Occupational Exposure to Blood and Body Fluids among Health Care Workers in Arada Sub-city Health Centers of Addis Ababa, Ethiopia
Received: 05-Oct-2018 / Accepted Date: 01-Nov-2018 / Published Date: 09-Nov-2018 DOI: 10.4172/2329-6879.1000281
Abstract
Background: Healthcare professionals (HCPs) are at high possibility of constricting blood-borne infections due to their occupation. The occurrence of these infections among HCPs is higher in low-income countries (e.g. Ethiopia). This study intended to examine the degree of occupational exposure (OE) to BBFs and its associated factors among HCPs in Arada Sub-city, Addis Ababa Ethiopia.
Methods: A cross-sectional study conducted from November 3, 2017, to December 19, 2017. Three hundred and sixty-one HCPs selected for study using a simple random sampling technique. The data were collected using a structured questionnaire and analyzed using SPSS version 20. To identify factors associated with blood and body fluids bivariate and multivariate analysis used.
Results: Among health, care professional one hundred and forty-nine, (41.3%) of had have exposure to BBFs in the past year. Profession (Nurse)0.76 [adjusted odds ratio (AOR)0.5, 95% confidence interval (CI) 0.26-0.98], Shortage of personal protective equipment (PPE) in the Past Year 1.99 (AOR 1.86, 95% CI1.11-3.11), Lack lifetime training on IP8.18(AOR 7.08, 95% CI 3.57-14.03) and not Using PPE 2.19 (AOR 2.25, 95% CI 1.3 -3.89) were among the factors associated with OE to BBFs.
Conclusions: This study shows a high proportion of HCP exposed to BBFs, Exposure to BBFs is observed in the practices carried out without proper equipment and standard precautions thus thereby ensuring the availability of proper equipment, proper training regarding the standard precautions and encouraging the HCPs to implement standard precautions to avoid such exposures.
Keywords: Occupational health; Health care professionals; Occupational exposure; Blood and body fluids; Infection prevention
Introduction
An occupational exposure that may place a worker to different infections; A percutaneous injury; either needle-stick or cut with sharp objects; or contact of mucous membrane; or contact of non-intact skin that is, chapped, abraded, or afflicted with dermatitis; with blood, tissue or other infectious body fluids [1,2].
Occupational health and safety are one of the most important aspects of human concern. It aims an adaptation of working environment to workers for the promotion and maintenance of the highest degree of the physical, mental and social well-being of workers in all occupations. Each year, work-related injuries and diseases kill an estimated 2 million people worldwide, which is greater than the global annual number of deaths from malaria. Annually, an estimated 160 million new cases of work-related diseases occur worldwide, including respiratory and cardiovascular diseases, cancer, hearing loss, musculoskeletal and reproductive disorders, mental and neurological illnesses [1,3].
Occupational exposure to blood and infectious body fluid remains a major occupational safety problem for healthcare workers (HCWs). Exposure to human BBFs poses at risk of blood-borne infections like hepatitis B, hepatitis C and human immunodeficiency virus (HIV). Body fluids are encountered during different medical interventions and are hence responsible for occupation-related HIV transmission [4,5].
Each year all most 6% of healthcare professionals percutaneous exposed to blood borne pathogens worldwide; out of the total exposure 2 million of those to HBV, 0.9 million to HCV and 170000 to HIV. This exposure may end up with infections in 15 000 HCV, 70 000 HBV, and 500 HIV. Most of the infections (which is 90%) through exposure occurred in developing countries [6,7].
These infections are preventable, as shown by the low rates achieved in certain countries that have engaged in serious prevention efforts, including training of HCW, HBV immunization, post-exposure prophylaxis, and improved waste management [6].
In Ethiopia, 30.5% of HCWs have a lifetime risk of needle stick injury and 25.7% sharp injury all over their career life but the lifetime risk of BBFs exposure was less than that of needle stick injury it accounts 28.8%.
In the year 2010, the prevalence of needle sticks injury in Ethiopia was 17.5% and sharp injury were 13.5%, but exposure to BBF was greater than both needle stick and sharp injury accounts 20.2% [8].
