Metabolic Rehabilitation: Body Homeostasis through the Action of Photobiomodulation in Weight LossâA Comparative Study
Received: 28-Oct-2021 / Editor assigned: 01-Jan-1970 / Reviewed: 01-Jan-1970 / Revised: 01-Jan-1970 / Accepted Date: 23-Nov-2021 / Published Date: 30-Nov-2021 DOI: 10.4172/2165-7904.1000471
Abstract
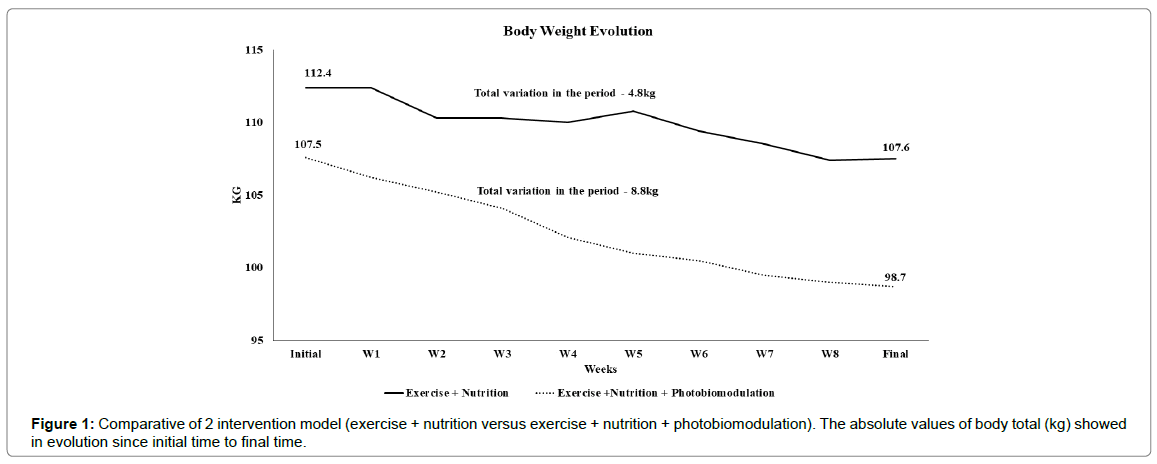
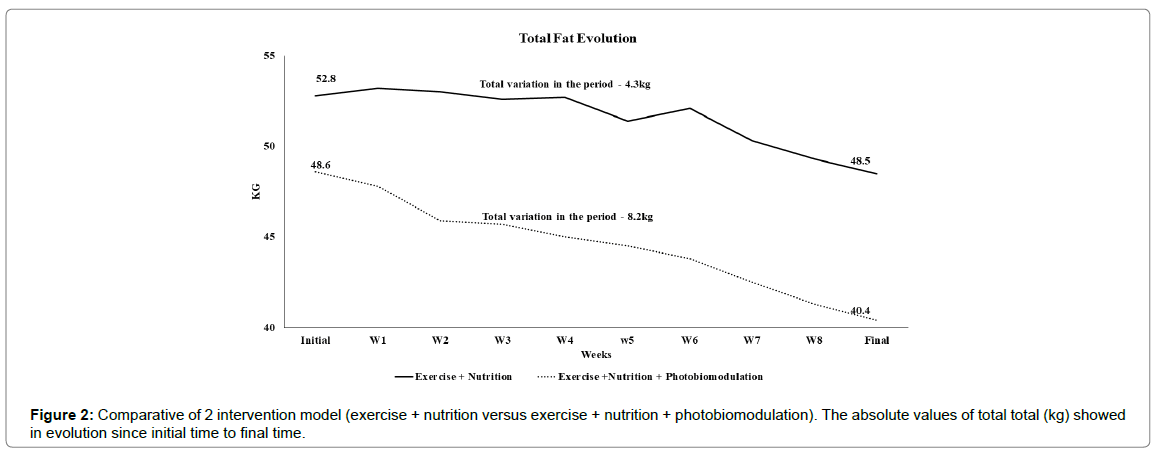
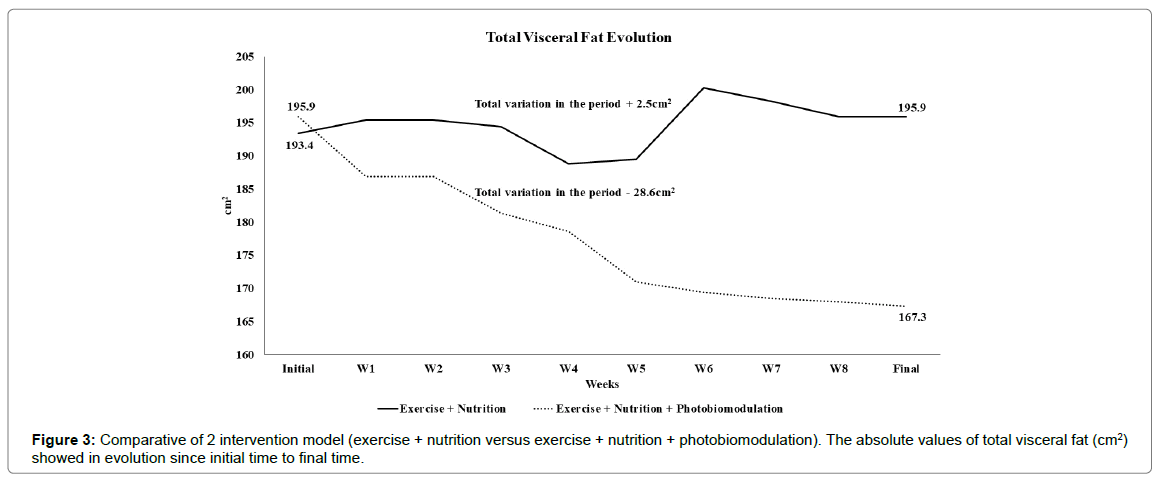
Excess body weight is a public health problem causing overweight and obesity, with the main characteristic of increasing body fat. Current non-pharmacological and non-invasive treatments prioritize negative energy balance through physical exercise and nutrition education. Over the years, it has been established that the association of traditional therapy (exercise and nutrition) together with photobiomodulation enhances the reduction of body fat. The aim of this study was to evaluate the action of photobiomodulation in a patient undergoing 8 weeks of traditional therapy and 8 weeks of traditional therapy associated with photobiomodulation, evaluating anthropometry, lipid profile and glycemic/insulin profile. The exercise protocol defined for the study included aerobic exercises (30 minutes) and resistance exercises (30 minutes), lasting 8 weeks, 3 times a week, with Nutritional Intervention. The photobiomodulation was always performed after physical exercise sessions in the anterior (abdominal and quadriceps) and posterior region (gluteus and biceps femoris) for 8 minutes per region. Comparison results