Review Article Open Access
Occupational Lung Diseases among Soldiers Deployed to Iraq and Afghanistan
Anthony M Szema1,2*1New York State Center for Biotechnology Stony Brook University School of Medicine, Stony Brook, NY 11794, USA
2Chief, Allergy Section, Veterans Affairs Medical Center, Northport, NY, 11768, USA
- *Corresponding Author:
- Anthony M Szema
Assistant Professor of Medicine and Surgery
Principal Investigator, New York State Center for Biotechnology
Stony Brook University School of Medicine
Stony Brook, NY 11794, USA
E-mail: anthony.szema@stonybrookmedicine.edu
Received date: March 20, 2013; Accepted date: May 20, 2013; Published date: May 22, 2013
Citation: Szema AM (2013) Occupational Lung Diseases among Soldiers Deployed to Iraq and Afghanistan. Occup Med Health Aff 1:117. doi: 10.4172/2329-6879.1000117
Copyright: © 2013 Szema AM. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Occupational Medicine & Health Affairs
Abstract
Military personnel deployed to Iraq and Afghanistan, from 2004 to the present, has served in a setting of unique environmental conditions. Among these are exposures to burning trash in open air “burn pits” lit on fire with jet fuel JP-8. Depending on trash burned--water bottles, styrofoam trays, medical waste, unexploded munitions, and computers--toxins may be released such as dioxins and n-hexane and benzene. Particulate matter air pollution culminates from these fires and fumes. Additional environmental exposures entail sandstorms (Haboob, Shamal, and Sharqi) which differ in direction and relationship to rain. These wars saw the first use of improvised explosive devices (roadside phosphate bombs),as well as vehicle improvised explosive devices (car bombs), which not only potentially aerosolize metals, but also create shock waves to induce lung injury via blast overpressure. Conventional mortar rounds are also used by Al Qaeda in both Iraq and Afghanistan. Outdoor aeroallergens from date palm trees are prevalent in southern Iraq by the Tigris and Euphrates rivers, while indoor aeroallergen aspergillus predominates during the rainy season. High altitude lung disease may also compound the problem, particularly in Kandahar, Afghanistan. Clinically, soldiers may present with new-onset asthma or fixed airway obstruction. Some have constrictive bronchiolitis and vascular remodeling on open lung biopsy - despite having normal spirometry and chest xrays and CT scans of the chest. Others have been found to have titanium and other metals in the lung (rare in nature). Still others have fulminant biopsy-proven sarcoidiosis. We found DNA probe–positive Mycobacterium Avium Complex in lung from a soldier who had pneumonia, while serving near stagnant water and camels and goats outside Abu Gharib. This review highlights potential exposures, clinical syndromes, and the Denver Working Group recommendations on post-deployment health.
Keywords
Burn pits; Aeroallergenaspergillus; Bronchiolitis; Mycobacterium avium complex
Abbreviations
IED: Improvised Explosive Device; VIED: Vehicle Improvised Explosive Device; MAC: Mycobacterium Avium Complex; ABPA: Allergic Broncho Pulmonary Aspergillosis; CHUS: Containerized Housing Units; IAW-LI; Iraq Afghanistan War Lung Injury
Summary for Table of Contents
Occupational lung diseases have emerged as a problem among soldiers deployed to Iraq and Afghanistan. Clinical presentations are different from prior wars and require pulmonologists to have an enhanced knowledge base regarding concepts such as burn pits, improvised explosive devices, blast overpressure, sandstorms and allergy. Denver Working Group recommendations offer a framework for evaluating war fighters with Iraq Afghanistan War Lung Injury (IAW-LI).
Introduction
For a variety of reasons, U.S. soldiers deployed to Iraq between the years 2004-2011, and Afghanistan from 2004-present, have been assigned extended or multiple tours of duty, often 1 year or longer at a time. As a result, they have been increasingly exposed to unfavorable environmental conditions, which are dusty and harsh.
For most of the Iraq war, widespread use of incinerators was not available, and at the largest air base in Balad, a ten acre open air burn pit operated daily by burning all trash between 2003-December 2009, lit by jet fuel called JP-8 (Figure 1, Fumes from Camp Anaconda, Balad, Iraq). In Afghanistan, there are many small bases without incinerators, so trash is burned with JP-8 in burn pits as well, leading to aerosolized particulate matter air pollution. JP-8 releases benzene when burned at low heat without incinerators. Depending on the substances burned, dioxins and n-hexane may be aerosolized, for example, during the burning of plastic water bottles, styrofoam breakfast trays, medical waste, unexploded munitions, electronic devices/computers.
