Occult Talar Fractures in Young Athletes: Case Report and Literature Review
DOI: 10.4172/2329-910X.1000322
Abstract
Talar fractures are uncommon injuries that are often misdiagnosed as usual ankle sprains. The diagnosis could be challenging only with a plain radiography and the computerized tomography scan could be the first exam reaching it. The consequences of a missed diagnosis are increased risk of persistent pain, non-union and degenerative changes. We present a case of a non-displaced talar neck fracture in an athlete diagnosed only after 7 days, and a case of a snowboarder fracture in a football player identified only at tenth day. Both cases had an acceptable clinical outcome, but the complications are neither uncommon nor neglectable.
Keywords: Talar fractures; Snowboarder fracture; Occult talar fractures; Avascular necrosis; Hawkins
Abbreviations
Computerized Tomography scan (CT scan); Weight Bearing (WB); Range of Motion (ROM); Avascular Necrosis (AVN)
Introduction
Talar fractures are uncommon injuries, accounting for <1%-4% of all foot fractures [1,2]. They are often misdiagnosed because its symptoms resemble those of an ankle sprain. The diagnosis could be challenging with a simple plain radiography, turning the computerized tomography (CT) scan the most indicated exam in case of high index of suspicion. Missed diagnosis and subsequent delayed or inadequate treatment increases the risk of persistent pain, disability, non-union and degenerative changes [1-4].
Cases Report
Case 1: Non displaced talar neck fracture in a young volleyball player
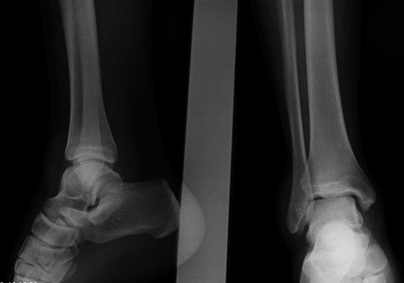
23 year old male volleyball player with history of acute inversion ankle sprain after a jump during a training session. The player immediately presented severe ankle pain and absolute disability to continue playing. He was transported to urgent department and at admission was unable to tolerate weight bearing (WB) and present a mild swelling without ecchymosis. The ankle radiographic series was negative and the athlete was discharged to home with instruction to follow RICE protocol (Figure 1). After 7 days, he was reassessed for sustained pain and repeated imaging study, including ankle CT scan (Figures 2 and 3). In CT scan was evident a Hawkins II talar neck fracture. An open reduction and internal fixation with 3 screws was performed, followed by 10 weeks of no weight bearing and active mobilization (Figure 4). At 10 weeks he had complete ankle range of motion (ROM) and started partial WB.
Case 2: Occult snowboarder fracture in a young football player
17 years old male football player with a left lateral process of talus fracture. After injury, the player referred severe pain and was unable to tolerate WB. In the emergency department he was clinically assessed and made an ankle radiographic series. On the radiography it was not evident any fracture or other articular abnormality (Figure 5). The diagnosis of ankle sprain was assumed. After 10 days, the player returned with sustained pain and non-tolerating partial WB. At that time, he repeated the radiography and made an ankle CT scan (Figure 6). The CT scan revealed a Hawkins type I fracture of the lateral process of the talus. We performed an open reduction and internal fixation with one lag screw of the talar lateral process (Figure 7). Postoperatively, a non WB short leg boot was applied for 6 weeks followed by a partial WB short leg boot for an additional period of 4 weeks. At 10 weeks the player was able to walk without any pain and with complete ROM.
Discussion
Fractures of the talus have a relatively low incidence accounting for <1% of all bone fractures and 3%-6% of all foot fractures [5]. They are easily misdiagnosed, missed or untreated because its early symptoms resemble an ankle sprain or a ‘soft tissue injury’. The plain radiograph is the first exam asked but it could not be enough. The CT scan is the most indicated exam in a high level of suspicion injury. An early and appropriate diagnosis and treatment could decrease the complications and morbidity of these fractures [2,6-8].