of traditional versus combined therapy show respectively: body metabolic rate 0.54 and 5.38 body weight -4.8 kg and -8.8 kg, body fat 3.53% and 9.02%, Total fat 8.86% and 20.3%, visceral fat 1.27% and 17.8%, trunk fat 0.79% and 17.6%, right arm fat 12.5% and 37.1%, left arm fat 14.6% and 37.1%, right leg fat 13.2% and 21.6%, left leg fat of 13.4% and 23.7%. The lipid, glycemic/insulin profile showed the same pattern of reduction. Our study shows a wide anthropometric, lipid, glycemic and insulin reduction, when observing the combined action of photobiomodulation with traditional therapy in relation to the singular action of traditional therapy, allowing that in a period of only 8 weeks it is possible to restore the quality of life of the patient. patient, in a non-pharmacological and non-invasive way.
Keywords: Photobiomodulation; Body Weight; Visceral Fat; Serum Lipids; Metabolic Rehabilitation; Exercise
Introduction
Excess body weight is a public health problem both in Brazil and worldwide, causing overweight and obesity, which is called chronic subclinical inflammatory disease [1]. As the main characteristic, the increase in body weight brings with it an increase in total body fat, especially visceral fat, responsible for the emergence of numerous diseases called comorbidities [2,3]. Thus, conditions such as severe changes in the lipid profile, insulin resistance, type 2 diabetes mellitus and cardiovascular diseases are some of the diseases that occur through the inflammatory process resulting from the increase in body weight [4,5].