This era of warfare also led to the use of roadside Improvised Explosive Devices (IEDs) and VIEDS (vehicles loaded with explosives) by the insurgency, resulting in detonation of vehicles, which aerosolizes metal. Blast overpressure is from shock waves due to explosions and can lead not only to traumatic brain injury (TBI), but also lung injury, since the delicate alveoli or air sacs are tethered and susceptible to shear stress.
Endogenous environmental conditions of this habitat also entail sandstorms traveling horizontally, called Haboob-often very intense and associated with rain. These Haboobs are in a gravity current, a primarily horizontal flow in a gravitational field that is driven by a density differences. In Iraq, dust storms are so frequent that the language employs different terms describing the direction of the storm, e.g. :1) Northern seasonal dust storm, “shamali” ( ىلامش ) and 2) Easterly season dust storm, “sharqi” ( ىقرش ) which literally means Eastern. (Figure 1, Al Asad, Iraq, dust storm). These ambient conditions are unique and are dramatically different from the usual conditions that soldiers are exposed to in the U.S. The average rainfall in Iraq is low (per annum) during the summer, leading to dry soil and dust-filled air. However, during the winter season, it rains [1].
The most common outdoor aeroallergen in Iraq is date palm pollen in spring. Date palm trees have been cultivated in southern Iraq, along the banks of the Tigris and Euphrates rivers, for five thousand years (ancient Mesopotamia) [1]. Outdoor aeroallergens, including spring date palm pollen may trigger asthma and allergic rhinitis leading to cough.
The most common indoor aeroallergen is Aspergillus, a causative agent of Allergic Broncho Pulmonary Aspergillosus (ABPA), associated with asthma. Inhalation of small (<5 μm) particulatematter air pollution dust can trigger asthma, even in the absence of allergic sensitization. Indeed, massive disasters such as the World Trade Center collapse led to finding even 10 μm-sized particles in lung.
Blast overpressure entails shock waves to the chest during an explosion. These shock waves exert shear stress on delicately tethered alveolar air sacs in lung to cause lung injury. It is plausible that those soldiers with Traumatic Brain Injury also have blast overpressure to the lung [2,3].
Continuous exposure to indoor dust in humidified Containerized Housing Units (CHUs), especially during the rainy season, may lead to allergic sensitization to dust mite antigens, which are risk factors for asthma [4]. Soldiers also report asbestos and mold in old buildings constructed during the Saddam Hussein era, which are sometimes used to house troops on maneuvers. Sick building syndrome and asbestosrelated lung disease may be sequellae of these exposures (Figure 3).
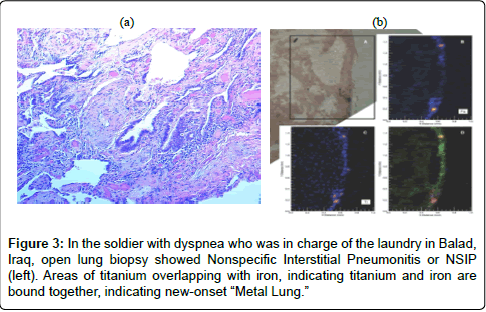
Due to the chaotic nature of war, some soldiers with pneumonia may be stoic and untreated; or, their disease is not recognized. We have detected positive DNA probes for Mycobacterium Avium Complex (MAC) in lung biopsy tissue from a soldier with pneumonia who was untreated. In another soldier who was in charge of the laundry in Balad, diagnosed with Nonspecific Interstitial Pneumonitis (NSIP), we actually found a bronchiolocentric pattern on closer examination, and later detected titanium, iron, and copper in his lung tissue with specialized testing, using Brookhaven National Laboratory’s National Synchrotron Light Source [3].
The energy dispersive X-ray figure indicates that iron and titanium are in such high abundance that they are more of these metals than calcium, which is normally distributed throughout the lung. (Figure 2a and 2b, Micro-X-ray fluorescence methods and biopsy of lung with titanium present)
An additional soldier with previously normal radiographic imaging had masses which were culture negative granulomatous lesions, suggestive of sarcoidosis. Whether the fires triggered this or if he was destined to get this is unknown, but is eerily similar to firefighters in New York City who had elevations of sarcoidosis diagnoses after 9/11, which has subsided since then [5].