Neck talar fractures
Fractures of the neck of the talus are rare injuries representing <0.1% of all fractures, but accounting for 30 to 50% of all talar fractures [1,5,7,9,10]. The classically described mechanism of lesion is forced dorsiflexion of the ankle combined with axial loading. Most of the times they are associated to high energy traumas to the ankle (such as fallings from height or road traffic accidents), resulting in open injuries in nearly 20%-40% and over 50% of associated fractures [2,7,8,10].
The clinical presentation of a neck talar fracture could be indistinct from an ankle sprain which turns the diagnosis challenging. Nevertheless, most of these fractures are diagnosed by a simple plain radiography [1,5]. Anteroposterior, oblique and lateral radiographs of both the ankle and foot should be taken initially to improve the diagnosis rate and to assess the extension of the lesion [7]. Canale and Kelly described an x-ray view to better appreciate the talar neck: the foot is placed in maximum plantar flexion, with 15° of eversion and the beam with 75° angle to the horizontal in the sagittal plane [7,11].
Immediate reduction of displaced fractures, subluxations or dislocations at the initial presentation is the standard of care to preserve the soft tissue envelope and neurovascular structures. Recent literature has showed that the correlation of the risk of avascular necrosis (AVN) is greater with the degree of initial displacement than with the time from injury to surgical fixation. Therefore, reduction of the fracture is the most urgent thing to do, and the definitive stable osteosynthesis, could be delayed in favour of protection of the soft tissues, unless the fracture is irreducible and/or open [7,8].
However, occult fractures correspond to a significative ratio at the early assessment [1,5]. When clinical suspicion of neck fracture is high (prolonged symptoms and relevant bruise and swelling, etc.) another image study should be required as a CT scan [1,5,7]. A magnetic resonance imaging or a nuclear scintigraphy are not so helpful in the acute setting and should be left for assessment of talar vitality during follow up [1,8].
In the case of late or missed diagnosis, and subsequent improper treatment, the morbidity and the number of complications increase greatly [1]. The most prevalent complication is subtalar arthrosis which occurs in almost 50% of the cases. The prevalence of tibiotalar and talonavicular arthrosis also rounds one third of talar neck fractures. Malunion could happen in 25%-30% of the patients, but non-union is rare, accounting to less than 5%. One of the most feared is AVN which is very associated to this type of fracture occurring in nearly 30% of all talar neck fractures [5,7,10].
The vascularization pattern of the talus is peculiar. It has no muscular or tendinous attachments and thus relies on the integrity of its capsule for its blood supply which runs retrogradely by branches of the anterior tibial artery, posterior tibial artery and a perforating peroneal artery [1,7,8,10,12]. Therefore, an impairment of the blood supply of the head by a neck talar fracture have an increased risk of AVN. Injuries associated to medial malleolar fractures are less likely to develop AVN due to preservation of the deltoid ligament and the deltoid branch of the posterior tibial artery [8,9].
The rates of AVN correlate with the degree of initial dislocation [1,5,8,10,13]. Hawkins described a classification system of the talar neck and body fractures, later modified by Canale and Kelly, which provides descriptive and prognostic information [11,14]. Type I fractures are vertical, minimally displaced, with the subtalar joint reduced, and a reported rate of AVN of 0%-10%. Type II injuries include vertical, displaced fractures with the subtalar joint subluxated or dislocated, and are associated to AVN in 15%-20% of the cases. Type III fractures are similar to type II with the addition of dislocation of the ankle joint; a 30%-50% rate of AVN has been reported. Type IV fractures are neck talar fracture associated with dislocation of the ankle joint and dislocation or subluxation of the head of the talus from the talonavicular joint. The rate of AVN ranges from 10%-60% [7,10,13]. This variability could be partly explained by recent demonstration of a significative anterograde blood supply of the head and body whereby not all talar neck fracture evolve to osteonecrosis [7,15,16].