Currently, treatments for non-pharmacological and non-invasive conditions are aimed at a negative energy balance, where through the use of the most diverse physical exercise protocols, aiming at caloric expenditure and the use of nutritional education, allowing the reduction of excessive caloric intake [2,6-8], it is possible to reduce body weight. Over the years, our research group has carried out several studies that have made it possible to transfer knowledge from experimental studies [9-12] to clinical studies [6,8,13-18], establishing not only as viable, but a concrete possibility of associating traditional non-pharmacological therapy (exercise and nutrition) with photobiomodulation technology, enhancing the metabolic action to reduce body fat. In this context, it was found that the association of photobiomodulation with traditional non-pharmacological and non-invasive therapies allows a reduction in anthropometric parameters such as body weight, total and visceral fat, as well as an improvement in the lipid profile, glycemic and insulin status, thus reversing dyslipidemia, liver disorders and thus reducing cardiovascular risks [6,8-18].
The aim of this study was to evaluate the action of photobiomodulation in a patient undergoing 8 weeks of traditional therapy (exercise+nutrition) and 8 weeks undergoing traditional therapy associated with photobiomodulation (exercise+nutrition+ph otobiomodulation), evaluating anthropometric data, lipid profile and glycemic/insulin profile, thus allowing to assess the action of light on the patient’s metabolic evolution.
Materials And Methods
Ethics and Volunteer: This study was carried out by the Institute of Physics of São Carlos, University of São Paulo and approved by ethics committee on human research at Federal University of São Carlos - UFSCar C.A.A.E 13956313.7.0000.5504 and Clinical Trials.gov (231,286). For the study, an obese man was selected. Inclusion criteria were: body mass index between 30 and 40 kg/m2, aged between 20 and 40 years old. Exclusion criteria were: use of cortisone, anti-epileptic drugs, history of kidney disease, alcohol consumption, smoking. The study had two phases: Phase 1 - period of 8 weeks, where the volunteer was submitted to nutritional re-education action and a physical exercise program. Phase 2 - period of 8 weeks, where the volunteer was submitted to nutritional reeducation action, physical exercise program and photobiomodulation. Between the phases, there was an interval of 30 days. At each stage of treatment, evaluations were carried out in two stages, the initial stage and the final stage.
Physical Exercise Program: The exercise protocol defined for the study included aerobic exercises (30 minutes) and resistance exercises (30 minutes), lasting 8 weeks, 3 times a week. Aerobic exercise was performed on a treadmill (Pro Fitness AP8500 Plus), with maximum heart rate intensity between 70 and 85% (previously established in a submaximal test on a treadmill). Resistance training was performed by performing specific exercises for the main muscle groups: bench press (Biceps, Triceps, Pectorals Major and Rectus Abdominals), lat pull-down (Biceps, Teres Major and Latissimus Dorsi), Straight- Bar Cable Curl (Biceps), triceps pushdowns (Triceps), hamstring curls (Semitendinosus, Biceps Femoris and Semimembranosus), calf raises (Gastrocnemius), leg presses and sit-ups (Gluteus Maximus, Quadriceps Femoris, and Gastrocnemius). In each session, there was a progressive adjustment of the training loads, according to individual capacity, using the inversion of volume and system intensity in relation to number of repetitions, ranging from 6, 12 and 20 repetitions in three sets and conducted using maximal repetitions (Rm) [10.23.27]. This model of training was conducted based on the guidelines of the American College of Sports Medicine [7].
Nutritional Intervention: Nutritional lectures were held to adjust caloric intake, as well as not to drink alcoholic beverages. The assessment of usual food consumption was performed through a threeday food record and analyzed via AVANUTRI software.
Photobiomodulation: The action of photobiomodulation was always performed after physical exercise sessions. The laser emitters were fixed perpendicularly to the skin and positioned in the anterior and posterior region for 8 minutes per region, being in the anterior region (abdominal and quadriceps) and in the posterior region (gluteus and biceps femoris). The parameters used were: Ga-Al-As Semiconductor Diode Laser, wavelength 808 nm, 64 emitters in 4 plates (16 emitters per plate), diameter of spot in horizontal 0.3692 cm/vertical 0.0582 cm, area of spot of 0.0169 m2, output power of 100 mW, irradiance of 6.0 W/cm2, radiant energy 96J, total radiant energy delivered 147,456J (all 24 sessions, 3 times per week). To minimize the psychological bias, the transmitters were turned off in phase 1 and turned on in phase 2, without the patient’s knowledge.