Factors for risky occupational practices among HCW had suboptimal practices and unfavorable attitudes related to standard precautions such as needle recapping (46.9%), high workload 44.3%, lack of protective barriers 33.3% and lack of knowledge on standard pre-cautions 17.8% [8,9]. CDC has proposed standard precautions (SPs), which are a series of procedures for preventing OE and for handling potentially infectious materials. HCPs are advised to follow SPs regularly, such as: observing regular personal hygiene; using protective barriers, e.g. gloves and gowns, whenever there is contact with the mucous membranes or BBFs of patients; and disposing of sharps and other clinical waste correctly [10,11]. Regardless of the implementation of safety measures prevention of exposure to BBFs still there is a problem of exposure to BBFs is existing [1]. This study will have a significant input in the formulation of appropriate strategy to modify and facilitate the overall prevention of OE to BBFs, for program planning and evaluation as well as baseline information for policymakers and regulatory bodies to improve the occupational safety in Health Facilities.
There were no adequate studies conducted to assess the occupational Blood and body fluid exposure in the sub-city so, that this study will be the source of information for future researchers.
Limitation of the study
The research was sensibly prepared, we are still aware of its limitations and shortcomings. First, the research conducted in the health center, which is the lowest level of the health care unit in the structure of the Ethiopian healthcare unit.
Second, self-Social desirability bias is also a potential limitation in self-reported studies like this one, and also there was no clear registration for occupational exposure to blood and body fluids, to minimize the problems items are included from other researchers for comparison. Additionally, during interpretation design, related limitation considered.
Methods
This study was undertaken in Arada sub city, Addis Ababa. From seven health centers there are 3702 health professionals in the sub-city. The study was conducted from November 3-December 19, 2017, Across-sectional study with an internal comparison. The sample size for the study was calculated using EPI info software version 7 unmatched case-control by assuming; P1=factors associated with BBFs exposure (Profession), P2=factors associated with BBFs (Age)(10) with a Confidence interval of 95%, Power 80%.
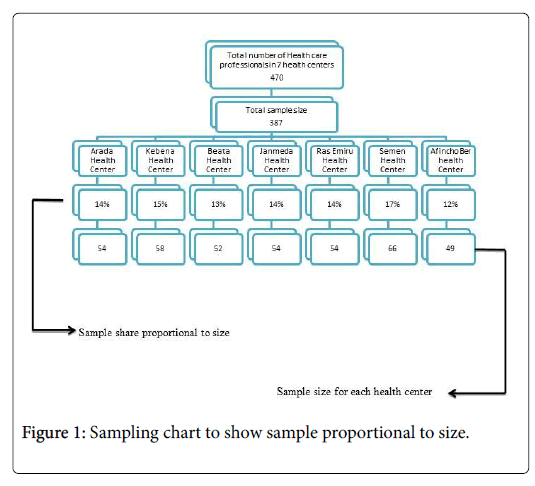
Finally, by adding a 10% non-response rate final sample size required 387 (Table 1 and Figure 1).
| Factors | %of controls exposed | %of cases exposed | CI | Power | Allocation ratio | Sample size for group 1 | Sample size for group 2 | Total sample size |
|---|---|---|---|---|---|---|---|---|
| Profession Midwifery | 1.85 | 10.04 | 95% | 80% | 01:02 | 77 | 154 | 231 |
| Age(< or =24) | 12.96 | 24.40 | 95% | 80% | 01:02 | 117 | 234 | 351 |
| Compliance with standard precaution | 60 | 73 | 95% | 80% | 01:02 | 99 | 198 | 297 |
Table 1: Showing Sample size for to assess occupational exposure to blood and body fluid exposure Arada sub city health center, Addis Ababa, Ethiopia, 2017.
The data from participants collected using a structured intervieweradministered questionnaire.
Data entry performed by using Epi Info version 7 and analysis performed using SPSS version 20.0 software (SPSS Inc., Chicago, IL, USA). After conducting a descriptive analysis for some variables, multivariate analysis made to observe the relative effect of independent variable on the dependent variable by controlling the effect of other variables. Only variables that reached a p-value less than 0.05 at the bivariate analysis level kept in the succeeding model.
