Modified Method of Tracheostomy in ICU Patients in âÃâ¬ÃÅHeratsiâÃâ¬Ã No.1 Hospital
Received: 13-Dec-2017 / Accepted Date: 17-Jan-2018 / Published Date: 24-Jan-2018 DOI: 10.4172/2376-032X.1000226
Abstract
Long-term mechanical ventilation is the most common situation for which tracheostomy is indicated for patients in intensive care units (ICUs). The ideal techniques for tracheostomy have been topics of considerable debate. The new modified method of surgical tracheostomy is presented with compare of the classical surgical tracheostomy (CST) and PDT techniques.
Clinical trial with external control was providing in “Heratsi” No.1 Hospital Complex Intensive Care Unit (ICU). The study was carried out on 65 patients who underwent modified method of surgical tracheostomy by Poghosyan (Main Group) and Control Group was created collecting clinical data from medical records of 53 patients who underwent the Classical Surgical Tracheostomy (CST) (Group B), and 28 patients who underwent the Percutaneus DilatationTracheostomy (PDT) (Group C). Early and intermediate complications of each method of tracheostomy were analyzed for results interpretation. Group A (PMST) had less early complications- 1.5% (1 death because of apnoea) compare to Group B (CST) 49% (26 early complications including 2 deaths) and Group C (PDT)-25% (7 complications without death).
There was no tracheostomy related mortality in intermediate stage of post-operation care in any group. Also there was less intermediate complications rate in PMST Group compare to CST Group (1 vs. 19) and PDT Group (1 vs. 5).
In our study PMST demonstrated less intraoperative and intermediate complications in compare with CST and PDT. As an open surgical method it could be used in cases, when PDT is contraindicated, but in compare with CST it is minimal invasive, without any incision of subcutaneous soft tissues and with aesthetic results similar to PDT.
Keywords: Tracheostomy; ICU; Stroke; Percutaneus Dilatational Tracheostomy
Introduction
Tracheostomy is a surgical procedure routinely done in critically ill patients requiring prolonged mechanical ventilatory support.
It has a number of advantages including improved lung mechanics, easier oral hygiene, diminished nociceptive stimuli on the larynx or trachea, decreased need for sedatives, enhanced communication, and the fact that the head and neck are free of equipment [1-3].
Tracheostomy might facilitate weaning by reducing dead space and airway resistance, and by improving secretion clearance [4]. It has been associated with improved mobility and decreased length of intensive care stay [5-7].
However tracheotomy also has adverse effects like procedure-related complications and later cosmetic concerns [8-10].
Timing of tracheostomy should be personalized for the patients after taking into account the risks and benefits of this procedure [11].
Tracheostomies can be performed through with an open or percutaneous technique. Both open surgical tracheostomy (ST) and percutaneous dilatational tracheostomy (PDT) are methods used to perform tracheostomy in select individuals.
The best technique for performing tracheostomy remains a matter of debate [1,3,12,13]. Each method has his advantages and disadvantages.
The determining factors in deciding whether to use an ST or PDT in a particular situation depends on patient anatomical and physiological factors and as well on surgeon experiences and prefers.
The aim of this study is to present the modified method of surgical tracheostomy with compare of the classical surgical tracheostomy (CST) and PDT techniques to reduce surgical complications.
Materials and Methods
Clinical trial with external control was providing in “Heratsi” No.1 Hospital Complex Intensive Care Unit (ICU). From May 2013 to July 2017 we performed 65 tracheostomies using Modified Surgical Tracheostomy Technique by Poghosyan (PMST) and these patients formed the Main Group A.
The Control Group was created collecting clinical data from medical records of 53 patients who underwent the Classical Surgical Tracheostomy (CST) (Group B), and 28 patients who underwent the Percutaneus DilatationTracheostomy (PDT) from September 2006 to April 2012 (Group C).
From 65 Main Group patients 25 were females and 40 males with ages from 20 to 82. Four tracheostomies were performing by urgent indications and 61 patients requiring prolonged mechanical ventilation in ICU.
Seventeen patients (27.9%) patients were undergoing treatment because of hemorrhagic stroke, 16 (26.2%) patients for respiratory failure due to pulmonary diseases, 12(19.7%) for different traumatic injuries and 16 (26.2%) patients for other diagnosis.