Anthropometry and body composition: The voluntary was weighed and height measurements obtained (light clothes and no shoes) using an electronic scale. The body composition and anthropometrics parameters used in this study were: body mass (kg), body mass index (kg/m2), lean muscle mass (kg), total skeletal muscle mass (kg), Basal metabolic rate (kcal), body activity rate (kcal), total fat mass (kg), percentage of fat (%), fat mass of right arm (kg), fat mass of left arm (kg), fat mass of trunk (kg), fat mass of right leg (kg), fat mass of left leg (kg), visceral body fat (cm2). We used the bioelectrical impedance analysis (BIA) device to measure the change in impedance in body tissues by sending detectable electrical signals through the body. The BIA device use this is study was the In Body 720 (Biospace Co. Ltd.; Seul, Korea), which uses six frequencies (1,5,50,250,500 and 1,000 kHz). The body mass index (BMI) was calculated by body mass (Kg) dividing stature (m2).
Serum Analysis: The blood samples were collected after 12 hours overnight. The concentrations of glucose, insulin, lipid profile were analyzed with methods for in vitro diagnostic, specific for each measurement, performed in the specialized clinical laboratory. Insulin sensitivity was assessed using the homeostasis model assessment IR (insulin resistance) index (HOMA-IR).
Body Metabolic Progress and Delta (Δ): The development of a quantification method to measure the metabolis through the action of a certain therapy transcends only the use of the basal metabolic rate. Thus, the use of bioelectrical bio impedance, body mass (kg), skeletal muscle mass (kg) and basal metabolic rate (kcal) variables were organized in order to allow a more accurate analysis of body metabolic progress. Thus, as the basal metabolic rate is considered the basal amount of calories for the maintenance of basal body functions and skeletal muscle, in na amount and functionality, determining the variation of the basal metabolic rate [6], we propose:
“Body metabolic progress (kcal)=[body mass (kg)/basal metabolic rate (kcal)] × skeletal muscle mass (kg)”
In addition, as a way to normalize the data, a percentage form of Delta [6] was used, expressed in:
“Delta Value (Δ)=(Initial value - Final value) / Initial value × (100)”
Results
Table 1 shows the muscle and metabolic body composition variables, compared in the periods involving traditional therapies (Exercise+Nutrition) and those associated with Photobiomodulation (Exercise+Nutrition+Photobiomodulation). We observed in the period of traditional therapies the increase (delta) of the variables Skeletal Mass Muscle (1.5), Body Metabolic Rate (0.54) and Body Metabolic Progress (5.38), while in the period when it was associated with photobiomodulation, we observed the variables Skeletal Mass Muscle (-0.91), Body Metabolic Rate (-0.98) and Body Metabolic Progress (6.52).
| Exercise + Nutrition | Exercise + Nutrition + Photobiomodulation | |||||
|---|---|---|---|---|---|---|
| Initial | Final | Δ | Initial | Final | Δ | |
| Skeletal Mass Muscle (kg) | 32.7 | 33.2 | 1.5 | 33.2 | 32.9 | -0.91 |
| Body Metabolic Rate (Kcal) | 1634 | 1643 | 0.54 | 1644 | 1628 | -0.98 |
| Body Metabolic Progress (kcal) | 480.07 | 507.42 | 5.38 | 507.26 | 542.67 | 6.52 |
Table 1: Comparative of body muscle and metabolic composition in different period of treatment.
Figure 1 shows the evolution of body weight in the 8-week periods involving the action of exercise+nutrition in relation to the 8-week period involving the action of exercise+nutrition+ photobiomodulation. The reduction in the first period (-4.8 kg) in relation to the reduction in the second period (-8.8 kg) is shown.
Table 2 represents the reduction in body, total fat depots and limbs, comparing the period of treatment without the action of light in relation to the period composed by the association of photobiomodulation. The comparison shows percentage reductions in body fat of 3.53% and 9.02%, Total fat of 8.86% and 20.3%, visceral fat of 1.27% and 17.8%, and trunk fat 0.79% and 17.6%, right arm fat of 12.5% and 37.1%, left arm fat of 14.6% and 37.1%, right leg fat of 13.2% and 21.6% and in the left leg fat of 13.4% and 23.7%, respectively for the intervention period that includes exercise + nutrition therapies and exercise +nutrition and photobiomodulation therapies.
