Review Article Open Access
Non-Communicable Disease Prevention and Worksite Health Promotion Programs: A Brief Review
Kolbe-Alexander TL* and Lambert EVUCT/MRC Research Unit for Exercise Science and Sports Medicine, Department of Human Biology, School of Health Sciences, University of Cape Town, South Africa
- *Corresponding Author:
- Tracy Kolbe-Alexander
MRC/UCT Research Unit for Exercise Science and Sports Medicine
Department of Human Biology, Faculty of Health Sciences
University of Cape Town Private Bag, South Africa
Tel: 27 21 650 5126
Fax: 27 21 686 7530
E-mail: Tracy.Kolbe-Alexander@uct.ac.za
Received date: September 28, 2013; Accepted date: November 20, 2013; Published date: November 27, 2013
Citation: Kolbe-Alexander TL, Lambert EV (2013) Non-Communicable Disease Prevention and Worksite Health Promotion Programs: A Brief Review. Occup Med Health Aff 1:141. doi: 10.4172/2329-6879.1000141
Copyright: © 2013 Kolbe-Alexander TL, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Occupational Medicine & Health Affairs
Abstract
Introduction: Non-communicable diseases (NCD’s) accounted for nearly two-thirds of global deaths in 2008. The aim of this literature review is to examine current evidence for the role of worksite health promotion programs’ role in the prevention of NCD’s. The prevalence of risk factors for NCD’s among employees and the clustering of risk behaviors among employees will be discussed. In addition, the role of health risk appraisals as an entry for worksite health promotion programs is discussed. Methods: The search strategy included using Pub Med to find relevant manuscripts. Manuscripts that were published within the last 10 years, as well as systematic reviews and meta-analyses were given priority due to the limited scope of this review. Results: Worksite health promotion programs have been shown to result in economic benefits both for the employer and employee. In addition to the economic benefits, previous research has shown that worksite health promotion programs are effective in reducing the risk for NCD’s among employees. Comprehensive worksite health promotion programs which include tailoring the program according to the company’s and employees’ needs have been found to be most effective. In addition, worksite intervention programs that have had the greatest impact on improving employee health were those targeting the employees at highest risk for NCD’s. The Health Risk Assessment (HRA) is one of the most frequently implemented worksite health promotion programs and has been implemented in more than 50% of large companies in the USA by 2004. The HRA is beneficial to identify employees who might be at increased risk for NCD, and could be considered as the first step towards improved health. Conclusion: Worksite health promotion programs have the potential to play a role in reducing the prevalence of NCD’s and their risk factors and both health and economic benefits.
Keywords
Non-communicable disease; Worksite health promotion; Health risk assessment
Introduction
Non-communicable diseases (NCD) are defined as being slow in onset and progression, and long in duration [1]. Diseases including heart disease, stroke, diabetes, chronic respiratory disease and some cancers form part of the definition of NCD [1,2]. These diseases accounted for nearly two-thirds of global deaths in 2008, has been steadily increasing, and impacts on most countries and people of all ages and socio-economic groups [2-4]. This trend is evident in South Africa as well, where NCD’s accounted for 28% of the total burden of disease [5]. In fact, the World Health Organization (WHO) has estimated that the NCD burden in South Africa is more than double that in some developed countries, although similar to that of other Sub- Saharan African countries [5].
Modifiable risk factors that have been shown to play a role in reducing the prevalence of NCDs include tobacco use, an unhealthy diet, excessive alcohol consumption and physical inactivity [2-8]. Other risk factors for NCD include: age, elevated blood pressure, dyslipidemia, elevated serum cholesterol and glucose concentrations, waist circumference, Body Mass Index more than 25 kg/m2 [9]. Data from various studies investigating the odds of having cardio-metabolic disease is presented in Table 1. Results on this table shows that the risk of cardio-metabolic and NCD’s due to physical inactivity is comparable to that of other risk factors. Yet physical activity, has been regarded as the ‘Cinderella risk factor’ as it receives less attention, political commitment and resources than the other risk factors [6]. If it were possible to reduce to the global pandemic of physical inactivity, it has been estimated that between 6-10% of all deaths due to NCD’s may be prevented [8]. Lee et al. calculated that by increasing the prevalence of physical activity by 25% it may be possible to avert 1.3 million deaths annually [8].