The treatment of a neck talar fracture is defined by the degree of dislocation. Most of the literature recommends short leg casting for type I fractures plus 6 to 12 weeks of non WB or until consolidation. It has also been described percutaneous fixation as a method for treatment of type I fractures with the possibility of early range of motion. Displaced type II-IV fractures almost all will require open reduction and internal fixation focusing on anatomic reduction and restoration of the peritalar joints, not depreciating the emergency character of reduction of open and/or dislocated fractures [1,5,7,8,17].
Snowboarder fractures
The fracture of the lateral process of the talus is thought to be an uncommon injury clinically resembling ankle sprains whereby they are frequently overlooked initially with between 30 and 60% of missed diagnosis [3,4,6].
In the physical exam, tenderness anterior and inferior to the tip of the lateral malleolus or a posterior subtalar effusion could be signs strongly suggestive and more specific of an occult lateral process fracture [3,6]. A Mortise or Broden’s view are also more sensitive than a standard radiograph, but the CT scan is the image technique of choice if fracture of the lateral process of the talus is suspected but plain radiographs are negative or inconclusive, especially in a patient with long term pain following an ankle injury [3,4,6].
This injury was rarely seen before snowboard became a popular sport in recent decades. In the general population, its incidence rounds less than 1% of talar fractures, but recent evidence shows a remarkably higher incidence in the snowboarders (some authors have pointed rates around 15%-30%) often associated with falls after high jumps associated to aerial manoeuvres [3,4,6,18]. Most authors describe the mechanism of trauma as an high energy trauma, with dorsiflexion and inversion in combination with a axial load, but, to date, the precise mechanism of injury has not been established as conflicting results could be found in the literature, with a possible role of eversion movement [2,3,4,19].
Lateral process fractures are classically classified by Hawkins in three types. Type I fractures are simple fractures with extension from the talofibular articular surface to the posterior talocalcaneal articular surface of the subtalar joint. Type II fractures are comminuted and involve not only the whole lateral process but also the fibular and posterior calcaneal articular surfaces of the talus. Type III injuries are chip fractures involving the anterior and inferior portion of the lateral process [3,4,6]. Type I fractures are the most common with a much greater incidence in low energy trauma, while type II and III are more associated with high energy falls/ traffic accidents [6].
Boack suggested another classification system for either lateral or posterior process fractures, where there are four types of fracture each again subdivided according to severity of bone injury, displacement, degree of chondral lesion and ligamentous stability. The arthroscopy appears as an indication for excision, chondral lesion assessment or osteosynthesis [2,6].
As the neck talar fractures, the treatment of this injury depends on the classification, degree of comminution and fracture displacement, but most of them require surgical treatment [2-4].
Type I lesions are usually treated with open reduction and internal fixation mostly in the event of large fragments (>20 mm) or more than 2 mm of displacement. If the fragment is displaced less than 2 mm this could be managed conservatively with casting; if it measures less than 5 mm, it should be managed as a Type II fracture and it could be excised arthroscopically [2,3]. Regardless the fixation type, surgically treated patients have less chance of develop significant symptoms or require later surgery than those treated conservatively [6].
Excision is the best option for type II fractures. Arthroscopy may have a role in fragment excision, joint debridement and assessment of chondral lesions [2,3]. In this type of injury, function is remarkably better and symptoms and need of late surgery are significantly less common after excision than casting [6].
Type III injuries have been shown to have good results with 6 weeks of protected WB and a cast [2,3]. The outcome of conservative treatment is very good with a minority of the patients being left with severe symptoms. There is also no statistically significant difference between casting or no treatment at all in what concerns to prolonged pain, but those treated with a cast have a significant lower risk of surgery [6].
Due to its resemblance to an ankle sprain, there is a high risk of morbidity if lateral process fractures are not managed timely and appropriately. Conservative treatment has been shown to have good outcomes in the majority of the cases but 60% evolves to non-union, while only 5% after a surgical treatment [2,20]. Whatever the treatment is, severe subtalar arthritis has been reported in 10%-15% of patients who had suffered a lateral process fracture [2,18].