Ethical clearance was first obtained from ethical clearance committee of Haramaya University and Addis Ababa health bureau. Thereafter ethical approval and written consent was submitted to the respective sub city and verbal consent was requested from all the participants during data collection. To ensure confidentiality names and other identity related information is not included.
Result
Three hundred seventy-one participants are participated, which gives 96% response rate. Ten incomplete questionnaires discarded, and the analysis based on the remaining 361 respondents.
Overall 143 of the HCPs (39.6%) were men. The mean age of the respondents was 27 ± 5.46 years. Most of the study participants, 49.3% were nurses, 22.7% were working in outpatient departments, and the mean overall working experience of the respondents had had 3.9 years (Table 2).
| Variable | No (%) of subjects (n = 361) |
|---|---|
| Sex | |
| Male | 143 (39.6) |
| Female | 218 (60.4) |
| Age group | |
| <24 | 118 (32.7) |
| 25-29 | 163 (45.2) |
| >30 | 80 (22.2) |
| Professional category | |
| Health Officer | 66 (18.3) |
| Nurse | 173 (47.9) |
| Midwife | 57 (15.8) |
| Lab Technician/Technologist | 33 (9.1) |
| Pharmacists | 26 (7.2) |
| Medical Doctor | 6 (1.7) |
| Current working department | |
| Regular OPD | 82 (22.7) |
| Emergency OPD | 49 (13.6) |
| Delivery Room | 65 (18) |
| Laboratory | 33 (9.1) |
| ART clinic | 26 (7.2) |
| Injection Room | 37 (10.2) |
| TB Room | 23 (6.4) |
| Other | 46 (12.7) |
| Work experience | |
| < or=2 years | 186 (51.5) |
| 3-5 years | 99 (27.4) |
| >or=6 Years | 76 (21.1) |
Table 2: Socio-demographic characteristics of health care professionals in Arada Sub City, Addis Ababa Ethiopia.
Magnitude of occupational exposure
Out of 361 study participants, 47.4 % (95% CI 42.1-52.1%) had been exposed to BBFs in their career. In the last 12 months, 41.3% (95% CI 42.1-52.1%) HCPs had exposed to BBFs. In this study, needle stick injuries over their professional career and in the past 12 months were reported by 26.3%, 18.3% of HCPs, correspondingly (Table 3).
| Variable | No (%) of subjects (n=361) |
|---|---|
| Lifetime occupational exposure to blood and body fluids | |
| Yes | 171 (47.4) |
| No | 190 (52.6) |
| Lifetime needle stick injury | |
| Yes | 95 (26.3) |
| No | 266 (73.7) |
| Past one year Occupational exposure to blood and body fluids | |
| Yes | 145 (40.2) |
| No | 216 (59.8) |
| Past one year Needle stick injury in the past year | |
| Yes | 66 (18.3) |
| No | 295 (81.7) |
Table 3: Occupational exposure to blood and body fluids among health care professionals in Arada Sub city, Addis Ababa.
In the past 12 months from exposed health care professionals, the majority were nurses (40.7%) and the rest were midwives (29%), health officers (17.9%), and laboratory technologists (12.4%).
Factors associated with occupational exposure
Most of the study participants had used gloves during health care procedure (73.1%) and 48 (13.3%) had training on infection prevention in the last 12 months. In the last 12 months, 58.2% of study participants had reported there were adequate PPE available. Almost half of the participants (52.4%) noticed posted safety signs in their health care facility. A total of 255 (70.6%) study participants know that there was an IP committee in the healthcare facility, although 189 (52.4%) reported that the workplace was not safe for the prevention of OE to BBFs (Table 4).
