Nail-stem Construct Method for Periprosthetic Humeral Fractures with Recalcitrant Nonunion after Total Elbow Arthroplasty: A Surgical Technique
Received: 26-May-2022 / Manuscript No. JMIS-22-64964 / Editor assigned: 30-May-2022 / PreQC No. JMIS-22-64964(PQ) / Reviewed: 13-Jun-2022 / QC No. JMIS-22-64964 / Revised: 25-Jul-2022 / Manuscript No. JMIS-22-64964(R) / Published Date: 02-Aug-2022
Abstract
Background: Implant loosening and periprosthetic fracture nonunion is the most challenging complications of total elbow arthroplasty. There is limited literature on how to treat these conditions. This study describes the surgical technique used in an innovative nail-stem construct and evaluates patient outcomes following this salvaging method.
Case presentation: We present four cases in this study between 2018 and 2019. All four patients (average age 78.7 years) achieved an optimal range of motion and secure stability with a painless elbow at the final follow-up.
Conclusion: Our innovative, low cost nail-stem construct procedure is a feasible alternative for revision total elbow arthroplasty in patients with implant loosening, periprosthetic humeral fractures, and recalcitrant nonunion.
Keywords: Implant loosening; Total elbow arthroplasty; Nail-stem construct; Revision surgery; Recalcitrant nonunion
Introduction
Total Elbow Arthroplasty (TEA is increasingly performed in recent years; however, TEA involves a higher percentage of complications and revisions compared to other arthroplasty sites [1]. The survival rates of TEA have been shown to be 92%, 81%, 71%, and 61%, at 5, 10, 15, and 20 years, respectively [2]. Infection, aseptic loosening and periprosthetic fractures are the common complications that require revision surgery; whereas, a periprosthetic fracture with recalcitrant nonunion in an aseptic loosened implant is the most complex complication following TEA [3,4]. This may be related to several factors, including patient age, prosthetic design, and multiple prior surgical procedures [5,6]. Ligament deficiency caused by nonanatomic force transmission in a semi-constrained implant is the primary reason that leads to substantial bone resorption [7]. In a study of 92 TEAs with a mean follow-up of 6.5 years, the rate of mechanical implant failure was 25%, and more than half of the study population showed aseptic loosening [5]. The overall complication and revision rates have been reported to be approximately 24% and 13%, respectively [8,9]. Furthermore, fractures around the loose prosthesis associated with massive bone loss are technically challenging and devastating scenarios in revision TEA [10]. Although revision of the loose prosthesis and reduction of the fracture with allograft reconstruction have been the gold standard of treatment, recalcitrant nonunion may still develop, even with different osteosynthesis methods. To overcome it, we developed an innovative and inexpensive procedure using a nail-stem construct for salvaging this kind of periprosthetic humeral fractures following TEA. Similar approaches in cases of periprosthetic femoral fractures with nonunion after total hip arthroplasty had been described, which involved treatment with nails overlapping the femoral stem tip [11-14]. The concept of our nail-stem construct used in the elbow was inspired by the procedures implemented in the hip. To our knowledge, although the basic principle was similar, no report on using this technique on the elbow has been published. Herein, we describe the procedures in detail and report the encouraging early results in four patients using the nail-stem construct.
Case Presentation
Between 2018 and 2019, we included four patients diagnosed with implant loosening and periprosthetic humeral fractures subsequent to previous TEA (Coonrad-Morrey Total Elbow, Zimmer). The demographics involved patient age, sex, lesion site, number of previous surgeries, and the time from the primary TEA to the nailstem reconstruction (Table 1). A total of one right and three left elbow nail-stem reconstruction procedures were performed at our hospital. All four patients were women with an average age of 79.3 years who had previously undergone TEA for rheumatoid arthritis (two cases) and traumatic osteoarthritis (two cases). The review and publication of patient data in this study were ethically approved by the institutional review board committee of the Buddhist Dalin Tzuchi Hospital Taiwan.
| Age | Gender | Number of previous surgeries (Exclude nail-stem construct) | Time period from primary TEA to ail-stem construction |
Lesion site based on *Mayo classification |
Blood loss | Operation time | Mean hospital stay | Pre/Post op VAS | Elbow motion arch | Union | Follow-up time | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Case 1 | 73 y/o | Female | 5 | 12 years | H-II3 | 500 cc | 2 hours | 12 days | 06-Jan | 45–120 degrees | Solid union | 36 months |
| Case 2 | 76 y/o | Female | 4 | 10 years | H-II3 | 400 cc | 2 hours | 7 days | 07-Jan | 30–120 degrees | Solid union | 24 months |
| Case 3 | 87 y/o | Female | 1 | 10 years | H-II3 | 300 cc | 2 hours | 7 days | 07-Jan | 0–130 | Solid union | 16 months |
| Case 4 | 81 y/o | Female | 4 | 10 years | H-II3 | 350 cc | 4 hours | 6 days | 06-Jan | 40–120 degrees | Solid union | 12 months |
| Average | 79.3 y/o | - | 3.5 | 10.5 years | H-II3 | 387.5 cc | 2 hours | 8.5 days | 6.5/1 | 28.75–122.5 degrees | - | - |
Table 1: Patient data and the result of the four cases.