Sentinel Studies of New-Onset Asthma Post- Deployment
Our earlier work was based on the finding that 14%of medic visits in Iraq were due to respiratory complaints according to a personal communication from Michael E. Kilpatrick, M.D., Deputy Director for Force Health Protection and Readiness Programs in the Office of the Assistant Secretary of Defense for Health Affairs. The Millennium Study of soldiers in Iraq later confirmed these findings of 14% of soldiers with respiratory symptoms while in Iraq and Afghanistan [6].
Since June 4, 2004, asthma diagnosed after the age of 13 has been an exclusion criterion for military enlistment. Therefore, no U.S. military personnel enrolled since that date should have asthma in the absence of a medical waiver. This means that asthma should be diagnosed less often than in the general population.
We hypothesized that deployment to Iraq is a risk factor for asthma. We expected to find high asthma rates among soldiers serving in Iraq. We analyzed data retrospectively from the Northport Veterans Affairs Medical Center, and compared asthma rates in U.S. Iraq War Veterans to those rates in veterans who never served in Iraq. We analyzed computer records of 6,233, 18-45-year-old subjects who served and were discharged between 3/1/04-5/1/07. The subjects were identified from a computerized database and stratified based on whether they had prolonged deployment to Iraq (≥ 1 year) or were stationed in the United States. Asthmatic soldiers were further classified by International Classification of Disease (ICD) codes for asthma. Possible correlation between deployment and disease status was evaluated [1].
All patients were examined by Northport VAMC physicians. The clinical guidelines at the VAMC clinic for a diagnosis of asthma include:
Presence of respiratory symptoms (cough, wheeze, dyspnea, exercise-induced shortness of breath).
Spirometric evidence of airway obstruction with decreased FEV1/ FVC or FEF25-75.
Improvement of symptoms and FEV1 after bronchodilators.
Based on these criteria, soldiers deployed to Iraq were diagnosed with asthma more often than stateside soldiers (6.6% vs. 4.3%, with a crude Odds Ratio (OR) = 1.58, 95% Confidence Interval (CI) = 1.18- 2.11. The same conclusions apply when subjects are stratified by gender and age groups.
When stratified by age groups, the higher risk for asthma still holds. For men, the odds ratios of deployment were significant in the 26-30-year-old and 36-40 year-old age groups (Table 4). The same female age groups also showed higher risks of asthma, though the ORs were not statistically significant because of smaller sample sizes.
In the 45 subjects with numerical VA data, spirometric measurements were collected while subjects were taking asthma medications and showed reduced values (Table 5). 3 of 9 without spirometry were skin prick test + dust mite antigens (with one of these subjects + cat and another + dog). All of these three atopic patients noted wheezing when they contacted dust or their other agent noted on + skin test.
| FVC | 4.76±1 L |
| FEV1 | 3.49±0.19 L |
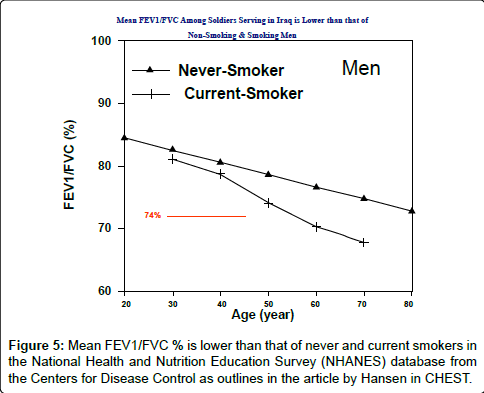
| FEV1/FVC | 74±5% |
Table 5: Mean FEV/FVC ratio percentage predicted values among soldiers diagnosed with asthma is reduced at 74%.