| Exercise + Nutrition | Exercise + Nutrition + Photobiomodulation |
|
|---|---|---|
| Body Weight Fat | -3.53 | -9.02 |
| Total Fat | -8.86 | -20.3 |
| Visceral Fat | -1.27 | -17.8 |
| Trunk Fat | -0.79 | -17.6 |
| Right Arm Fat | -12.5 | -37.1 |
| Left Arm Fat | -14.6 | -37.1 |
| Right Leg Fat | -13.2 | -21.6 |
| Left Leg Fat | -13.4 | -23.7 |
| Table 2-Comparative of 2 intervention model (exercise + nutrition versus exercise + nutrition + photobiomodulation). The values are expressed in delta (Δ). | ||
Table 2: Comparison of fat reduction between traditional therapy and the associated use of photobiomodulation in 8-week period.
Figure 2 shows the evolution of the patient’s total fat over the two intervention periods. It is possible to observe that in the period that involved the traditional therapies there was a reduction of -4.3 kg of fat and that in the period that there was the association of photobiomodulation, there was a reduction of -8.2 kg of fat.
Figure 3 illustrates the evolution of total visceral fat in the periods of traditional therapy (exercise + nutrition) and association of photobiomodulation (exercise + nutrition + photobiomodulation). A brief increase in the period without the use of photobiomodulation is observed, of 2.5 cm2, while in the period of 8 weeks with the use of photobiomodulation, there was a reduction of 128.6 cm2.
Table 3 shows the variation in lipid, insulin and glucose profiles when comparing the periods of traditional therapy (exercise + nutrition) and traditional therapy associated with photobiomodulation. It is possible to observe in the delta of lipid profile, the variations of total cholesterol -16.89 and -56.78, HDL-c -2.27 and -47.06, LDL-c -19.77 and -67.65, VLDL -38.89 and -31.25 and triglycerides -35.16 and - 31.25, respectively for the 8-week period of traditional therapy and traditional therapy associated with photobiomodulation. When we look at insulin and blood glucose, the variations show a delta of -65.17 and -32.5 for insulin and 3.26 and -31.25 for blood glucose, respectively for the exercise+nutrition versus exercise+nutrition+photobiomodula tion periods.
| Exercise + Nutrition | Exercise + Nutrition + Photobiomodulation | |||||
|---|---|---|---|---|---|---|
| Initial | Final | Δ | Initial | Final | Δ | |
| Total Cholesterol (mg/dL) | 173 | 148 | -16.89 | 185 | 118 | -56.78 |
| HDL-c (mg/dL) | 45 | 34 | -2.27 | 50 | 34 | -47.06 |
| LDL-c (mg/dL) | 103 | 86 | -19.77 | 114 | 68 | -67.65 |
| VLDL (mg/dL) | 25 | 18 | -38.89 | 21 | 16 | -31.25 |
| Triglycerides (mg/dL) | 123 | 91 | -35.16 | 105 | 80 | -31.25 |
| Insulin (uU/ml) | 14.7 | 8.9 | -65.17 | 10.6 | 8 | -32.5 |
| Blood Glucose (mg/dL) | 89 | 92 | 3.26 | 88 | 75 | -17.3 |
Table 3: Comparison of lipid profile, insulin and glucose in different periods of treatment
Table 4 provides a comparison between the water, intracellular, extracellular and total contents, in the period of 8 weeks where the patient was submitted to the traditional exercise + nutrition therapy and in the period of 8 weeks where the patient was submitted to the protocol that covered exercise + nutrition + photobiomodulation. It is possible to observe the reduction of variables when observing traditional therapy in relation to therapy associated with photobiomodulation, with the reduction of delta values for intracellular water 1.48 and -1.12, extracellular water -.124 and -2.53, and total water 0.46 and - 1.64, respectively for traditional therapy versus therapy associated with photobiomodulation.
| Exercise + Nutrition | Exercise + Nutrition + Photobiomodulation | |||||
|---|---|---|---|---|---|---|
| Initial | Final | Δ | Initial | Final | Δ | |
| Intracellular water (L) | 26.6 | 27 | 1.48 | 27 | 26.7 | -1.12 |
| Extracellular water (L) | 16.3 | 16.1 | -1.24 | 16.2 | 15,8 | -2.53 |
| Total water (L) | 42.9 | 43.1 | 0.46 | 43.2 | 42.5 | -1.64 |
Table 4: Comparison of intracellular water, extracellular water and total water in different periods of treatment
Discussion
The constant increase in obesity cases in the world [2,3,19] conditions the need for new non-invasive and non-pharmacological methods that allow the process of weight loss in a more optimized way, without harming health and, therefore, a healthy return to quality of life.