Case 1: A 73-year-old woman underwent left primary TEA 13 years ago due to rheumatoid arthritis. A periprosthetic humeral fracture around the loosened stem occurred after a fall five years postoperatively. In the following seven years, a total of five surgeries were performed at two medical centers, resulting in persistent loosening and nonunion. Triceps insufficiency and fibrosis were noted due to repetitive trauma after multiple surgeries.
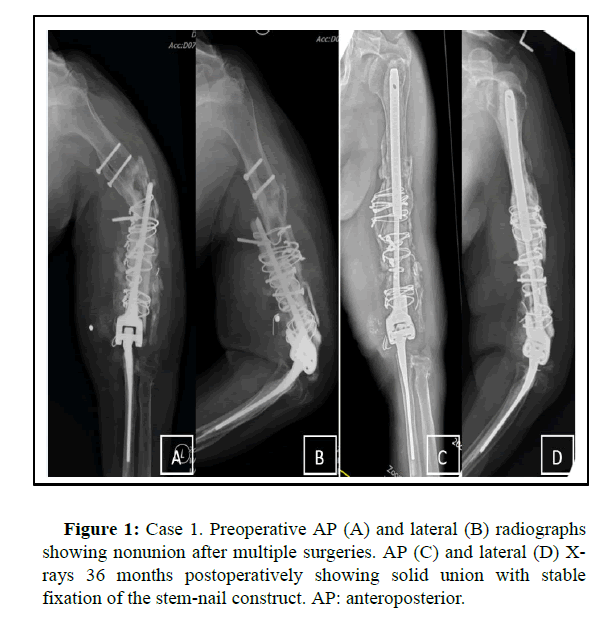
Previous revision procedures included a conventional plate and wire with auto-bone grafts, exchange with a long stem, and onlay allo-bone grafts. We used the nail-stem construct to treat the recalcitrant nonunion, and double allogenous bone plates were fixed with cerclage wires (Figure 1).
Case 2: A 76-year-old woman with rheumatoid arthritis was referred to our hospital due to failed osteosynthesis for a periprosthetic humeral fracture. Recalcitrant nonunion persisted despite three previous revision surgeries. The last surgical procedure consisted of locking plate fixation and autogenous bone chip grafts. Triceps insufficiency was also noted after previous surgeries. We solved this problem after adopting the nail-stem construct and double allogenous bone plate fixation.
Case 3: An 87-year-old woman sustained an acute periprosthetic fracture of the distal humerus after a fall. She had undergone primary TEA for traumatic osteoarthritis 11 years ago, and aseptic loosening of the humeral stem was found postoperatively. We treated the loosened implant and fracture with a nail-stem construct.
Case 4: An 81-year-old woman underwent left primary TEA 10 years ago due to traumatic osteoarthritis. A periprosthetic humeral fracture around the loosened stem occurred after a fall. Persistent implant loosening and recalcitrant nonunion occurred despite four surgeries being performed at two medical centers. The last surgical procedure consisted of the conventional plate and wire fixation with double allogenous bone plating. Physical examination showed triceps insufficiency and fibrosis before our surgery. We solved this problem after adopting the nail-stem construct and double allogenous bone plates with cerclage wire fixation.