| Risk Factor | Risk Factor Category | Prevalence (%) | Odds Ratio / Relative Risk# | 95% Confidence Interval | Data Source | Reference |
| Physical Activity: | Active Somewhat Active Inactive |
50.7 21.3 28.0 |
1.00 (Referent) 1.15 1.52 |
0.84 – 1.57 1.16 – 1.98 |
US NHANES | [9] |
| No LTPA Met PA guideline Exceeded PA Guideline |
1.00 (Referent) 0.91 0.82 |
0.79 – 1.04 0.74 – 0.91 |
Meta-analysis (males) | [37] | ||
| No LTPA Met PA guideline Exceeded PA Guideline |
1.00 (Referent) 0.80# 0.72# |
0.69 – 0.92 0.63 – 0.83 |
Meta-analysis (females) | [37] | ||
| Inactive (<150min/wk) | 1.17 | 1.01 – 1.36 | BRFSS | [38] | ||
| Smoking Status | Non-Smoker Ex-Smoker Current Smoker |
52.3 24.4 23.3 |
1.00 (Referent) 1.90# 2.31# |
1.45 – 2.50 1.67 – 3.20 |
US NHANES | [9] |
| Current Smoker | 1.37 | 1.10 – 1.70 | BRFSS | [38] | ||
| Never Smoker Current smoker |
1.00 (Referent) 1.42 |
1.01 – 201§ | Lipid Research Clinic’s PFS | [39] | ||
| Blood Pressure | Normal Pre-hypertensive Hypertensive |
43.3 29.3 27.4 |
1.00 (Referent) 0.71 1.21 |
0.49 – 1.01 0.88 – 1.67 |
US NHANES | [9] |
| Glucose | Normal Impaired Diabetes |
67.2 24.7 8.1 |
1.00 (Referent) 0.99 1.50 |
0.76 – 1.30 1.08 – 2.07 |
US NHANES | [9] |
| Triglycerides | Normal Borderline High High |
43.3 29.3 27.4 |
1.00 (Referent) 0.89 1.21 |
0.64 – 1.21 0.90 – 1.64 |
US NHANES | [9] |
| LDL Cholesterol | Optimal Near optimal Borderline High |
26 30.8 21.6 21.6 |
1.00 (Referent) 0.86 0.82 1.99 |
0.54 – 1.127 0.55 – 1.24 1.42 – 2.83 |
US NHANES | [9] |
| HDL Cholesterol | High Normal Low |
26.8 53.4 19.8 |
1.00 (Referent) 1.37 1.89 |
|
US NHANES | [9] |
| Body Mass Index | BMI >24.9 | 1.30 | 1.11 – 1.52 | BRFSS | [38] | |
| Waist Circumference | Low Moderately high High |
31.4 21.8 46.9 |
1.00 (Referent) 1.45 1.46 |
0.99 – 2.12 1.04 – 2.08 |
US NHANES | [9] |
BRFSS: Behavioral Risk Factor Surveillance System
PFS: Princeton Follow Up Study
§ = adjusted for confounders and other risk factors
LTPA = Leisure time physical activity
Table 1: The relative risk and odds ratio’s for cardio-metabolic disease from various studies.
Furthermore, non-communicable diseases have a negative impact on the global economy and have been identified as one of the major threats to economic development by the World Economic Forum [2-4]. The reduction in economic growth is estimated at 0.5% for every 10% increase in NCD-related mortality [4]. Worksites and companies are directly affected by NCD’s due to reduced employee productivity, increased absenteeism and increased likelihood of disability [2]. The loss in national income due to NCD’s is substantial. The projected loss in income from 2005 to 2015 in countries with emerging economies similar to South Africa, range from 49.2 billion international dollars in Brazil to 236.6 billion international dollars in India [10]. Therefore, countries, worksites and individuals are likely to incur higher medical expenditures and reduced productivity due to NCD’s. Some of the NCD’s can be prevented or managed by implementing screening and intervention programs.
Therefore the aim of this literature review is to examine current evidence for the role of worksite health promotion programs’ role in the prevention of NCD’s. The prevalence of risk factors for NCD’s among employees, with a focus on physical activity, and the clustering of risk behaviors among employees will be discussed. In addition, the economic consequences of NCD’s and possible benefits of worksite intervention programs are briefly addressed. The main component of the literature review reports on the role of health risk appraisals as an entry for worksite health promotion programs.
Methods
Search strategy and quality criteria
The search strategy included using the online database, Pub Med to find relevant manuscripts. Various combinations of the following terms were used when searching the Pub Med database; ‘worksite health promotion programs’; ‘non-communicable disease risk factors AND cluster of risk’; ‘economic burden AND non-communicable diseases; ‘physical activity AND worksite’; and ‘physical activity AND employee health’. The references in some of the manuscripts that were sourced were also examined for additional publications. In addition, reports from the World Economic Forum’s Workplace Wellness Alliance website (http://alliance.weforum.org/) were obtained.
Manuscripts that were published within the last 10 years, as well as systematic reviews and meta-analyses were given priority due to the limited scope of this review and, in some cases, paucity of data available.
Results
Rationale for worksite intervention programs
It has been estimated that more than 3.6 billion people will form part of the global workforce by 2020 [10]. Consequently, the worksite has identified as an opportune setting for health promotion programs aimed at improving employee health status and productivity since many people can be reached in this setting [11-13]. Employers have the opportunity to engage with employees on an ongoing basis with extensive reach and frequent interaction [14]. Indeed, the Report of the Secretary General, UN General Assembly, May 2011, recommends that the private sector play a role in promoting healthy lifestyle behaviors among employees including both health promotion policies and worksite health promotion programs [3].
Worksite health promotion programs have been shown to result in economic benefits both for the employer and employee [10]. The economic outcomes of worksite intervention programs includes increased productivity and reduced absenteeism and healthcare expenditure [12]. Evidence from a recent review of the economic benefits of these programs concluded that it is ‘one of the most effective strategies for reducing medical costs and absenteeism’ [15]. Consequently, more and more employers are implementing health promotion and intervention programs in their companies [12]. The economic outcomes of worksite health promotion programs will be discussed in more detail later in this literature review.
In addition to the economic benefits, previous research has shown that worksite health promotion programs are effective in reducing the risk for NCD’s among employees [16]. Although the effect sizes of these interventions on health vary and are less than that observed in clinical trials, it has still been advocated as it results in marginal changes [16]. Small changes in behavior and health parameters have been shown to result in a considerable impact on disease risk when observed at a population level [10].
