Obstetric Brachial Plexus Injury (OBPI): Is Functional Electrical Stimulation (FES) a Viable Intervention Option?
Received: 19-Sep-2019 / Accepted Date: 06-Nov-2019 / Published Date: 13-Nov-2019 DOI: 10.4172/2165-7025.1000419
Abstract
An estimated 35,000 new-borns will acquire obstetric brachial plexus injury (OBPI) each year in the USA. Despite major advancements in early neurosurgical procedures resulting in peripheral re-innervation, the recovery process typically takes several years. The inability to activate the upper extremity (UE) muscles during this period results in severe atrophy, joints contracture, diminished peripheral blood flow, limbs length discrepancy, all contributing to impaired development of UE use during uni-and bilateral daily functions. Functional electrical stimulation (FES) augmentation of recovery after damage to the brain is document extensively in peer-reviewed rehabilitation literature. In contrast, FES is seldom considered a treatment option in OBPI. The primary reason is that in the absence of peripheral innervation, the efficacy of FES has been traditionally questioned. However, knowing that the majority of toddlers who underwent neurosurgical procedures will recover varying degrees of innervation, raise the question can FES help recover muscle strength of the re-innervated yet very weak muscles? This short communication focus on determining who is a candidate for FES training and how to utilize FES to enhance the recovery and functional use of the paretic UE of children with OBPI
Keywords: Functional electrical stimulation; Brachial plexus injury
Introduction
Among new-borns in the USA, the annual incidence of obstetric brachial plexus injury (OBPI) is about 0.9% resulting in estimated 35,000 new-borns with paralysis/paresis on the upper extremity (UE) [1]. For some babies full or almost full recovery of UE function is expected [2]. But for 20-30%, the normal development is impaired because the paretic UE undergo varying degrees of muscle atrophy, loss of joint range of motion in the gleno-humeral, “scapula-thoracic”, elbow, and wrist joints, resulting in limited use of the UE in daily functions [3]. Functional electrical stimulation (FES) is seldom considered in the management of OBPI [4]. One reason for not considering FES is the uncertainty of sufficient innervation of the atrophied, paretic muscles. This paper presents a novel clinical approach to screen babies and children with OBPI and develop a treatment plan for those who are candidate for FES intervention.
Methods
Screening
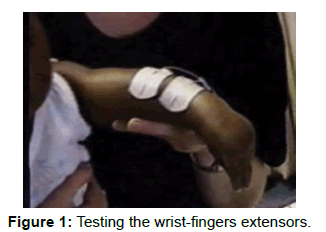
The stimulation parameters needed for screening include symmetric biphasic waveform pulse generator (FES); phase/pulse duration of 300- 600 microsec; 1-2 pulses per sec; and peak current intensity of no less than 100 mA. The electrodes are placed on each target muscle group (example the wrist-finger extensors as illustrated in Figure 1.
The stimulation intensity is increased rapidly looking for visible twitch contraction of the target muscles. The presence of twitch contractions indicates sufficient innervation to justify using FES to strengthen the tested muscle group. The testing is repeated on all paretic-atrophied muscles of the UE.
Testing of UE joints mobility
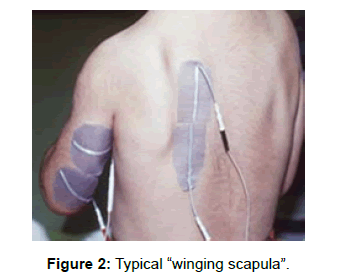
Limited active and particularly passive range of motion (PROM) are the primary impairments that prevent children with OBPI from using the UE [5,6]. Specifically, the limited PROM of the glenohumeral, elbow, and wrist joints must be documented during the initial screening. One exception to hypomobility is the hypermobility of the “scapula-thoracic” joint resulting in the typical “winging scapula” (Figure 2). Specifically, the unstable scapula protrudes, elevates, and internally rotates. The cause is damage to the subscapular and/or long thoracic nerves. The more unstable the scapula the less the chance of using the UE during reaching and over-head daily functions.