Timing of tracheostomy in ICU patient with mechanical ventilation was 9.8 ± 3 days.
In 4 patients with head and neck traumatic injuries, complicated by asphyxia PMST tracheostomy was performed immediately under local anesthesia in Emergency room and in one patient on mechanical ventilation in ICU PMST was performed bedside under local anesthesia.
In other cases PMST tracheostomy was performed under general anesthesia in operation room.
From 61 patients on prolonged mechanical ventilation in ICU 30 (49.1%) have anatomical disadvantages for PDT (short and fatty neck or morbidly obese patients with body mass index greater than 40 kg/m2) and 34 (55.7%) patients undertook anticoagulants.
PMST operation technique
Patient is positioned supine with a bolster placed transversely behind the shoulders to extend the neck and provide optimal exposure.
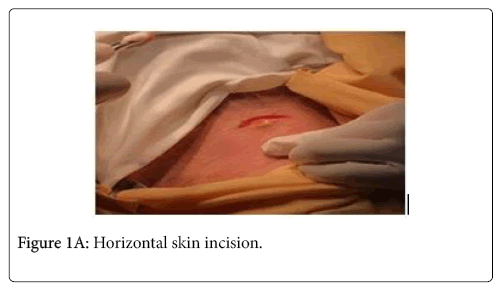
A 2-2.5 cm horizontal skin incision is made above 1.5 cm inferiorly of cricoids cartilage (Figure 1A).
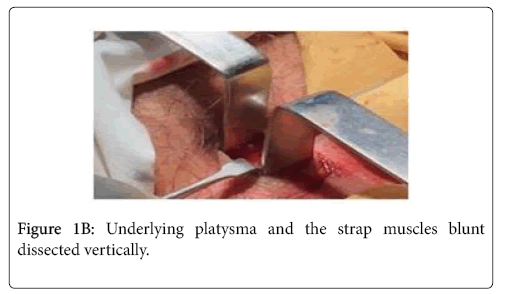
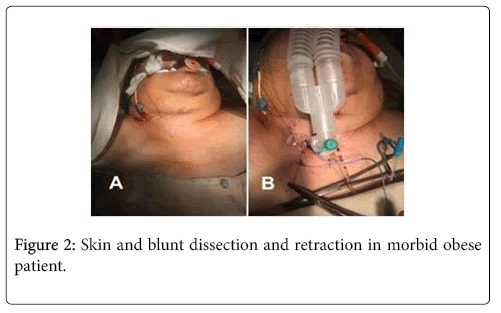
After skin division, underlying platysma and the strap muscles blunt dissected vertically by Mosquito hemostats and laterally retracted by the Senn-Miller retractors (Figure 1B).
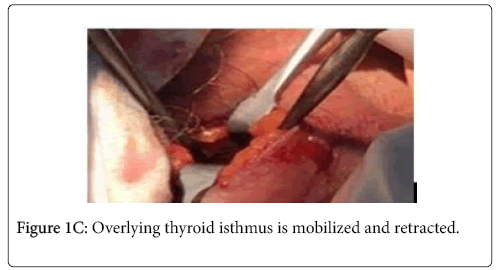
In some cases with fatty and short neck aspiration probe suggests. Overlying thyroid isthmus is mobilized and retracted inferiorly by narrow Henahan retractor or periosteal elevators (Figure 1C).
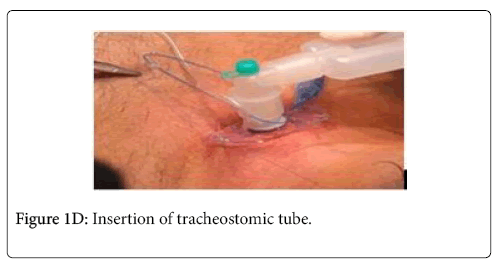
A cricoid hook is used to provide trachea upward traction for improving exposure. Once hemostasis and exposure are optimized, the second-third tracheal rings is incised vertically with a scalpel and tracheal entrance dilated by Trousseau tracheal dilator. Tracheostomic tube inserted after the intubation tube is removed (Figure 1D).
No skin sutures are needed for wound closure as it is enough small and Betadine dressing is put under tube flange.