The next section of the literature review will present data on the prevalence of NCD risk factors followed by an overview of the effectiveness of worksite health promotion programs.
Prevalence of NCD risk factors in the worksite
The main risk factors for NCD’s were reported in the introduction of this literature review. The risk factors that encompass lifestyle behaviors, namely, physical activity, and healthy diet (together with obesity) will be the focus of this section of the review. Indeed, the WHO identified these behaviors as among the five leading causes for global mortality [17].
Physical inactivity is widely recognized as a major risk factor for NCD’s [7,8]. If it were possible to reduce to the global pandemic of physical inactivity, it has been estimated that between 6-10% of all deaths due to NCD’s may be prevented [8]. For example, approximately 21-25% of breast and colon cancer and 27% of the burden of diabetes could be reduced by reducing the levels of physical inactivity [17]. However, more than half (58%) of the world’s population do not meet the physical activity guidelines, which is similar to the number of Africans who are currently insufficiently physically active (60%) [17].
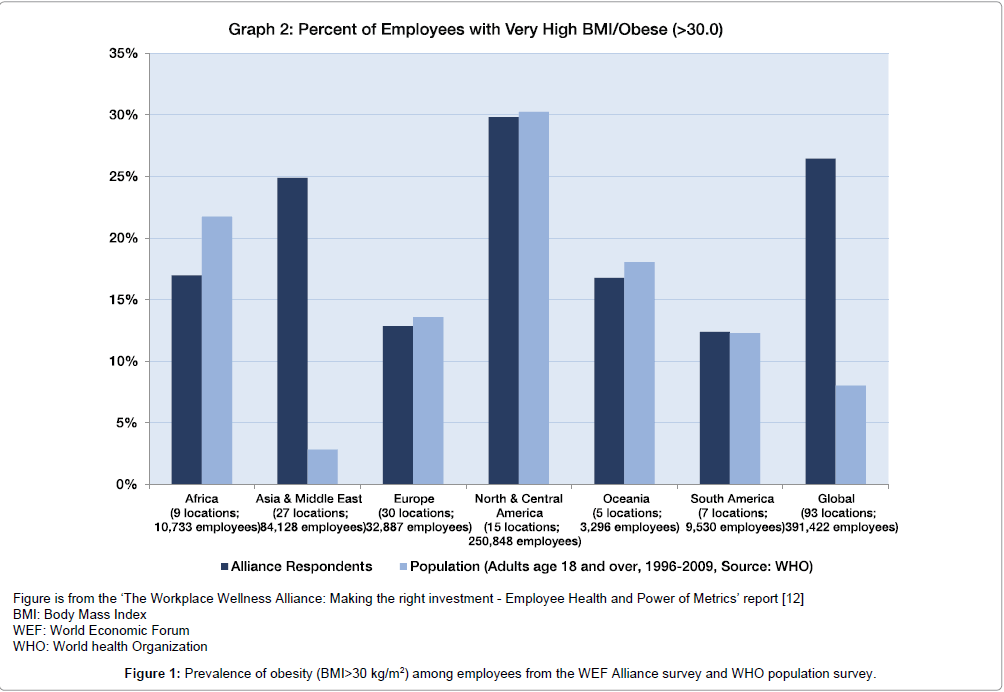
Changes in dietary behaviors with increased consumption of refined starch, sugar, salt and unhealthy fats has contributed to the increased prevalence global prevalence of obesity, which has more than doubled since 1980 [1,12]. A recent WHO report states that four in ten people are either overweight or obese (BMI 24.9 kg/m2) [17]. The ‘Workplace Wellness Alliance’ reported that the prevalence of obesity in African employees is nearly 20%, and is higher than that reported for Europe and South America [12]. This prevalence is slightly less than that reported in the population average which is from WHO survey which was conducted in adults (not only in the worksite setting) between 1996 and 2009 (Figure 1) [12]. Furthermore, the WHO reported that 41% of all deaths in Africans under the age of 60 years could be attributed to a high Body Mass Index [17].
The prevalence of NCD and cardio-metabolic disease has been investigated in the employed population, although less so in South Africa. Ker et al., 2007 described the frequency of metabolic syndrome among South African corporate executives comprising of men (n=1367) and women (n=25) with a mean age of 46 ± 7.9 years [18]. They found that nearly a third (31%) had metabolic syndrome as defined by ATP III criteria [18]. Furthermore, more than a third (36%) met two of the ATP III criteria for the diagnosis of the metabolic syndrome [18].
The increased prevalence of NCD is coupled with high proportion of employees having multiple risk factors. A pilot study among South African companies (n=18) found that the employed population was at an increased risk for NCDs and that a greater proportion of employees had poor lifestyle behaviors compared to the general South African population [19]. For example, nearly 70% of employees were not meeting the recommended 30 minutes of physical activity on at least 5 days of the week based on the Centers for Disease Control’s (CDC) and US Surgeon General’s report. Furthermore, nearly half of the employees were overweight, defined as a Body Mass Index (BMI) more than 24.9, and nearly a quarter were current smokers [19]. These findings are supported by a more recent study in which nearly 58% of the employees were either overweight or obese and 70% were not meeting the physical activity guidelines [20]. Approximately 31% of the employees in their survey had elevated serum cholesterol concentration while 81 and 91% had normal blood pressure and serum glucose concentrations, respectively [20]. These findings suggest that South African employees are at increased risk for NCD’s and would benefit from worksite health promotion programs.