Intervention
Once the determination is made that the child is likely to benefit from FES, it is incorporated to enhance the recovery of muscle strength and motor control within the framework of normal development. For treatment purposes, the pulse rate is increased to induce tetanic contraction. Clinical experience suggests that unlike adults, in very young children (1-6 years) only 5-10 pulses per sec (5-10 Hz) may induce tetanic contraction. Accordingly, it is the clinical observation that determines the specific pulse rate needed to induce tetanic contraction in each muscle. In general, the pulse rate should be kept low to minimize the chance of muscle fatigue. Example of activities can be seen in Figure 3.
However, without restoring joints range of motion, FES is not likely to benefit children with OBPI. A critical component of the intervention is therefore to provide specific physical exercises to restore or maintain mobility of the gleno-humeral, elbow and if needed wrist joints’ range of motion. The hyper mobility of the “scapula-thoracic” joint as seen in Figure 2 cannot be improved substantially by exercises or FES. FES cannot induce contraction of the subscapularis and serratus anterior because they are covered by the scapula. At best, FES can activate the rhomboids and middle-lower trapezius as seen in Figure 2 and minimize scapular upward rotation/elevation during reaching activities. Firm stabilization of the markedly unstable scapula will most likely require surgery [7].
Results and Discussion
The first and only reported clinical data using FES to manage OBPI was published in 2016 [4]. The author compared a group that received 3 months of structured weight bearing exercise program to a group that received the same program combined with neuromuscular electrical stimulation. Mallet grading system and dual-energy x-ray absorptiometry were used to evaluate shoulder function and bone mineral density (BMD) respectively. Adding the stimulation program resulted in significantly better outcomes.
Conclusion
Babies and children with neuromuscular and functional deficits resulting from OBPI should be screened to determine candidacy for FES. If the testing indicates sufficient innervation, FES when combined with other developmental interventions, may enhance the recovery of muscle strength, motor control and functional use of the upper extremity.
References
- DeFrancesco CJ, Shah DK, Rogers BH, Shah AS (2019) The Epidemiology of Brachial Plexus Birth Palsy in the United States: Declining Incidence and Evolving Risk Factors. J Pediatr Orthop 39: e134-e140.
- Zuarez-Easton S, Zafran N, Garmi G, Hasanein J, Edelstein S, et al. (2017) Risk factors for persistent disability in children with obstetric brachial plexus palsy. J Perinatol 37: 168-171.
- Sjoberg I, Erichs K, Bjerre I (1988) Cause and effect of obstetric (neonatal) brachial plexus palsy. Acta Paediatr Scand 77: 357-364.
- Elnaggar RK (2016) Shoulder Function and Bone Mineralization in Children with Obstetric Brachial Plexus Injury after Neuromuscular Electrical Stimulation During Weight-Bearing Exercises. Am J Phys Med Rehabil 95: 239-247.
- Ruyer J, Grosclaude S, Lacroix P, Jardel S, Gazarian A (2018) Arthroscopic isolated capsular release for shoulder contracture after brachial plexus birth palsy: clinical outcomes in a prospective cohort of 28 children with 2 years' follow-up. J Shoulder Elbow Surg 27: e243-e251.
- Luszawski J, Marcol W, Mandera M (2017) The components of shoulder and elbow movements as goals of primary reconstructive operation in obstetric brachial plexus lesions. Neurol Neurochir Pol 51: 366-371.
- Mackenzie WG, Riddle EC, Earley JL, Sawatzky BJ (2003) A neurovascular complication after scapulothoracic arthrodesis. Clin Orthop Relat Res 408: 157-161.
Citation: Alon G (2019) Obstetric Brachial Plexus Injury (OBPI): Is Functional Electrical Stimulation (FES) a Viable Intervention Option? J Nov Physiother 9:419. DOI: 10.4172/2165-7025.1000419
Copyright: © 2019 Alon G. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3957
- [From(publication date): 0-2019 - Dec 11, 2025]
- Breakdown by view type
- HTML page views: 3017
- PDF downloads: 940