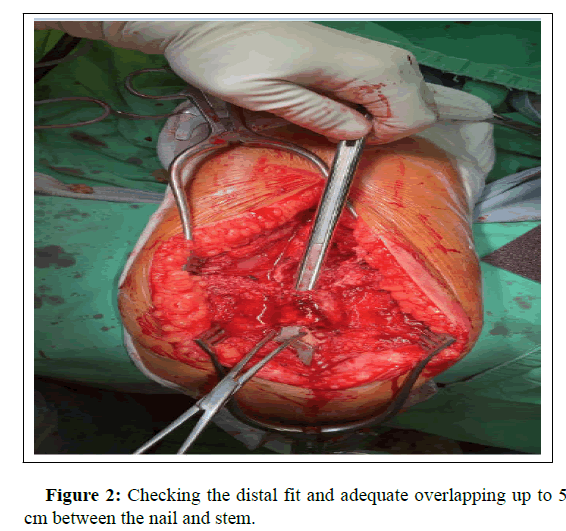
Surgical technique: The affected arm was placed on an elbow support in the lateral decubitus or prone position. A posterior incision was made with the triceps muscle split at the midline to expose the distal humerus. After identifying the radial nerve, extensive debridement was performed to remove all the previously implanted cement, K-wires, and screws/plate. Without disassembling the prosthetic ulnohumeral hinge (Coonrad-Morrey Total Elbow, Zimmer), the humeral stem was pulled out from the intramedullary (IM) canal. The proximal humeral IM canal was then over reamed at least 2 mm to facilitate smooth nail (Nailing System, Stryker) insertion. An appropriate cutting length of the nail was easily docked distally to the tip of the humeral stem with 3 to 5 cm of overlap into the stem and was long enough proximally to reach the humeral head in order to achieve construct stability (Figure 2).
The selected IM nail was pushed into the humeral canal and then pulled back distally several times to achieve the final nail-stem construct. Then the cement was packed into the humeral canal, and the IM nail was inserted to lead the stem into the nail, with the interface being cemented to augment fixation. At the final setting of the cemented nail-stem composite, elbow flexion-extension was checked to achieve a maximal range of motion, and the anatomical alignment was assured via fluoroscopy. For the periprosthetic bone defect, the harvested allografts chip was impacted, and double bone plates were subsequently fixed with cerclage wires. The wound was closed, and a sling protection was implemented for six to eight weeks. A rehabilitation program was initiated on the first postoperative day.
Results
In our four patients, the average duration from the primary TEA to the final revision with a nail-stem construct was 10.5 years, and the number of previous surgeries averaged 3.5. All the fractures were Mayo classification type II [3]. For the nail-stem construct procedure, the surgical time averaged 2 hours 40 minutes, the blood loss averaged 387.5 cc and the mean hospital stay was 8.5 days (Table 1).
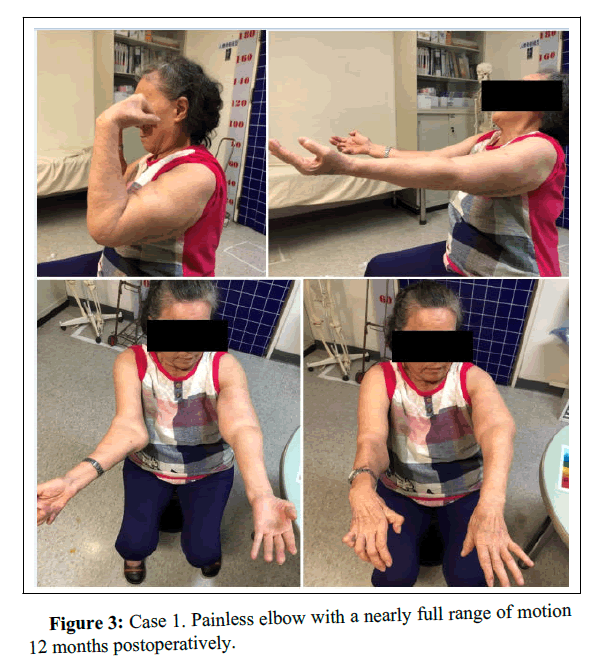
Preoperatively, all patients showed painful disability with deformity and instability. The average preoperative Visual Analog Scale (VAS) score was 6.5. Triceps insufficiency was fibrotic and moderate atrophy was noted in cases 1, 2 and 4 prior to surgery; however, adequate range of motion with a painless and stable elbow could be achieved in 1 year (Figure 3). The postoperative VAS score was 1. There were no complications, such as radial nerve injury, infection, or instability. Radiographically, solid unions were achieved in all cases without implant loosening or refracture at the final follow-up.
Discussion
Periprosthetic fracture nonunion associated with humeral stem loosening remains the most technically demanding due to extensive bone loss, poor bone quality and soft tissue contracture. Recalcitrant nonunion with persistent loosening of the humeral component continues to occur despite various osteosynthesis techniques, such as plate/screw/wire fixation, locking plate fixation, onlay allogenous bone plating, or revision with a longer stem. Therefore, we developed an innovative elongation technique to provide a “serviceable elbow” for patients with humeral bone loss following TEA. This technical procedure was successfully adopted in older patients who had failed multiple surgeries. The longevity of such a functional elbow can be maintained under protected weight lifting over three years, as demonstrated in our four cases. Although loosening may be a concern in the future due to the semi-constrained hinge design, the current longer and larger nail-stem reconstruction can be expected to decrease the incidence of loosening to the least extent.