Clustering of NCD risk factors with physical activity
Physical inactivity appears to cluster with other risk factors for cardiovascular disease whereby individuals who are inactive are more likely to have additional risk factors for cardio metabolic disease [9,21]. There has also been some research investigating the relationship between physical activity and other health risk in the employee population. This includes a four-year longitudinal study among Japanese full-time workers which was conducted in 12 large scale companies [22]. Participants were divided into four physical activity groups based on the results obtained at the outset, from the International Physical Activity Questionnaire (IPAQ). Those who exceeded 3000 MET minute per week were categorized as highly active; those who were active for < 3000 but > 1500 MET minutes per week were moderately active; while those who achieved <1500 but >600 MET minutes and <600 MET minute per week were categorized as some activity and sedentary, respectively [22]. Japanese employees with more than 4 diagnostic criteria for Metabolic syndrome were more likely to have lower levels of physical activity, however this was not significant in the univariate analysis [22]. In addition, when stratified according to Body Mass Index, levels of physical activity were not significantly associated with number of diagnostic criteria for metabolic syndrome among the Japanese workers. However, physical activity, as quantified by the IPAQ, was significantly associated with number of metabolic syndrome criteria in the Poisson regression analysis which included gender, age, smoking habits and daily alcohol consumption [22].
These findings are supported by Mozumdar and Liguori who investigated the relationship between occupational and leisure time physical activity with metabolic syndrome in 642 female America employees [23]. The employees, who were inactive during their occupation, also reported lower levels of leisure time physical activity. Furthermore, the employees who were inactive at work and during their leisure time also had significantly higher Body Mass Index and waist circumferences than those who were physically active. The odds of the inactive employees having Metabolic syndrome was 1.94 times higher (OR: 1.94; 95% CI: 1.32-2, 85) than those who participated in at least 150 minutes of moderate intensity physical activity per week [23].
Effectiveness of worksite health promotion programs on employee health
Addressing NCD’s in the workplace was reported as one of the most important and urgent concerns among the world’s business leaders [1]. An overview of the effectiveness of various worksite health promotion programs that encourages behavior change is presented in Table 2.
| Reference | Intervention | Participants | Outcome Measures |
| Barham et al. [40] | Twelve weekly sessions aiming to promote improved lifestyle behaviors. Monthly and 12 month follow up. |
Employees at risk for diabetes (n=45) or with diabetes (n=10) | Significant reductions in weight, BMI, waist circumference, and Physical activity after 3 months in the intervention group. No significant improvements in blood pressure, lipid and glucose. |
| Engbers et al., 2007 [41] | Food-based: Information sheets in food canteen, identification of healthy foods Brochures on healthy lifestyle Physical Activity: Point-of-decision prompts to use the stairs Slimming mirrors placed in stairwell 3 and 12 month follow up |
Government companies (n=2) Office workers (n = 641) |
Significant improvements in total cholesterol for women (-0.35mmol/l) and increased HDL in men (0.05mmol/l) at 3 months. Significant decrease in systole blood pressure (4mm Hg). BMI decreased (but not significantly) whereas there were significant decreases in skinfold measurements. |
| Groeneveld et al., 2011 [42] | Individual counseling using Motivational Interviewing techniques. Each participant had 3 face-to face and four telephonic counseling sessions. 6 and 12 month follow up |
Construction workers (n=816) with increased risk for NCD | Fruit intake increased at 6 months. Reduction in unhealthy snacks at 6 and 12 months. No significant effects on leisure time physical activity. Significant reduction in smoking at 6 months, but not at 12 months. |
| MacKinnon et al., 2010 [43] | Self-help educational materials, Motivational interviewing-based counseling sessions, group based counseling sessions, internet-based activities. Follow up every 6 months for 4 years |
Firefighters (n = 599) | Employees in the group based sessions increased fruit and vegetable intake. Those with individual based counseling increased habitual levels of physical activity and fitness. |
| Pressler et al., 2010 [44] | 12 week internet-based intervention comprising of initial education session, followed by structured exercise sessions and concluded with another education session. Baseline and 12 week follow up. |
Overweight employees (n=140); | Employees in the intervention group had significant improvements in fitness, waist circumference and reduced weight. The control group had significant improvements in waist circumference. |
| Prior et al., 2005 [45] | 15 minute screening and counseling session. Educational booklets on cholesterol, blood pressure and smoking |
Female employees (n=113) and male employees (n=4198); participants stratified according to NCD risk | Employees at high risk for NCD showed improvements in Blood pressure, total cholesterol, BMI for both men and women. There were no significant changes on physical activity score. |
| Terry et al., 2011 [46 ] | Tailored, telephone-based counseling program aiming to promote weight loss. | Private sector companies (n=10) with total of 1298 obese or overweight employees | Nearly half the program completers (48%) and non-completers (47%) lost weight. However the completers averaged 2.6 times higher weight loss than those who did not complete the intervention. |
BMI=Body Mass Index
Table 2: Summary of selected Worksite health promotion programs encouraging lifestyle behavior change.