The action of photobiomodulation, whether by the use of lasers or LEDs, is well defined and established in the literature [20-22] for the most diverse therapeutic actions and treatments of diseases [23-27] among them metabolic rehabilitation for weight loss [6,9,11,15-18]. In the latter, studies point to increased metabolism, measured via the Citrate Synthase enzyme [10], allowing for an increase in metabolic demand.
Our present study shows the positive action of photobiomodulation on metabolism (Table 1), allowing the body metabolic progress (BMP) [6] to show comparison values between traditional therapy (5.38) and combined therapy with photobiomodulation (6.52), clearly pointing to a more active metabolism when associated with photobiomodulation. This statement is corroborated by the results of higher values found with the Citrate Synthase enzyme in rats submitted to the exercise and photobiomodulation protocol, showing positive the combined action of exercise and photobiomodulation in an animal model [9-12]. The body Metabolic Progress (BMP) proves to be reliable since the variation seems more adequate due to the fact that the variables body weight, basal metabolic rate and skeletal muscle mass are directly interlinked [6]. Thus, due to the possibility of greater production of ATP, promoted by the combined action between traditional therapy and photobiomodulation, the evolution of body weight shown in Figure 1 shows the reduction of 4 kg of extra fat, when compared to the period of traditional therapy, showing a more intense metabolic demand for energy substrate. The same results are observed in experimental [10] and clinical [6,15-18] studies. It is possible to observe the various fat deposits being more intensely reduced when analyzing table 2, showing that visceral fat is directly reduced, which directly impacts the emergence of diseases associated with overweight and obesity [2.28]. Figure 2 shows the evolution of total body fat reduction, showing the reduction obtained during the traditional therapy period associated with -4.3 kg photobiomodulation in relation to the traditional therapy intervention time period. This result is also confirmed experimentally [9, 10] and clinically [6,15,16] in previous studies from our group.
The due importance in the observation of figure 3 is due to the marked reduction of visceral fat when the combined action of photobiomodulation is used, obtaining approximately 14.5% greater reduction. This result is in line with the reduction in visceral fat shown in Table 2, but allows the monitoring of evolution over time. Its reduction makes it possible to envision an easier control of diseases directly linked to the increase in visceral fat, such as type 2 diabetes mellitus or even allow for a reduction in the risk of cardiovascular diseases [2,28].
The constant need for energetic substrate primarily impacts the levels of serum lipids [9,15,16], with the greatest reduction being directly pointed out in table 3, when observing the values of the action conjugated with photobiomodulation. These reduction values are supported by the greater metabolic demand, being metabolized [6,9]. In this process, lipases are modulated [29], promoting the hydrolysis of the triglyceride molecule, providing free fatty acid and glycerol, which are then metabolized via beta-oxidation/re-esterification into VLDL and via gluconeogenesis, forming hepatic and muscle glycogen [6, 9,10]. Still, the reduction in insulin and blood glucose values are a reflection of the high energy demand and the high reduction in visceral fat, a factor directly related to insulin variations [6].
Thus, as a consolidated hypothesis in previous studies, the action of laser or LED as a photobiomodulator effect causes the modulation of the hormone-sensitive lipase enzymes and lipoprotein lipase [29], allowing the hydrolysis of triglyceride molecules, both in the circulating environment and stored in fat deposits in adipocytes [6,9,10]. It is believed that, firstly, the circulating environment (circulating lipids) is affected, with the subsequent need for action in the intracellular environment (lipids stored in adipocytes), to absorb the metabolic demand established due to the energy consumption promoted by the combined action between the traditional therapy and photobiomodulation, positively influencing the krebs cycle. Thus, triglyceride molecules are metabolized via beta-oxidation, generating Acetyl-CoA, allowing action via the Krebs cycle or re-esterified in VLDL. Glycerol, in turn, is taken to the gluconeogenesis pathway, promoting the formation of hepatic and muscle glycogen, corroborated by [6] and [9], in an experimental and clinical environment, respectively. Thus, the reduction of fat deposits are markedly reduced, as observed in the present study and previous studies [6,9,10,15,16].