| Variable | No (%) of subjects (N=361) |
|---|---|
| Wearing of gloves during health care procedure n=359 | |
| Yes | 264 (73.1) |
| No | 95 (26) |
| Last one year Training on prevention of occupational infection | |
| Yes | 48 (13.3) |
| No | 313 (86.7) |
| Availability of PPE throughout the last year | |
| Yes | 136 (37.7) |
| No | 225 (62.3) |
| Presence of safety signs in health care institution | |
| Yes | 189 (52.4) |
| No | 172 (47.6) |
| Presence of an infection prevention committee in health care institution | |
| Yes | 255 (70.6) |
| No | 106 (29.4) |
| Workplace availability of guideline for prevention of occupational exposure to blood and body fluids | |
| Yes | 198 (54.8) |
| No | 163 (45.2) |
Table 4: Individual and institutional factors affecting prevention of occupational exposure to blood and body fluids among health care professionals in Arada Sub City, Addis Ababa Ethiopia 2017.
The materials in which most injuries occurred by surgical blade 43%, Solid needle 33%, hollow needle 20% and scissors 4% in the past year.
Measures taken after OE to blood and body fluid products were applying pressure, 36.13%, applying and washing with iodine 25.72%, get tested for HIV, 22.25%, seeking PEP 8.38%, Take tetanus antitoxoid (TAT) 3.9% and squeezing on the exposed parts of the body 3.3%.
Shortage of PPE in the last 12 months was one of the factors that contribute to the exposure of BBFs to HCPs. Health care professional who did not have training on IP in their career more likely to expose than who had have and also use of PPE for every clinical procedure and Profession of HCWs showed statistically significant associations with OE to BBFs in the past 12 months at a p <0.05. The experience of the HCPs, department of work age of the HCPs these also considered as the factors that contribute to OE to BBFs.
In multivariate analysis profession, the department, inadequate availability of PPE in the past 12 months, use of PPE on procedure and lifetime training on IP were significantly associated with OE to BBFs in the past 12 months. Those HCPs who had no prior training on IP were 8.18 [adjusted OR (AOR) 7.08, 95% CI 3.57-14.03] times more likely to be exposed to BBFs than those who had training on their carrier lifetime. Moreover, nurses were 50% less likely to have occupational exposure to BBFs than health officers were (Table 5).
| Variables | Occupational Exposure | Crude OR (95%CI) | Adjusted OR (95%CI) | |
|---|---|---|---|---|
| Yes | No | |||
| Sex | ||||
| Female | 86 | 132 | 1 | |
| Male | 63 | 80 | 1.21 (0.79-1.85) | |
| Age Group(Y) | ||||
| <24 | 54 | 64 | 1 | |
| 25-29 | 67 | 96 | 0.83 (0.51-1.33) | |
| >= 30 | 28 | 52 | 0.64 (0.36-1.45) | |
| Working experience(Y) | ||||
| <2 | 82 | 104 | 1 | |
| 05-Mar | 35 | 64 | 0.69(0.42-1.15) | |
| >=6 | 17 | 15 | 0.92 (0.54-1.58) | |
| Profession | ||||
| Health officer | 26 | 40 | 1 | |
| Nurse | 59 | 119 | 0.76 (0.43-1.37) | 0.50 (0.26-0.98)* |
| Midwife | 42 | 16 | 4.04 (1.89-8.62)*** | 1.49 (0.62-3.55) |
| Lab professional | 18 | 15 | 1.85(0.79-4.29) | 0.86(0.33-2.26) |
| Shortage of PPE in the past year | ||||
| No | 72 | 138 | 1.99 (1.30-3.06)*** | 1.86 (1.11-3.11)* |
| Yes | 77 | 74 | 1 | |
| Ever had training on IP | ||||
| Yes | 13 | 93 | 1 | |
| No | 136 | 119 | 8.18 (4.35-15.36)*** | 7.08 (3.57-14.03)*** |
| Use of PPE | ||||
| Yes | 88 | 161 | 1 | |
| No | 61 | 51 | 2.19 (1.39-3.44)*** | 2.25 (1.3-3.89)** |
| Note: The P value >0.05 were not included in multivariate analysis. | ||||
| *P<0.05, **P<0.01, ***P<0.005 | ||||
| Personal protective equipment’s: Glove, Goggles, Boots, Apron Infection prevention |
Table 5: Factors associated with occupational exposure to blood and body fluids among HCPs of Arada sub city.