A recent systematic review of worksite health promotion programs and their effect on health and economic outcomes was conducted by Osilla et al., 2012 [24]. The thirty-three studies were included in the Osilla review if they were United States based and had a control group for the comprehensive worksite health promotion program [24]. Most of the interventions aimed to improve physical activity and dietary behaviors [24]. Eight of the 13 studies that evaluated physical activity reported increased levels of physical activity among employees. However only 3 of the seven randomized control trials found improvements in physical activity. None-the-less, improvements included an increase in 103 minutes of walking per week among the intervention group [24]. Similarly, half of the studies that measured dietary outcomes reported increased fruit and vegetable intake, and lower dietary fat intake [24]. This review underscored the importance of evidence-based interventions, with a strong research design and sufficient statistical power to detect meaningful effects of the intervention [24].
Other reviews have reported that interventions in which the primary focus is physical activity have been effective in increasing employees’ habitual levels of physical activity, in addition to improving body composition, fitness levels and a decreasing muscular skeletal disorders [10]. These findings are supported by a meta-analysis which included published and un-published physical activity-based intervention studies from 1969 until 2007 [25]. The effect size calculated for physical activity in the meta-analysis was 0.21 which equated to the intervention group walking approximately 612 extra steps per day than the control group at the post-test measurement [25]. In addition, fitness, quantified by maximal oxygen consumption was higher for the employees in the intervention group compared to the control group [24]. This metaanalysis also found that the risk for diabetes was reduced and that employees’ lipid profile had improved following the intervention [25].
A systematic review evaluating the effectiveness of worksite nutrition and physical activity intervention programs which targeted employees with varying Body Mass Index measures was performed by Anderson and co-authors in 2009 [26]. Forty-seven studies were included in the review, half of which were conducted in the USA and the other half conducted in Europe, Australia, New Zealand, Japan, Canada, India and Iceland [26]. The worksite interventions resulted in small, but significant changes in weight loss of approximately 3 pounds (1.36 kg) after 6-12 months [26]. There were also modest improvements in Body Mass Index (-0.5) body fat percentage after 12 months [26].
Moreover, comprehensive worksite health promotion programs which include tailoring the program according to the company’s and employees’ needs have been found to be most effective [12]. In addition, worksite intervention programs that have had the greatest impact on improving employee health were those targeting the employees at highest risk for NCD’s [16]. These interventions included a health risk assessment with feedback based on the employees screening results, were shown to play a role in employees improving their health behaviors and clinical measures, in addition to economic benefits achieved for employers [16].
The Health Risk Assessment (HRA) is often considered the first step of an intervention program as it provides an overview of employees current health status [27,28]. Therefore, the following section of the literature review will discuss the role of the HRA, its components and effectiveness in improving employee health status.
Health risk appraisal
The HRA has been advocated as a screening tool that should be used together with individual feedback to promote healthy lifestyles for employees [29]. Advances in technology include the introduction of web-based HRA’s and therefore have the potential to increase its potential reach and uptake [13]. Indeed, the HRA is one of the most frequently implemented worksite health promotion programs and has been implemented in more than 50% of large companies (> 750 employees) in the USA by 2004 [13]. An updated survey found that this had increased to 72% of a sample of USA companies offered HRA’s at their worksites [29].
The components of HRA’s vary, but usually include an assessment of lifestyle behaviors, typically self-reported [13]. Clinical measures that are either self-reported or verified / measured also form part of the HRA [13]. Self-report behaviors that could form part of the HRA include physical activity, body mass index, tobacco use, habitual alcohol intake and healthcare services utilization [13,30]. These results are then used to calculate the risk or standardized risk scores for various diseases, including NCD [13]. Ideally, the final component of the HRA might include feedback on the results and guidance to improve lifestyle behaviors and clinical interventions to reduce the risk of adverse health events such as NCDs [13]. The HRA is therefore beneficial to identify employees who might be at increased risk for NCD, and could be considered as the first step towards improved health. Consequently, the HRA is regarded as the ‘gateway intervention’ to more comprehensive health promotion intervention programs [13].
Articipation in HRA’s
HRA participation is largely based on employees volunteering to complete the questionnaires and clinical assessments. Thus it is plausible that a bias exists when reporting HRA data, as this might reflect the proportion of employees who are interested in their health status [28]. In one study of employed persons (n=45,398) from USA companies employer-sponsored health insurance, women, and persons with fewer chronic health conditions are more likely to complete an HRA than their counterparts [28]. The participants were more likely to be members of a consumer-directed health plan than being members of a Health Maintenance Organizations (HMO) or Point-of-Service plans (POS) [28]. Furthermore, participants generally had lower healthcareexpenditures in the previous year than the non-participants (US$242 versus US$ 318) [28].
The determinants of participation in HRA’s among employees (n=5125) at four Dutch companies was recently investigated by Colkesen et al. [31]. All employees were invited to participate in a webbased HRA program. Participants completed the HRA questionnaire, followed by a clinical assessment for anthropometrical measures and blood pressure and a laboratory assessment of serum cholesterol concentration. Each of the participants received tailored feedback based on their results [31]. The non-participants were sent a reminder and questionnaire via email whereby they could report on their self-rated health status and lifestyle behaviors anonymously [31]. The nonparticipants also reported on their reason for declining to participate in the HRA intervention program [31]. The main reasons the nonparticipants reported for failing to complete the HRA was lack of time and lack of awareness of the HRA screening intervention [31]. One of the main findings of this research study was that the participants were significantly older than the non-participants, 44 years and 41 years, respectively, with similar number of men in both groups [31]. Significantly more of the participants (85%) rated their health as either good or very good compared to 78% in the non-participants [31]. In addition, a significantly smaller proportion of the non-participants fewer than 10 days sick leave days in the previous year than the participants (86% versus 88%, p<0.05) [31]. These findings, therefore, support the hypothesis that HRA responders represent the ‘worried well’ employees.