Morrey [15] performed allograft-prosthetic composite reconstruction for massive bone loss with a less desirable outcome of limited functional restoration. Sanchez-Sotelo et al. [16] treated periprosthetic humeral fractures associated with a loose component, and subsequent implant revision using strut allograft augmentation resulted in a substantial complication rate. Endoprosthetic arthroplasty has been associated with poor outcomes and high complication rates in up to 50% of cases [4-18]. In our study, in relation to cases 1, 2, and 4, multiple attempts for osteosynthesis had failed in other hospitals even with the locking plate fixation procedure or revision with a longer stem. Marti [19] used a vascularized fibula graft with double plate fixation for a patient with extensive segmental loss of the humerus. The free fibular graft brings vascularity to the region of humeral nonunion with a background of a previous pathological fracture following radiotherapy. In our cases, unions were achieved even in the presence of a suboptimal soft tissue environment because adequate construct stability and a massive amount of bone grafting around the fracture site were achieved (Table 2).
| Surgical methods | Representative origin | Disadvantages | Advantages |
|---|---|---|---|
| Allograft-prosthetic composites. | Morrey et al. | Limit functional outcome/unavailable in hospitals with allograft shortage. | Recreate a bone stock. |
| Onlay allogenous bone plating. | Sanchez-Sotelo J. | Technique-demanding procedure/substantial complication rate. | Satisfactory result. |
| Endoprosthetic arthroplasty | Torbert JT. | Poor outcome/high complication rate. | Easy procedure/low technique demanding. |
| Vascular graft +plating. | Martin et al. | Difficulty with vessel end to end anastomosis due to fibrosis and scarring. | Vascularity leading to bone regeneration ability. |
| Nail-stem constructs. | JT chien | Need longer follow-up time/technique-demanding procedure. | Inexpensive/innovative/durable alternative procedure. |
Table 2: The advantage and disadvantage of different methods for periprosthetic humeral shaft fractures with severe bone loss.
There are multiple benefits of the nail-stem construct. Disconnecting the hinge is not required, and the original humeral and ulnar components can be retained without exchange. Therefore, it is an inexpensive procedure compared to the revision with a long stem or conversion to an endoprosthesis. The IM nail can accomplish an excellent fit with its larger diameter compared to the very thin humeral stem. Furthermore, the nail length can be customized to reach the humeral head. This kind of IM construct can provide enough stability and realign the humeral stem to a functional position, unlike the extramedullary plate fixation that failed in an osteoporotic humerus [20].
Some technical specifications of this procedure need to be emphasized. First, multiple fit trials prior to final cementation are essential to achieve a smooth and trouble-free insertion of the whole construct into the humeral canal. Second, suboptimal length of the nail can cause a compromise in the range of motion and difficulty in implantation. Third, overlapping between the nail and the stem should be more than 3 cm to avoid rotational instability or dislodgement. In a biomechanical model, Melvin reported that to obtain a stable stem-nail connection, 2.9 to 3.5 cm of overlap should be achieved. Lastly, full cementation helped maintain the whole construct among the interfaces of the humeral canal, the nail and the stem. The additional allografts can impact the periprosthetic bone defect to provide further bone stock. In our study, there was no sign of construct loosening within three years of follow-up despite mobilization from the first postoperative day. All our patients obtained painless elbows and returned to normal activity.
The current large and long nail-stem construct can eliminate the development of stress risers commonly seen in thin and short stems, which the major problems are causing instability and progressive loosening. With the positive results that we saw in the revision scenarios, we applied this nail-stem construct method in the case 3 patients who had severe rheumatoid arthritis in the primary setting to prevent further failure of periprosthetic fracture nonunion.
Conclusion
This study has some limitations, such as a short follow-up time and a small number of cases. Besides, it is a technically demanding procedure; therefore, a favorable outcome may not be achieved by inexperienced surgeons.
Recalcitrant nonunion of humeral components following TEA represents a challenge. The loosened humeral stem can be salvaged by intramedullary fixation using a nail-stem construct and onlay allogenous bone plating. The outcome of fracture union, implant survival, and satisfactory clinical results require more cases and longer-term follow-up in this off-labor use technique.
References
- Gschwend N, Scheier NH, Baehler AR (1999) Long-term results of the GSB III elbow arthroplasty. J Bone Joint Surg Br 81:1005-1012.
- Krukhaug Y, Hallan G, Dybvik E, Lie SA, Furnes ON, et al. (2018) A survivorship study of 838 total elbow replacements: a report from the Norwegian Arthroplasty Register 1994-2016. J Shoulder Elbow Surg 27:260-269.