So, no any incisions are doing except skin and only blunt dissection and retraction is performing under visual control even in morbid obesity patients (Figure 2).
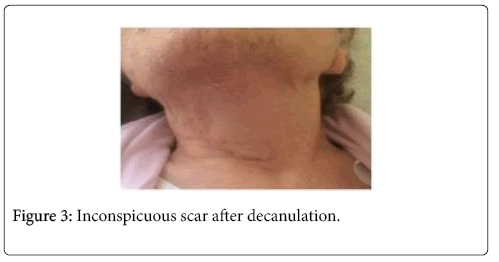
Depending on neck anatomy, duration of operation ranged from 5 to 17 min (average duration 11 ± 2 min). An inconspicuous scar is observed after decanulation (Figure 3).
Comparison between tracheostomy operation techniques in different groups has shown in Table 1.
| Surgical technique | Incision length | Soft tissue preparation | Visualization of anatomical structures | Average duration of operation | Special equipment (bronchoscope) necessity | Post decanulation scarring |
|---|---|---|---|---|---|---|
| PMST | 2-2.5 cm | Blunt dissection only | + | 11 ± 2 min | - | Minimal |
| CST | 4.5-5 cm | Incision and blunt dissection | + | 32 ± 4 min | - | Rough scarring, especially in cases of vertical skin incision |
| PDT | 1-1.5 cm | Dilatation | - | 14 ± 3 min | + | Minimal |
Table 1: Comparison between tracheostomy operation techniques in different groups.
Statistical analysis
Mean standard deviation and standard error were used to describe numerical data, for qualitative data rates and proportions were applied. For comparison of outcomes between groups was used Pearson’s chisquare test. In case of quantitative limitations, two-sided exact Fisher’ probability was used. In all cases results were considered statistically significant at p<0.05 value.
Results
For results interpretation we have analyzed early and intermediate complication of each method of tracheostomy. The results of early and intermediate complications have shown in Tables 2 and 3.
| Type of complication | Group A (PMST) | Group B (CST) | Group C (PDT) | |||
|---|---|---|---|---|---|---|
| n | Percentage % | n | Percentage % | n | Percentage % | |
| Haemorrhage | 0 | 14 | 26.40% | 3 | 10.70% | |
| Posterior tracheal wall injury | 0 | 0 | 1 | 3.60% | ||
| Paratracheal placement | 0 | 0 | 1 | 3,6% | ||
| Pneumothorax | 0 | 3 | 5.70% | 1 | 3.60% | |
| Cardiac arrest | 0 | 1 | 1.90% | 0 | ||
| Damage of other local structures | 0 | 6 | 11.30% | 0 | ||
| Apnoea | 1 | 1.60% | 1 | 0 | ||
| Other | 0 | 1 | 1.90% | 1 | 3.60% | |
Table 2: Early complications of tracheostomy.
| Type of complication | Group A (PMST) | Group B (CST) | Group C (PDT) | |||
|---|---|---|---|---|---|---|
| n | Percentage | n | Percentage % | n | Percentage % | |
| Late bleeding | 1 | 1.60% | 4 | 7.50% | 1 | 3.50% |
| Displacemet and dislodgement of the tube | 0 | 2 | 3.80% | 2 | 7.10% | |
| Surgical emphysema | 0 | 6 | 11.30% | 2 | 7.10% | |
| Pneumothorax | 0 | 4 | 7.50% | 1 | 3.50% | |
| Infection | 0 | 2 | 3.80% | 0 | ||
| Tracheoesophageal fistula | 0 | 1 | 1.90% | 0 | ||
Table 3: Intermediate complications of tracheostomy.
Based on the results obtained in the tables Group A (PMST) had less early complications 1.5% (1 death because of apnoea) compare to Group B (CST) 49% (total 26 early complications including 2 deaths) and Group C (PDT) 25% (7 complications without death). Statistically significant less number of hemorrhage was observed in PMST group (x2 =17.04, p<0.000), as well as damage of other local structures and surgical emphysema (Fisher’ exact coefficient =0.007).
There was no tracheostomy related mortality in intermediate stage of post operation care in any group. Also there was less intermediate complications rate in PMST Group compare to CST Group (1 vs. 19) and PDT Group (1 vs. 5).
