (n=58) were eclampsia, 1.3% (n=3) were gestational HTN. None of the cases was diagnosed to have chronic HTN or superimposed preeclampsia. Most severe forms of hypertensive disorder in pregnancy were due to eclampsia and followed by preeclampsia (Figure 1).
Complication associated with HDP and mode of delivery
About 83.6% (n=188) gave birth without development of hypertensive related compactions. Of all pregnant mothers with hypertensive disorder of pregnancy, 7.1% (n=16) had renal failure, 5.8% (n=13) had pulmonary edema, 1.8% (n=4) had cerebral edema and 1.8% (n=4) were died. About 73.33% of all pregnant mothers with HDP were delivered by spontaneous vaginal delivery while the rests were given birth by caesarian section.
Determinants of maternal outcome
It was observed from a data of multivariate analysis that parity and high blood pressure were strongly associated with unfavourable maternal outcome at p-value less than 0.001. Being nulliparous was about three times more likely to develop poor maternal outcome when compared to being multiparous (AOR 3.45 (95% CI (0.043-15.152)) (Table 2).
| Variable | Category | Sig. | AOR (95% C.I.) | |
|---|---|---|---|---|
| Good outcome | Poor outcome | |||
| Age of mother in year | ||||
| 20-24 | 12 | 16 | 0.24 | 2.518 (0.023-12.86) |
| 25-29 | 92 | 20 | 0.14 | 1.113 (0.047-25.12) |
| 30-34 | 36 | 29 | 2.21 | 3.442 (0.086-10.56) |
| 35-39 | 7 | 13 | * | * |
| Gestational age | ||||
| Term | 122 | 40 | * | * |
| Preterm | 25 | 38 | 1.54 | 1.213 (0.021-8.14) |
| Parity | ||||
| Nulliparous | 37 | 58 | <0.001 | 3.45 (0.043-15.152) |
| Multiparous | 110 | 20 | * | * |
| Blood pressure | ||||
| 140/90-159/109 mm Hg | 92 | 40 | * | * |
| >160/110 mm Hg | 55 | 38 | 0.42 | 4.136 (0.172-23.458) |
| Type of HDP | ||||
| PIH | 4 | 1 | * | * |
| Preeclampsia | 108 | 56 | <0.001 | 2.132 (0.021-14.162) |
| Eclampsia | 35 | 21 | <0.001 | 5.345 (0.054-35.216) |
| ANC follow Up | ||||
| Yes | 135 | 56 | * | * |
| No | 12 | 22 | 0.54 | 5.657 (0.032-11.286) |
Table 2: Determinants of fetal outcome of pregnant mothers with hypertensive disorder of pregnancy from June 20 to November 20 at hospitals in Wolaita zone, Southern Ethiopia.
Discussion
The magnitude of pregnancy related hypertensive disorder in our study was 5.37% which is consistent with some other study [1,2]. But it is higher than the study conducted in on 255 consecutive cases of hypertensive disorder in pregnancy who were managed at Kocaeli University Hospital 2.4% [6]. The review of this study also found that magnitude of severe hypertensive disorder of pregnancy was found to be 34.67%. Another similar study also found that severe preeclampsia was common in 35.5% of pregnant mothers and followed by eclampsia [7,8]. This might be because most of the mothers were young ages and living in low socio-economic status which are the characteristics of hypertensive disorder of pregnancy.
In this review, it is found that hypertensive disorder in pregnancy is related with significant maternal morbidity and mortality that agrees with the findings reported elsewhere [9,10]. This study also found that the most common insult of hypertensive disorder in pregnancy is preeclampsia followed by eclampsia, but none of the pregnant mother has chronic hypertension which agrees with some other similar studies [11,12]. It is also found that most of maternal poor outcome were attributed by eclampsia. Compared to pre-eclampsia, eclampsia carries a much higher risk of death and serious morbidity for the woman and her baby [13].
In this study, it was found that that the most common consequences associated with hypertension diseases are the restriction of intrauterine growth, low birth weight which is consistent with other similar studies [14,15]. On the other hand, another study reported that the most common insult to the fetus is prematurity and intra-uterine fetal deaths [16,17].
In spite of doing several studies, the initiating events and exact management of preeclampsia are still unidentified. Currently delivery is the only definite cure for preeclampsia. There are standard guidelines verifying the route of delivery of pregnant mothers with hypertensive disorder in pregnancy and the findings of multiple studies have shown the advantages of vaginal delivery despite of increasing rate of caesarean section worldwide [17-19]. However, the frequency of caesarean section in the present study was 26.67%, which is lower than 34.3% reported by Gangly in 2007 [20]. This may be due the fact that this study is specific to the case of hypertensive disorder of pregnancy which cannot represent the frequency of all pregnant mother gave birth by caesarean section at hospitals in Wolaita zone.
Conclusion and Recommendation
Hypertensive disorder of pregnancy is associated with increased risk of maternal adverse outcome. young age group, nulliparous and high blood pressure were strongly associated with unfavourable maternal outcome. Commonest type of hypertensive disorder in pregnancy is preeclampsia and eclampsia. Majority of HDP cases were given birth by spontaneous vaginal delivery. Therefore, a continuous close follow up of all laboring mothers, provision of antihypertensive as per protocol and measuring of blood pressure of all pregnant mother at each visits is very important to control the impact of high blood pressure in the late trimester.