- Kwak JM, Koh KH, Jeon IH (2019) Total elbow arthroplasty: clinical outcomes, complications, and revision surgery. Clin Orthop Surg 11:369-379.
- Kim JM, Mudgal CS, Konopka JF, Jupiter JB (2011) Complications of total elbow arthroplasty. J Am Acad Orthop Surg 19:328-339.
- Erşen A, Demirhan M, Atalar AC, Atıcı T, Kapıcıoglu M, et al. (2015) Is Coonrad-Morrey total elbow arthroplasty a viable option for treatment of distal humeral nonunions in the elderly? Acta Orthop Traumatol Turc 49:354-360.
- Cil A, Veillette CJ, Sanchez-Sotelo J, Morrey BF (2008) Linked elbow replacement: a salvage procedure for distal humeral nonunion. J Bone Joint Surg Am/90:1939-1950.
- Kaufmann RA, D'Auria JL, Schneppendahl J (2019) Total elbow arthroplasty: elbow biomechanics and failure. J Hand Surg Am 44:687-692.
- Voloshin I, Schippert DW, Kakar S, Kaye EK, Morrey BF, et al. (2011) Complications of total elbow replacement: a systematic review. J Shoulder Elbow Surg 20:158-168.
- Little CP, Graham AJ, Karatzas G, Woods DA, Carr AJ, et al. (2005) Outcomes of total elbow arthroplasty for rheumatoid arthritis: comparative study of three implants. J Bone Joint Surg Am 87:2439-2448.
- Ramirez MA, Cheung EV, Murthi AM (2017) Revision total elbow arthroplasty. J Am Acad Orthop Surg 25:166-174.
- Verburg AD (1998) Retrograde nailing of femoral fracture below a hip prosthesis: a case report. J Bone Joint Surg Br 80:282-283.
- Cassar Gheiti AJ, Baker JF, Brown TE, Mulhall KJ (2013) Management of total femoral bone loss using a hybrid cement spacer surgical technique. J Arthroplasty 28:347-351.
- Richards C, Bell CJ, Viswanathan S, English H, Crawford RW, et al. (2010) Use of a cement-loaded Kuntscher nail in first-stage revision hip arthroplasty for massive femoral bone loss secondary to infection: a report of four cases. J Orthop Surg 18:107-109.
- Zuurmond RG, Pilot P, Verburg AD, van Os JJ, Verdonschot N (2008) Retrograde bridging nail in periprosthetic femoral fracture treatment which allows direct weight bearing. Proc Inst Mech Eng H. 222:629-635.
- Morrey ME, Sanchez-Sotelo J, Abdel MP, Morrey BF (2013) Allograft-prosthetic composite reconstruction for massive bone loss including catastrophic failure in total elbow arthroplasty. J Bone Joint Surg Am 95:1117-1124.
- Sanchez-Sotelo J, O'Driscoll S, Morrey BF (2002) Periprosthetic humeral fractures after total elbow arthroplasty: treatment with implant revision and strut allograft augmentation. J Bone Joint Surg Am 84:1642-1650.
- Ross AC, Sneath RS, Scales JT (1987) Endoprosthetic replacement of the humerus and elbow joint. J Bone Joint Surg Br 69:652-655.
- Torbert JT, Fox EJ, Hosalkar HS, Ogilvie CM, Lackman RD, et al. (2005) Endoprosthetic reconstructions: results of long-term follow-up of 139 patients. Clin Orthop Relat Res 438:51-59.
- Gathen M, Norris G, Kay S, Giannoudis PV (2019) Recalcitrant distal humeral non-union following previous leiomyosarcoma excision treated with retainment of a radiated non-angiogenic segment augmented with 20 cm free fibula composite graft: A case report. World J Orthop 10:212-218.
- Melvin JS, Smith JL, Sims SH, Patt JC (2012) The use of an interference fit retrograde nail as an adjunct to plate fixation of a complex Vancouver B1 periprosthetic femoral fracture. Injury 43:1779-1782.
Citation: Chiang YS, Chen SH, Liu KC, Yang CC, Chien JT (2022) Nail-stem Construct Method for Periprosthetic Humeral Fractures with Recalcitrant Nonunion after Total Elbow Arthroplasty: A Surgical Technique. J Med Imp Surg 7: 148.
Copyright: © 2022 Chiang YS, et al. This is an openaccess article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 1289
- [From(publication date): 0-2022 - Dec 20, 2025]
- Breakdown by view type
- HTML page views: 934
- PDF downloads: 355