In a similar study, Burton et al. 2003 reported that the pharmaceutical expenses were similar for HRA participants and non-participants [32]. Employees completing the HRA in their research study were more likely to be women, and older than the non-participants [32]. However, the participants reported significantly fewer risk factors than the general US population [32], further supporting the hypothesis that employees who complete the HRA are the ‘worried well”.
Effectiveness of HRA on employee health status
A recent review of the effectiveness of HRA with feedback was conducted by Soler et al. who aimed to establish whether the HRA without feedback and advice leads to behavior change among employees [13]. Research studies included in this review were those that evaluated the effect of HRA’s in the worksite setting and subsequent changes in health status or lifestyle behaviors [13]. Feedback sessions that only took place once and lasting less than one hour were regarded as part of the standard HRA process [13]. ‘Feedback plus’ was defined as those studies in which health education sessions lasting more than an hour, multiple sessions, policy and environmental change, or incentives to promote physical activity and nutrition [13].
These authors concluded that there was insufficient evidence of the effect of this type on intervention on fruit and vegetable intake, body composition and fitness levels of participants [13]. Conversely, there was strong or sufficient evidence for HRA with ‘feedback plus’ to have a positive effect on tobacco use, alcohol intake, dietary fat intake, serum glucose and cholesterol concentration and improved composite risk status [13].
Repeating a HRA multiple times allows for comparison between assessments and to monitor change in health status and behaviors. Pai et al. (2009) researched the association between the frequency of HRA participation and subsequent health status [33]. Their study was based on longitudinal data (1997 – 2004) from a multistate USA-based manufacturing company [33]. All employees received individualized feedback upon completion of the HRA, which served as an entry point into other worksite health promotion programs [33]. The baseline health status was similar for the employees completing only one HRA and those completing two or more during this time period [33]. However, those employees who the HRA more than once had significantly fewer risk factors at follow up than at baseline [33]. In addition, significantly fewer multiple HRA completers experienced a decline in their health status than those who completed the HRA once [33]. This improved health status could be a consequence of the feedback highlighting areas for improvement and suggested intervention or treatment.
One of the unintended consequences of completing an HRA may be short-term increased health-care expenditure among participants. Indeed completing a HRA has previously been associated with increased doctors visits (0.02 visit increase from baseline) and number of prescriptions filled (0.02 increase from baseline) [28]. This was coupled with associated increase in monthly healthcare spending for doctors visits and medication [28]. The economic consequences of completing the HRA will now be addressed in the final section of this literature review.
Economic burden of non-communicable disease
The World Economic Forum states that NCD’s have a substantial and negative impact on the economy due to decreased labor supply, capital accumulation and both country and global gross domestic product (GDP) [1]. This is largely due to the reduced number of employees, resulting in a decrement in the quantity and quality of the labor force [1]. Organizations and companies should therefore be aware of the impact that NCD might have on their employees’ productivity, potential loss of skill, and increased healthcare-related expenditure [1]. Consequently, worksite health promotion programs, including HRA programs are becoming an increasing concern and vital component of employee care [1]. Indeed, implementing worksite intervention programs that targeted healthy eating and obesity resulted in an improvement in labor productivity of 1-2% in a range countries [12].
As documented earlier in this literature review, the HRA can identify the employees’ health risks and the feedback would direct them to interventions to improve their health status and reduce their risk for NCD. It is plausible that an improvement in health status could result in reduced healthcare expenditure. Kowlessar and colleagues investigated the relationship between eleven health risks and medical expenditure [34]. Health risk data were obtained form HRA’s administered by the Mayo clinic while healthcare expenditure was obtained from the Thomson Reuters MarketScan® Commercial Claims and Encounters database [34]. Both the HRA and claims data were for January 2005 to December 2008 [33]. Most of the employees in the sample were men (68-72%) and were salaried (84-85%) [34]. Lifestyle behaviors including physical activity, healthy nutrition and alcohol and tobacco use were associated with reduced healthcare expenditure, absenteeism and presenteeism [34]. Similarly, employees categorized at low risk for serum cholesterol, triglycerides and glucose concentrations had lower healthcare expenditure and increased productivity [34]. Results from a multivariate analyses showed that the main contributors to increased healthcare costs was a Body Mass Index more than 24.9 kg/m2, high blood pressure, high blood glucose, high triglycerides and insufficient physical activity [34]. For example, employees who were meeting physical activity guidelines had 23% reduced healthcare costs than those who were inactive [34].
These findings are supported by similar research studies [32,35,36]. One of these studies by Pronk et al. 2011 investigated the association between health assessment scores and health claims in the subsequent 12 months [36]. These authors calculated a number of scores which included “Total health potential score” (THPS), “modifiable health potential score” (MHPS), a “non-modifiable health potential score” (NMHPS) and a “quality of life score” (QOLS) [36]. The MPHS comprised of physical activity behavior, tobacco use, diet quality, breakfast consumption, fruit and vegetable consumption, calcium, sugar intake, sleep, alcohol use and self reported stress [36]. Each of these health scores resulted in significantly higher healthcare expenditure for the next 12 months [35]. Importantly, a higher MPHS was significantly associated with future annual healthcare costs, F(46)=26.43; p<0.001 [36]. Thus those individuals with healthier lifestyle behaviors had lower subsequent medical expenses. Thus HRA’s and related intervention programs have might play a role in attenuating the economic impact of NCD’s on the economy.