Funding
Wolaita Soddo University provided fund for data collectors.
Authors Contribution
MS have contributed to conception, design of the study, data acquisition, data entry, data analyses, result interpretation, manuscript development and revision. EW has contributed to conception, initial design of the study, data acquisition, data analyses, result interpretation and manuscript development. Both authors read and approve the final manuscript.
Acknowledgement
Firstly, we would like to thank Wolaita Soddo University for financial support. Then, would like to thank study participants for providing a high response rate.
References
- Herring CS, Heywood SG, Hatjis CG (2005) The multiple challenges in the management of a patient with HELLP syndrome, liver rupture and eclampsia. W V Med J 101: 261-262.
- Whelton PK, He J, Appel LJ, Cutler JA, Havas S, et al. (2002) Primary prevention of hypertension: Clinical and public health advisory from the national high blood pressure education program. JAMA 288: 1882-1888.
- Zhang C, Williams MA, King IB, Dashow EE, Sorensen TK, et al. (2002) Vitamin C and the risk of preeclampsia-results from dietary questionnaire and plasma assay. Epidemiology 13: 409-416.
- Villar J, Abdel-Aleem H, Merialdi M, Mathai M, Ali MM, et al. (2006) World Health Organization randomized trial of calcium supplementation among low calcium intake pregnant women. Am J Obstet Gynecol 194: 639-649.
- WHO (2005) The world health report 2005: Make every mother and child count.
- Yücesoy G, Ozkan S, Bodur H, Tan T, Calişkan E, et al. (2005) Maternal and perinatal outcome in pregnancies complicated with hypertensive disorder of pregnancy: A seven year experience of a tertiary care center. Arch Gynecol Obstet 273: 43-49.
- Misra DP, Kiely JL (1997) The association between nulliparity and gestational hypertension. J Clin Epidemiol 50: 851-855.
- Caritis S, Sibai B, Hauth J, Lindheimer M, VanDorsten P, et al. (1998) Predictors of pre-eclampsia in women at high risk. Am J Obstet Gynecol 179: 946-951.
- Rosenberg K, Twaddle S (1990) 6 Screening and surveillance of pregnancy hypertension-an economic approach to the use of daycare. Baillière's Clin Obstet Gynaecol 4: 89-107.
- Sibai B, Dekker G, Kupferminc M (2005) Pre-eclampsia. Lancet 365: 785-799.
- Roberts CL, Algert CS, Morris JM, Ford JB, Henderson-Smart DJ (2005) Hypertensive disorders in pregnancy: A population-based study. Med J Aust 182: 332-336
- Lawler J, Osman M, Shelton JA, Yeh J (2007) Population-based analysis of hypertensive disorders in pregnancy. Hypertens Pregnancy 26: 67-76.
- Brown MA, Hague WM, Higgins J, Lowe S, McCowan L, et al. (2000) The detection, investigation and management of hypertension in pregnancy: Full consensus statement. Aust N Z J Obstet Gynaecol 40: 139-155.
- Lauterbach MD, Raz S, Sander S, Craig J (2001) Neonatal hypoxic risk in preterm birth infants: The influence of sex and severity of respiratory distress on cognitive recovery. Neuropsychology 15: 411.
- Chaim SRP, De-Oliveira SMJV, Kimura AF (2008) Pregnancy-induced hypertension and the neonatal outcome. Acta Paul Enferm 21: 53-58.
- Leitner Y, Fattal-Valevski A, Geva R (2000) Six-year follow-up of children with intrauterine growth retardation: long-term, prospective study. J Child Neurol 15: 781-786.
- Zibaeenezhad M, Ghodsi M, Arab P, Gholzom N (2010) The prevalence of hypertensive disorders of pregnancy in Shiraz, Southern Iran. Iran Cardiovasc Res J 4: 169-172.
- Smith GC, Shah I, White IR, Pell JP, Crossley JA, et al. (2007) Maternal and biochemical predictors of antepartum stillbirth among nulliparous women in relation to gestational age of fetal death. BJOG 114: 705-714.
- Magee LA, Helewa M, Rey E (2008) Diagnosis, evaluation and management of the hypertensive disorders of pregnancy. J Obstet Gynaecol Can 30: S1-S2.
- Bhattacharjee N, Ganguly RP, Saha SP (2007) Misoprostol for termination of midâ€trimester postâ€Caesarean pregnancy. Aust N Z J Obstet Gynaecol 47: 23-25.
Citation: Obsa MS, Wolka E (2018) Maternal Outcome of Pregnant Mothers with Hypertensive Disorder of Pregnancy at Hospitals in Wolaita Zone, Southern Ethiopia. J Preg Child Health 5: 375. DOI: 10.4172/2376-127X.1000375
Copyright: © 2018 Obsa MS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 6042
- [From(publication date): 0-2018 - Oct 11, 2025]
- Breakdown by view type
- HTML page views: 4884
- PDF downloads: 1158