The reasons for OE to BBFs were during childbirth (35%); the abrupt motion of a patient during blood draw or during the intramuscular or venous injection of drugs (31%); during the handling and collection of waste (10%) and during needle recapping (16%).
Discussion
In this study, 47.4% (95% CI 42.1-52.1%) HCPs were exposed to BBBs in their lifetime and 41.3% (95% CI 42.1-52.1%) of healthcare professionals were exposed to BBFs within last one year.
The main factors for the exposure to BBFs were the profession of the HCW, which had a significant impact; shortage of PPE in the last one year had places HCPs 1.8 times more risk of exposure of BBFs. Besides the shortage of PPE, not using PPE for every procedure had also an impact on the exposure of HCPs to BBFs and HCPs who had no training on IP had also a significant association between exposure of BBFs.
Half of the study participants (47.4 % (95% CI 42.1-52.1%)) had exposed to BBFs in their professional career, which is lower than findings from China (66%), Serbia (66%), Iran (74%), Turkey (64%), India (73%), Nigeria (68.9), Mali (64.1) and Kenya (71%). This difference was occurring because of the facility’s which are selected in this study were only from Health centers (primary health care units) but in the case of the other studies, HCP was selected from hospitals [12-16].
In the last one year, 41.3% (95% CI 42.1-52.1%) of healthcare workers had exposed to BBFs in this study, which is lower than the findings from Bahir Dar and Tanzania study, which is 65.9% and 47.9 respectively, but it was higher than study from Uganda (33.87%) and it was much higher than study in Kenya which is 25%. This discrepancy may occur due to the difference between the study area which is in this study the study participants were selected from only from urban health centers, but in the case of Bahir Dar study HCPs were selected from both urban and rural health centers [10,17-19].
Out of HCP which are exposed to BBFs, most of them are nurses (40%), which is the same as findings from the study in Taiwan but it is lower than the findings in Nigeria (50%). According to this study, there is no statistically significant difference across the HCPs, except for Nurses. However, in this study Nurses were 50% safer than health officers were. This discrepancy may be due to the difference in their number and the type of their department [20,21].
Fifty-one percent of the study participants are aware of the availability of PPE throughout the last 12 months, which is equivalent to the Bahir Dar study (51%) [10].
This study also revealed that 69% HCPs have used PPE in the last health care procedure which is lower than studies from Dire Dawa (85%) and better than a study from Bahir Dar (54%) this discrepancy may occur due to shortage of PPE and attitudes of HCP towards using PPE for every procedure. HCPs who did not use PPE for all health care procedure were 2.19 (AOR 2.29, 95% CI1.33-3.95) times more likely to be occupationally exposed to BBFs than those who were using PPE during a health care procedure in the last one year [8,10].
Only 29.4% of the respondents reported that they had had training on IP in this study, which less compared to study, finding from eastern Ethiopia (39%), Tanzania (73.1%) and Kenya (50.81%) this variation could be due to attention is given by healthcare administrator [8,17,19]. The lack of Regular infection prevention training may be the reason behind this variation.
The main factors for the OE to BBFs that identified in this study were a profession, inadequate training on infection prevention, department of work and persistent use of PPE most of the factors were comparable with the studies in Bahir Dar and Dire Dawa [8,10].
This study found a high number of OE to BBFs among HCPs in Arada sub city health centers. The main reasons, which identified in this study for the high number of exposures to BBFs, are the availability of PPE in the facilities, the consistent use of PPE, and training on IP. Therefore, providing training on IP to HCPs and always availing PPE may reduce the number of exposures.
References
- https://www.cartercenter.org/resources/pdfs/health/ephti/library/lecture_notes/env_occupational_health_students/ln_occ_health_safety_final.pdf
- WHO (2007) Post-exposure prophylaxis to prevent HIV Infection: Joint WHO. ILO Guidelines on post-exposure prophylaxis (PEP) to prevent HIV infection.