Summary
The burden of NCD’s is increasing globally, however more so in low-middle-income countries. The workplace provides an opportune setting for health promotion programs which aim to address NCD’s and their risk factors. The HRA, can be regarded as the first step towards identifying employees who are at increased risk, and who might benefit from additional intervention programs.
Although there is some research emerging from Low Middle Income countries investigating the effectiveness of worksite health promotion programs, more research is warranted. Indeed, the World Economic forum has identified the need for additional research, particularly for countries other than the United States of America [12]. This research will contribute to comparing employee health metrics from different countries and sectors, in addition to providing Return on Investment (ROI) data that is context specific [12].
References
- Bloom DE, Cafiero ET, Jane´-Llopis E, Abrahams-Gessel S, Bloom LR, et al. (2011) The Global Economic Burden of Noncommunicable Diseases. Geneva: World Economic Forum. In. Edited by Forum WE. Geneva: Harvard School of Public Health.
- Beaglehole R, Bonita R, Alleyne G, Horton R, Li L, et al. (2011) UN High-Level Meeting on Non-Communicable Diseases: addressing four questions. Lancet 378: 449-455.
- Probst-Hensch N, Tanner M, Kessler C, Burri C, Künzli N (2011) Prevention--a cost-effective way to fight the non-communicable disease epidemic: an academic perspective of the United Nations High-level NCD Meeting. Swiss Med Wkly 141: w13266.
- Beaglehole R, Bonita R, Horton R, Adams C, Alleyne G, et al. (2011) Priority actions for the non-communicable disease crisis. Lancet 377: 1438-1447.
- Mayosi BM, Flisher AJ, Lalloo UG, Sitas F, Tollman SM, et al. (2009) The burden of non-communicable diseases in South Africa. Lancet 374: 934-947.
- Bull FC, Bauman AE (2011) Physical inactivity: the "Cinderella" risk factor for noncommunicable disease prevention. J Health Commun 16 Suppl 2: 13-26.
- Gregg EW, Gerzoff RB, Caspersen CJ, Williamson DF, Narayan KM (2003) Relationship of walking to mortality among US adults with diabetes. Arch Intern Med 163: 1440-1447.
- Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, et al. (2012) Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet 380: 219-229.
- McGuire KA, Janssen I, Ross R (2009) Ability of physical activity to predict cardiovascular disease beyond commonly evaluated cardiometabolic risk factors. Am J Cardiol 104: 1522-1526.
- World Health Organisaton WEF: Preventing non communicable diseases in the workplace through diet and physical activity: WHO/World Economic Forum report of a joint event. In. Geneva: World Health Organisation; 2008: 51.
- Kassi E, Pervanidou P, Kaltsas G, Chrousos G (2011) Metabolic syndrome: definitions and controversies. BMC Med 9: 48.
- WEF: Making the right investment: Employee health and the power of metrics. In. Edited by Alliance TWW: World Economic Forum; 2013.
- Soler RE, Leeks KD, Razi S, Hopkins DP, Griffith M, et al. (2010) A systematic review of selected interventions for worksite health promotion. The assessment of health risks with feedback. Am J Prev Med 38: S237-262.
- Pronk NP, Kottke TE (2009) Physical activity promotion as a strategic corporate priority to improve worker health and business performance. Prev Med 49: 316-321.
- Chapman LS (2012) Meta-evaluation of worksite health promotion economic return studies: 2012 update. Am J Health Promot 26: TAHP1-1TAHP12.
- Goetzel RZ, Pronk NP (2010) Worksite health promotion how much do we really know about what works? Am J Prev Med 38: S223-225.
- WHO: Global Health Risks: mortality and burden of disease attributed to selected major risks. In. Edited by Organisation WH. Geneva; 2009: 70.
- Ker J, Rheeder P, Van Tonder R (2007) Frequency of the metabolic syndrome in screened South African corporate executives. Cardiovasc J S Afr 18: 30-33.
- Kolbe-Alexander TL, Buckmaster C, Nossel C, Dreyer L, Bull F, et al. (2008) Chronic disease risk factors, healthy days and medical claims in South African employees presenting for health risk screening. BMC Public Health 8: 228.
- Patel D, Goetzel RZ, Beckowski M, Milner K, Greyling M, et al. (2013) The Healthiest Company Index: a campaign to promote worksite wellness in South Africa. J Occup Environ Med 55: 172-178.
- Ekblom-Bak E, Hellénius ML, Ekblom O, Engström LM, Ekblom B (2010) Independent associations of physical activity and cardiovascular fitness with cardiovascular risk in adults. Eur J Cardiovasc Prev Rehabil 17: 175-180.
- Katano S, Nakamura Y, Nakamura A, Murakami Y, Tanaka T, et al. (2010) Relationship among physical activity, smoking, drinking and clustering of the metabolic syndrome diagnostic components. J Atheroscler Thromb 17: 644-650.
- Mozumdar A, Liguori G (2011) Occupational physical activity and the metabolic syndrome among working women: a Go Red North Dakota study. J Phys Act Health 8: 321-331.
- Osilla KC, Van Busum K, Schnyer C, Larkin JW, Eibner C, et al. (2012) Systematic review of the impact of worksite wellness programs. Am J Manag Care 18: e68-81.