Although there was no benefits in duration of manipulation in comparison with PDT method, but our suggested method is significantly shorter in comparison with CST (p<0.001).
Discussion
Tracheostomy is one of the most frequently performed procedures in the critically-ill patients, and is one of the cornerstones that help improve the lives of patients who are ventilator-dependent or have lost their native airway [2,8,14]. Complications from surgical procedures are common and must be taken into account when assessing the risks and benefits of a particular treatment approach [15]. The best technique for performing tracheostomy remains a matter of debate [13,16].
In most adult ICU patients requiring elective tracheostomy and without contraindications to percutaneous tracheostomy, it has been suggested that percutaneous dilatational tracheostomy (PDT) should be considered the procedure of choice, as it possible performance at the bedside, reduction of operating room costs, limiting patient travel, timing and improved healing [1,8]. However, the method contraindicated in patients with coagulopathy, thrombocytopenia, other risk factors for bleeding, inadequate surface landmarks, inability to tolerate hypoxemia or hypercarbia, need for proximal or distal extension tracheostomy, morbid obesity etc. [13,17]. In our experiences 49.1% of Main Group patients have anatomical disadvantages for PDT and 55.7% of same group patients undertook anticoagulants.
Halum et al. [18] performed multi-institution historical cohort study regarding tracheotomy complications from consecutive surgeries performed across eight participating institutions. Bleeding was identified as the most common early complication (2.6%). Perioperative tracheotomy complications are rare; however, the rate of death for all causes was high (22%) in this population. Percutaneous tracheotomy resulted in a significantly higher rate of postoperative bleeding (6.6%) than the open method (1.9%) (P<0.05). In our study there was no intraoperative or postoperative bleeding in Group A (PMST) in compare with CST (0 vs.18) and PDT Group (0 vs. 4). We perform only blunt vertical dissection after small horizontal skin incision PMST Group, which creates minimal bleeding.
Pneumothorax after tracheostomy is one of the most described complications, with an incidence as high as 17% in some reports [13]. We don’t have any case of pneumothorax in Group A (PMST) while there was describe 7 cases in CST Group and 2 in PDT Group.
From the damage of local structure more often thyroid damage has occurred, less- posterior tracheal wall injury with esophageal perforation. Due to the anatomic location of the thyroid directly anterior to the trachea, the gland is at risk of injury during both open and percutaneous tracheostomy procedures. An open tracheostomy offers the advantage of direct visualization and ability to cauterize, divide, and/or legate the thyroid isthmus as necessary for exposure of the trachea. Insufficient hemostasis at the time of the procedure may cause significant postoperative bleeding. However, with a percutaneous tracheostomy, there is no visualization of the thyroid gland [8,19]. By our methodic thyroid isthmus is mobilized and retracted inferiorly by narrow Henahan retractor or periosteal elevators. So we don’t use any incision or dissection of thyroid and thus prevent bleeding from thyroid and necessarily ligation. Surgical emphysema was the third more common tracheostomy complication in our study. Subcutaneous emphysema occur secondary to a disruption in the respiratory tract allowing air to freely leak into the contiguous subcutaneous spaces. As it relates to percutaneous tracheostomies, the rate of subcutaneous emphysema has been reported to be approximately 1.4% [8,20]. Six cases of surgical emphysema were observed in CST Group with and 2 cases in PDT Group as an intermediate complication. There was no any case of surgical emphysema in PMST Group
Apnoea was another complication observed in this study. This complication was encountered in 1 female patients suffering from cardiopulmonary insufficiency. Since of the tube tracheal insertion, bradycardia was observed with apnoea cardiac arrest. This was the only fatal case in Group A (PMST).
Infection occurred in 2 patients from Group B (CST). In PMST and PDT Groups tracheostomy carried through a small skin incision, thus no any sutures needs for wound closing. Absence of a large wound and sutures reduces the risk of postoperation infection.
Conclusion
Complications from tracheostomy are common and must be taken into account when assessing the risks and benefits of a surgical approach and method. In our study PMST demonstrated less intraoperative and intermediate complications in compare with CST and PDT. As an open surgical method it could be used in cases, when PDT is contraindicated, but in compare with CST it is minimal invasive, without any incision of subcutaneous soft tissues and with aesthetic results similar to PDT
References
- Cheung NH, Napolitano LM (2014) Tracheostomy: Epidemiology, indications, timing, technique, and outcomes. Respir Care Jun 59: 895-915.