- Armstrong TW, Liang Y, Hetherington Y, Bowes III SM, Wong O, et al. (2011) Retrospective occupational exposure assessment for case-control and case-series epidemiology studies based in Shanghai China. J Occup Environ Hyg 8: 561-572.
- Hajjaji MD, Chaabouni T, Jmal KH, Messadi FA, Abdennadher M, et al. (2014) Occupational blood exposure among health care personnel and hospital trainees. Int J Occup Environ Med 5: 57-61.
- Alemie GA (2012) Exploration of healthcare workers’ perceptions on occupational risk of HIV transmission at the University of Gondar Hospital, Northwest Ethiopia. BMC Res Notes 5: 704.
- World Health Organization. (2002) The world health report 2002: Reducing risks, promoting healthy life. World Health Organization.
- Bartlett JG (2006) USPHS updates occupational HIV post-exposure prophylaxis guidelines. The Hopkins HIV report: A bimonthly newsletter for healthcare providers 18: 10-11.
- Reda AA, Fisseha S, Mengistie B, Vandeweerd JM (2010) Standard precautions: Occupational exposure and behavior of health care workers in Ethiopia. PLoS One 5.
- Tebeje B, Hailu C (2010) Assessment of HIV post-exposure prophylaxis use among health workers of governmental health institutions in Jimma Zone, Oromiya Region, Southwest Ethiopia. Ethiop J Health Sci 20: 55–64.
- Yenesew MA, Fekadu GA (2014) Occupational exposure to blood and body fluids among health care professionals in Bahir Dar town, Northwest Ethiopia. Safety and health at work 5: 17-22.
- Kermode M, Jolley D, Langkham B, Thomas MS, Crofts N, et al. (2005) Occupational exposure to blood and risk of bloodborne virus infection among health care workers in rural north Indian health care settings. Am J Infect Control 33: 34-41.
- Naderi H, Sheybani F, Bojdi A, Mostafavi I, Khosravi N, et al. (2012) Occupational exposure to blood and other body fluids among health care workers at a university hospital in Iran. Workplace Health Saf 60: 419-422.
- Sofola OO, Folayan MO, Denloye OO, Okeigbemen SA (2007) Occupational exposure to bloodborne pathogens and management of exposure incidents in Nigerian dental schools. J Dent Educ 71: 832-837.
- Koné MC, Mallé KK (2015) Blood exposure accidents: Knowledge and practices of hospital health workers in Mali. Bull Soc Pathol Exot 108: 369-372.
- Snell SA, Shadur MA, Wright PM (2000) Human resources strategy: The era of our ways.
- Mbaisi EM, Wanzala P, Omolo J (2013) Prevalence and factors associated with percutaneous injuries and splash exposures among health-care workers in a provincial hospital, Kenya. Pan Afr Med J 14: 14:10.
- Kumakech E, Achora S, Berggren V, Bajunirwe F (2011) Occupational exposure to HIV: A conflict situation for health workers. Int Nurs Rev 58: 454-462.
- Mashoto KO, Mubyazi GM, Mohamed H, Malebo HM (2013) Self-reported occupational exposure to HIV and factors influencing its management practice: a study of healthcare workers in Tumbi and Dodoma Hospitals, Tanzania. BMC Health Serv Res 13: 276.
- Hsieh WB, Chiu N, Lee C, Huang F (2006) Occupational blood and infectious body fluid exposures in a teaching hospital: a three-year review. Journal of Microbiology Immunology and Infection 39: 321.
- Umar AG, Aisha A (2017) Common occupational health hazards amongst Health care workers in a Tertiary Health Institution in Bida, North-central Nigeria. Int J Biomed Res 8: 1–6.
Citation: Amerga EW, Mekonnen TG (2018) Occupational Exposure to Blood and Body Fluids among Health Care Workers in Arada Sub-city Health Centers of Addis Ababa, Ethiopia. Occup Med Health Aff 6: 281. DOI: 10.4172/2329-6879.1000281
Copyright: © 2018 Amerga EW, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4645
- [From(publication date): 0-2018 - Nov 20, 2025]
- Breakdown by view type
- HTML page views: 3671
- PDF downloads: 974