- Conn VS, Hafdahl AR, Cooper PS, Brown LM, Lusk SL (2009) Meta-analysis of workplace physical activity interventions. Am J Prev Med 37: 330-339.
- Anderson LM, Quinn TA, Glanz K, Ramirez G, Kahwati LC, et al. (2009) The effectiveness of worksite nutrition and physical activity interventions for controlling employee overweight and obesity: a systematic review. Am J Prev Med 37: 340-357.
- Serxner SA, Gold DB, Grossmeier JJ, Anderson DR (2003) The relationship between health promotion program participation and medical costs: a dose response. J Occup Environ Med 45: 1196-1200.
- Huskamp HA, Rosenthal MB (2009) Health risk appraisals: how much do they influence employees' health behavior? Health Aff (Millwood) 28: 1532-1540.
- Okie S (2007) The employer as health coach. N Engl J Med 357: 1465-1469.
- Taitel MS, Haufle V, Heck D, Loeppke R, Fetterolf D (2008) Incentives and other factors associated with employee participation in health risk assessments. J Occup Environ Med 50: 863-872.
- Colkesen EB, Kraaijenhagen RA, Frings-Dresen MH, Sluiter JK, van Kalken CK, et al. (2011) Participation in a workplace web-based health risk assessment program. Occup Med (Lond) 61: 586-589.
- Burton WN, Chen CY, Conti DJ, Schultz AB, Edington DW (2003) Measuring the relationship between employees' health risk factors and corporate pharmaceutical expenditures. J Occup Environ Med 45: 793-802.
- Pai CW, Hagen SE, Bender J, Shoemaker D, Edington DW (2009) Effect of health risk appraisal frequency on change in health status. J Occup Environ Med 51: 429-434.
- Kowlessar NM, Goetzel RZ, Carls GS, Tabrizi MJ, Guindon A (2011) The relationship between 11 health risks and medical and productivity costs for a large employer. J Occup Environ Med 53: 468-477.
- Yen L, McDonald T, Hirschland D, Edington DW (2003) Association between wellness score from a health risk appraisal and prospective medical claims costs. J Occup Environ Med 45: 1049-1057.
- Pronk NP, Lowry M, Maciosek M, Gallagher J (2011) The association between health assessment-derived summary health scores and health care costs. J Occup Environ Med 53: 872-878.
- Sattelmair J, Pertman J, Ding EL, Kohl HW 3rd, Haskell W, et al. (2011) Dose response between physical activity and risk of coronary heart disease: a meta-analysis. Circulation 124: 789-795.
- Bellow A, Epstein JF, Parikh-Patel A (2011) Lifestyle behaviors associated with secondary prevention of coronary heart disease among California adults. Prev Chronic Dis 8: A31.
- Shi L, Morrison JA, Wiecha J, Horton M, Hayman LL (2011) Healthy lifestyle factors associated with reduced cardiometabolic risk. Br J Nutr 105: 747-754.
- Barham K, West S, Trief P, Morrow C, Wade M, et al. (2011) Diabetes prevention and control in the workplace: a pilot project for county employees. J Public Health Manag Pract 17: 233-241.
- Engbers LH, van Poppel MN, van Mechelen W (2007) Modest effects of a controlled worksite environmental intervention on cardiovascular risk in office workers. Prev Med 44: 356-362.
- Groeneveld IF, Proper KI, van der Beek AJ, Hildebrandt VH, van Mechelen W (2011) Short and long term effects of a lifestyle intervention for construction workers at risk for cardiovascular disease: a randomized controlled trial. BMC Public Health 11: 836.
- MacKinnon DP, Elliot DL, Thoemmes F, Kuehl KS, Moe EL, et al. (2010) Long-term effects of a worksite health promotion program for firefighters. Am J Health Behav 34: 695-706.
- Pressler A, Knebel U, Esch S, Kolbl D, Esefeld K, et al. (2010) An internet-delivered exercise intervention for workplace health promotion in overweight sedentary employees: a randomized trial. Prev Med 51: 234-239.
- Prior JO, van Melle G, Crisinel A, Burnand B, Cornuz J, et al. (2005) Evaluation of a multicomponent worksite health promotion program for cardiovascular risk factors-correcting for the regression towards the mean effect. Prev Med 40: 259-267.
- Terry PE, Seaverson EL, Grossmeier J, Anderson DR (2011) Effectiveness of a worksite telephone-based weight management program. Am J Health Promot 25: 186-189.
Relevant Topics
- Child Health Education
- Construction Safety
- Dental Health Education
- Holistic Health Education
- Industrial Hygiene
- Nursing Health Education
- Occupational and Environmental Medicine
- Occupational Dermatitis
- Occupational Disorders
- Occupational Exposures
- Occupational Medicine
- Occupational Physical Therapy
- Occupational Rehabilitation
- Occupational Standards
- Occupational Therapist Practice
- Occupational Therapy
- Occupational Therapy Devices & Market Analysis
- Occupational Toxicology
- Oral Health Education
- Paediatric Occupational Therapy
- Perinatal Mental Health
- Pleural Mesothelioma
- Recreation Therapy
- Sensory Integration Therapy
- Workplace Safety & Stress
- Workplace Safety Culture
Recommended Journals
Article Tools
Article Usage
- Total views: 19587
- [From(publication date):
December-2013 - Jul 26, 2025] - Breakdown by view type
- HTML page views : 14652
- PDF downloads : 4935