- Freeman BD, Morris PE (2012) Tracheostomy practice in adults with acute respiratory failure. Crit Care Med 40: 2890-2896.
- De Leyn P, Bedert L, Delcroix M, Depuydt P, Lauwers G et al. (2007) Tracheotomy: Clinical review and guidelines. Eur J Cardiothorac Surg 32: 412-421.
- Sofi K, Wani T (2010) Effect of tracheostomy on pulmonary mechanics: An observational study. Saudi J Anaesth 4: 2-5.
- Bosel J (2014) Tracheostomy in stroke patients. Curr Treat Options Neurol 16: 274.
- Hosokawa K, Nishimura M, Egi M, Vincent JL (2015) Timing of tracheotomy in ICU patients: A systematic review of randomized controlled trials. Crit Care 19: 424.
- Engels PT, Bagshaw SM, Meier M, Brindley PG (2009) Tracheostomy: From insertion to decannulation. Can J Surg 52: 427-433
- Cipriano A, Mao ML, Hon HH, Daniel Vazquez D, Stawicki SP, et al. (2015) An overview of complications associated with open and percutaneous tracheostomy procedures. Int J Crit Illn Inj Sci 5: 179-188.
- Klemm E, Nowak AK (2017) Tracheotomy-related deaths. Dtsch Arztebl Int 114: 273-279.
- Rana S, Pendem S, Pogodzinski MS, Hubmayr RD, Gajic O (2005) Tracheostomy in critically ill patients. Mayo Clin Proc 80: 1632-1638.
- Longworth A, Veitch D, Gudibande S, Whitehouse T, Snelson C, et al. (2016) Tracheostomy in special groups of critically ill patients: Who, when, and where? Indian J Crit Care Med 20: 280-284.
- Andriolo BN, Andriolo RB, Saconato H, Atallah AN, Valente O (2015) Early versus late tracheostomy for critically ill patients. Cochrane Database Syst Rev 14: CD007271.
- Delaney A, Bagshaw SM, Nalos M (2006) Percutaneous dilatational tracheostomy versus surgical tracheostomy in critically ill patients: A systematic review and meta-analysis. Crit Care 10: R55.
- Heffner JE, Miller KS, Sahn SA (1986) Tracheostomy in the intensive care unit. Part 1: Indications, technique, management. Chest 90: 269-274.
- Durbin CG (2005) Early complications of tracheostomy. Respir Care 50: 511-515.
- Oliver ER, Gist A, Gillespie MB (2007) Percutaneous versus surgical tracheotomy: an updated meta-analysis. Laryngoscope 117: 1570-1575.
- Molardi A, Benassi F, Manca T, Ramelli A, Vezzani A, et al. (2016) Parma tracheostomy technique: A hybrid approach to tracheostomy between classical surgical and percutaneous tracheostomies. J Thorac Dis 8: 3633-3638.
- Halum SL, Ting JY, Plowman EK, Belafsky PC, Harbarger CF, et al. (2012) A multi-institutional analysis of tracheotomy complications. Laryngoscope 122: 38-45.
- Scurry WC, McGinn JD (2007) Operative tracheotomy. Operative techniques in Otolaryngology 18: 85-89.
- Fikkers BG, van Veen JA, Kooloos JG, Pickkers P, van den Hoogen FJ, et al. (2004) Emphysema and pneumothorax after percutaneous tracheostomy: case reports and an anatomic study. Chest 125: 1805-1814.
Citation: Poghosyan AY, Malkhasyan IE, Shahparonyan RG, Manucharyan GK, Tadevosyan AE (2018) Modified Method of Tracheostomy in ICU Patients in “Heratsi” No.1 Hospital. J Interdiscipl Med Dent Sci 6: 226. DOI: 10.4172/2376-032X.1000226
Copyright: © 2018 Poghosyan AY, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 6143
- [From(publication date): 0-2018 - Dec 07, 2025]
- Breakdown by view type
- HTML page views: 5229
- PDF downloads: 914