Conclusion
Talar fractures could easily be missed given their resemblance to a usual ankle sprain and their small representation of the injuries treated by orthopaedic surgeons. A high index of suspicion is required in cases of severe acute ankle sprains or persistent ankle pain after previous ankle injury. CT scan could be the key in suspected cases. Early recognition and adequate treatment based on fracture type may reduce the associated morbidity and long term sequelae.
Conflict of Interest
We have no conflict of interests to disclose and the manuscript has been read and approved by all named authors.
Acknowledgement
We would like to thank Dr Afonso Ruano for the guidance during all the process and the incentive to publication, Dr António Andrade for writing assistance and proof reading, and all the members of the Orthopaedic Service of ULSNE, Bragança, Portugal for the support during this investigation.
References
- Mickel TJ, Andersen R, Keeling J, McKenna P (2008) Occult talar neck fracture associated with talar avulsion diagnosed by MRI: A case report. Foot Ankle Int. 29(9):956-958.
- Majeed H, McBride DJ (2018) Talar process fractures: An overview and update of the literature. EFORT Open Rev. 3(3):85-92.
- Kramer IF, Brouwers L, Brink PR, Poeze M (2014) Snowboarders' ankle. BMJ Case Rep.
- Boon AJ, Smith J, Zobitz ME, Amrami KM (2001) Snowboarder's talus fracture. Mechanism of injury. Am J Sports Med. 29(3):333-338.
- Perera A, Baker JF, Lui DF, Stephens MM (2010) The management and outcome of lateral process fracture of the talus. Foot Ankle Surg. 16(1):15-20.
- Whitaker C, Turvey B, Illical EM (2018) Current concepts in talar neck fracture management. Curr Rev Musculoskelet Med. 11(3):456-474.
- Rammelt S, Zwipp H (2009) Talar neck and body fractures. Injury. 40(2):120-135.
- Mechchat A, Bensaad S, Shimi M, Elibrahimi A. (2014) Unusual ankle fracture: A case report and literature review. J Clin Orthop Trauma. 5(2):103-106.
- Jordan RK, Bafna KR, Liu J, Ebraheim NA (2017) Complications of Talar Neck Fractures by Hawkins Classification: A Systematic Review. J Foot Ankle Surg. 56(4):817-821.
- Canale ST, Kelly FB (1978) Fractures of the neck of the talus. Long term evaluation of 71 cases. J Bone Joint Surg Am. 60(2):143-156.
- Bourton T, Sloan J (2003) Comminuted fracture of the talus not visible on the initial radiograph. Emerg. Med. J. 20.
- Alton T, Patton DJ, Gee AO (2015) Classifications in Brief: The Hawkins Classification for Talus Fractures. Clin Orthop Relat Res. 473(9):3046-3049.
- Hawkins LG (1970) Fractures of the neck of the talus. J Bone Joint Surg Am. 52(5):991-1002.
- Miller AN, Prasarn ML, Dyke JP, Helfet DL (2011) Quantitative assessment of the vascularity of the talus with gadolinium-enhanced magnetic resonance imaging. J Bone Joint Surg Am. 93(12):1116-1121.
- Prasarn ML, Miller AN, Dyke JP, Helfet DL (2010) Arterial anatomy of the talus: A cadaver and gadolinium enhanced MRI study. Foot Ankle Int. 31(11):987-993.
- Berlet GC, Lee TH, Massa EG (2001) Talar neck fractures. Orthop Clin North Am. 32(1):53-64.
- Valderrabano V, Perren T, Ryf C, Rillmann P (2005) Snowboarder's talus fracture: Treatment outcome of 20 cases after 3.5 years. Am J Sports Med. 33(6):871-880.
- Funk JR, Srinivasan SC, Crandall JR (2003) Snowboarder's talus fractures experimentally produced by eversion and dorsiflexion. Am J Sports Med. 31(6):921-928.
- Parsons SJ (2003) Relation between the occurrence of bony union and outcome for fractures of the lateral process of the talus:Â case report and analysis of published reports. Br. J. Sports Med. 37(3):274 - 276.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2232
- [From(publication date): 0-2021 - Oct 07, 2025]
- Breakdown by view type
- HTML page views: 1484
- PDF downloads: 748