The reduction of aqueous, intracellular, extracellular and total media (Table 4), points to a framework of systemic organic homeostasis, strengthened by the use of intracellular water in reaction of the electron transport chain, due to the greater metabolic demand and energy production due to exercise synergy and photobiomodulation [20,21]. Furthermore, the increased regulation provides greater extracellular and total water regulation in these media [30]. Thus, the metabolic rehabilitation promoted by the synergy between traditional therapy and photobiomodulation proves to be effective in an 8-week intervention period, allowing an efficient result in a reduced time of action.
Conclusion
The need for new non-invasive and non-pharmacological methods to restore quality of life in relation to overweight and obesity is increasingly important. Our study shows not only the reduction of body weight, but the reduction of all fat deposits, as well as the regularization of the lipid profile, glycemic/insulin status and total, intracellular and extracellular composition of body water, allowing for a period of just 8 weeks it is possible to restore the patient’s quality of life, without harm. The importance of expressive results in shorter periods of time are necessary as intervention instruments that prevent the advancement of diseases related to excess body fat from taking hold and making these diseases a high cost to public health and life.
References
- Carnier J, Sanches PDL, da Silva PL, de Piano A, Tock LR, et al. (2012) Obese adolescents with eating disorders: Analysis of metabolic and inflammatory states. Physiol Behav 105: 175-80.
- Tchernof A, Després J (2013) Pathophysiology of human visceral obesity: an update. Physiol Rev 93: 359-404.
- Gruzdeva O, Borodkina D, Uchasova E, Dyleva Y, Barbash O (2018) Localization of fat depots and cardiovascular risk. Lipids Health Dis 17: 1-9.
- Ueno T, Sugawara H, Sujaku K, Hashimoto O, Tsuji R, et al. (1997) Therapeutic effects of restricted diet and exercise in obese patients with fatty liver. J Hepatol 27: 103-7.
- Grant-Guimaraes J, Feinstein R, Laber E, Kosoy J (2016) Childhood overweight and obesity. Gastroenterol Clin North Am 45: 715-28.
- De Aquino Junior AE, Carbinatto FM, Moriyama LT, Bagnato VS (2018) Regression of Non-Alcoholic Fatty Liver by Metabolic Reduction: Phototherapy in Association with Aerobic Plus Resistance Training in Obese Man – A Pilot Study. J Obes Weight Loss Ther 8:1-7.
- Joseph E Donnelly, Steven N Blair, John M Jakicic, Melinda M Manore, Janet W Rankin, et al. (2009) American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc 41:459-71.
- De Piano A, de Mello MT, Sanches PDL, da Silva PL, Campos RMS, et al. (2012) Long-term effects of aerobic plus resistance training on the adipokines and neuropeptides in nonalcoholic fatty liver disease obese adolescents. Eur J Gastroenterol Hepatol 24: 1313-24.
- Aquino AE Jr, Sene-Fiorese M, Paolillo FR, Duarte FO, Oishi JC, et al. (2013) Low-level laser therapy (LLLT) combined with swimming training improved the lipid profile in rats fed with high-fat diet. Lasers Med Sci 28: 1271-80.
- Aquino AE Jr, Sene-Fiorese M, Castro CA, Duarte FO, Oishi JC, et al. (2015) Can low-level laser therapy when associated to exercise decrease adipocyte area ? J Photochem Photobiol B 149: 21-26.
- De Aquino AE Jr, de Castro CA, Ana da Silva K, Carbinatto FM, Anibal FF, et al. (2016) Low-level laser therapy promotes decrease in inflammatory process in obese trained rats. J Community Med Health 6: 1-5.
- De Aquino AE Jr, Carbinatto FM, de Castro CA, Venturini FP, Parizotto NA, et al. (2017) Photobiomodulation decrease antioxidantenzymes activity in obese trained rats. Bioenergetics 6: 1- 5.
- Paolillo FR, Milan JC, Aniceto IV, Barreto SG, Rebelatto JR, et al. (2011) Effects of Infrared-LED illumination applied during high-intensity treadmill training in postmenopausal women. Photomed Laser Surg 29: 639-645.
- Paolillo FR, Borghi-Silva A, Parizotto NA, Kurachi C, Bagnato VS (2011) New treatment of cellulite with infrared-LED illumination applied during high-intensity treadmill training. J Cosmet Laser Ther 13: 166-171.
- Duarte FO, Sene-Fiorese M, de Aquino Junior AE, da Silveira Campos RM, Masquio DC, et al. (2015) Can low-level laser therapy (LLLT) associated with an aerobic plus resistance training change the cardiometabolic risk in obese women? A placebo-controlled clinical trial. J Photochem Photobiol B 153: 103-110.
- Sene-Fiorese M, Duarte FO, de Aquino Junior AE, Campos RM, Masquio DC, et al. (2015) The potential of phototherapy to reduce body fat, insulin resistance and “metabolic inflexibility†related to obesity in women undergoing weight loss treatment. Lasers Surg Med 47: 634-642.
- Da Silveira Campos RM, Damaso AR, Masquio DC, Aquino AE Jr, Sene-Fiorese M, et al. (2015) Low-level laser therapy (LLLT) associated with aerobic plus resistance training to improve inflammatory biomarkers in obese adults. Lasers Med Sci 30: 1553-1563.
- Da Silveira Campos RM, Damaso AR, Masquio DC, Duarte FO, Sene-Fiorese M, et al. (2018) The effects of exercise training associated with low-level laser therapy on biomakers of adipose tissue transdifferentiation in obse women. Lasers Med Sci 33: 1245-1254.
- Huang H, Yan Z, Chen Y, Liu F. (2016) A Social contagius modelo f the obesity epidemic. Sci Rep 6: 37961.
- Karu TI, Pyatibrat LV (2003) Photobiological modulation of cell attachment via cytochomec oxidase. Photochem. Photobiol Sci 3: p211-216.
- Karu TI, Pyatibrat LV, Natalia IA (2005) Cellular effects of low power laser therapy can be mediated by nitric oxide. Lasers in Surgery and Medicine 36: 307-314.
- Vladimov YA, Osipov AN, Klebanov GI (2004) Photobiological principles of therapeutic applications of laser radiation. Biochemistry 69: p81-90.
- De Souza Simão ML, Fernandes AC, Ferreira KR, De Oliveira LS, Mário EG, et al. (2019) Comparison between the Singular Action and the Synergistic Action of Therapeutic Resources in the Treatment of Knee Osteoarthrosis in Women: A Blind and Randomized Study. J Nov Physiother 9: 2.
- Junior AEA, Carbinatto FM, Franco DM, Bruno JSA, Simão MLS et al. (2020). The Laser and Ultrasound: The Ultra Laser like Efficient Treatment to Fibromyalgia by Palms of Hands–Comparative Study. J Nov Physiother, 11: 2.
- Tamae PE, Santos AVD, Simão MLS, Canelada ACN, Zampieri KR, et al. (2020) Can the Associated Use of Negative Pressure and Laser Therapy Be A New and Efficient Treatment for Parkinson's Pain? A Comparative Study. J Alzheimers Dis Parkinsonism 10: 2.
- Panhóca VH, Lopes LB, Paolillo FR, Bagnato VS (2018) Treatment of temporomandibular disorder using synergistic laser and ultrasound application. Oral Health Dent Manag, 17: 1-5.
- Panhóca VH, Nogueira MS, Bagnato VS (2020) Treatment of facial nerve palsies with laser and endermotherapy: a report of two cases. Laser Phys Lett 18: 015601.
- Neeland IJ, Ross R, Després J, Matsuzawa Y, Yamashita S, et al. (2019) Visceral and ectopic fat, atherosclerosis, and cardiometabolic disease: a position statement. Lancet Diabetes Endocrinol 7: 715-725.
- Azeemi ST, Raza SM, Masoom Y (2008) Colors as catalysts in enzymatic reactions. J Acupunct Meridian Stud 1: 139-142.
- Rakova N, Kitada K, Lerchl K, Dahlmann A, Birukov A, et al. (2017) Increased salt consumption induces body water conservation and decreases fluid intake. J Clin Invest. 127: 1932-1943.
Citation: Junior AEA, Carbinatto FM, Bagnato VS (2021) Metabolic Rehabilitation: Body Homeostasis through the Action of Photobiomodulation in Weight Loss – a Comparative Study. J Obes Weight Loss Ther 11: 471. DOI: 10.4172/2165-7904.1000471
Copyright: © 2021 Junior AEA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3184
- [From(publication date): 0-2021 - Dec 21, 2025]
- Breakdown by view type
- HTML page views: 2597
- PDF downloads: 587