This mean value of FEV/FVC<80% is lower than that of both never and current smokers in the National Health and Nutrition Examination Survey (NHANES) from the Centers for Disease Control (CDC). (Figure 4 and 5)
| Age group (Year) | Deployment Status | Female (n=1453) | Male (n=4780) | ||||
| Asthma | No Asthma | OR (95% CI) | Asthma | No Asthma | OR (95% CI) | ||
| ≤ 25 | Persian Gulf | 1 | 21 | 0.91 | 14 | 272 | 1.67 |
| U.S. | 12 | 229 | [0.11, 7.34] | 18 | 585 | [0.82, 3.41] | |
| 26-30 | Persian Gulf | 1 | 16 | 1.96 | 15 | 242 | 2.22 |
| U.S. | 10 | 313 | [0.24, 16.24] | 22 | 787 | [1.13, 4.34] | |
| 31-35 | Persian Gulf | 1 | 11 | 1.74 | 6 | 97 | 1.49 |
| U.S. | 12 | 230 | [0.21, 14.63] | 25 | 603 | [0.60, 3.73] | |
| 36-40 | Persian Gulf | 1 | 5 | 7.06 | 10 | 87 | 2.44 |
| U.S. | 7 | 247 | [0.73, 68.63] | 37 | 784 | [1.17, 5.07] | |
| >40 | Persian Gulf | 1 | 9 | 1.54 | 11 | 99 | 1.74 |
| U.S. | 22 | 304 | [0.19, 12.67] | 64 | 1002 | [0.89, 3.41] | |
| Homongeneity test (across different age groups) | P-Value | P-Value | |||||
| 0.71 | 0.90 | ||||||
| 0.96 | |||||||
| Crude OR (all age groups) | 1.69 [0.66, 4.36] | 1.60 [1.17, 2.18] | |||||
| 1.58 [1.18, 2.11] | |||||||
| Mantel-Haenszel Common OR (95% CI) | 1.70 [0.66, 4.40] | 1.90 [1.37, 2.63] | |||||
| 1.88 [1.38, 2.56] | |||||||
Table 4: Odds ratio of being diagnosed with asthma is high among 26-40 year-olds, with those 36-40 having the greatest risk: sevenfold.
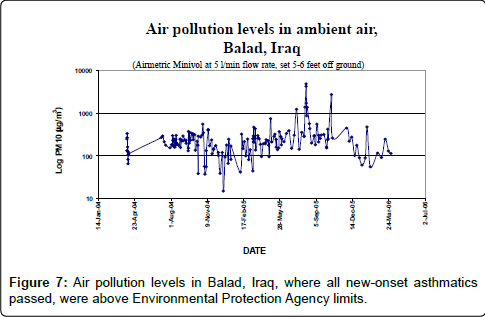
Air pollution levels in Balad, Iraq, (Figure 6) during this time frame from 2007-7, where all subjects in the study were confirmed to have passed through, were higher than Environmental Protection Agency limits of 35 μg/m3. Indeed, levels were, for the most part over 100 and exceeded 1000 on occasion. These data support an etiologic mechanism for why deployment to Iraq is associated with an increased likelihood of being diagnosed with asthma. The Institute of Medicine report on burn pits also suggests high levels of particulate matter were in ambient air [1]. Particulate matter air pollution in and of itself is associated with both cardiovascular and respiratory disease [7-14].
New-Onset Respiratory Symptoms after Deployment to Iraq and Afghanistan
A follow-up study published in the JOEM looked at rates of spirometry among soldiers either deployed to Iraq/Afghanistan or elsewhere. Spirometry is ordered in the VA system after a patient complains of respiratory symptoms which are recognized by the health care provider, who indicates symptoms in a compute entry box as well as an ICD code diagnosis. A request is sent to the pulmonary fellow who approves the test. Patients have to return on either of two spirometry screening days per month. The data is later interpreted and scanned into the computerized patient record system. These hurdles, at once, lead to underestimation of the scope of the problem, since there is noncompliance with follow-up to get the test, this system does not count abnormal spirometry conducted by pulmonologists outside the VA, and completed spirometries, despite interpretation by a pulmonary attending physician and fellow are not counted until the information technology branch scans in the raw data [4].
While there were more smokers in the Iraq/Afghanistan group vs. all others, 16.1% vs. 3.3%, a multivariate analysis excluded smoking as a risk factor for obtaining a spirometry or having abnormal values. Higher rates of post-traumatic stress disorder and traumatic brain injury are in the Iraq/Afghanistan group. PTSD is associated with asthma among monozygotic twins and may be related to cytokine release. Traumatic brain injury may also be associated with blast overpressure to the chest from the same explosion to the head (Tables 6-8).
| Iraq/Afghanistan (n=1816) | Non Iraq/Afghanistan (n=5335) | p-value* | |
| Age (year): mean (std dev) | 33.85 (9.23) | 35.38 (10.08) | <0.001 |
| Smoker: n (%) | 292 (16.1) | 178 (3.3) | <0.001 |
| Diagnosed with asthma: n (%) | 113 (6.2) | 38 (0.7) | <0.001 |
| With spirometry: n (%) | 263 (14.5) | 98(1.8) | <0.001 |
| Female: n (%) | 158 (8.7) | 918 (17.2) | <0.001 |
| TBI: n (%) | 499 (27.5) | 219 (4.1) | <0.001 |
| PTSD: n (%) | 610 (33.6) | 198(3.7%) | <0.001 |
Table 6: Comparisons of veterans deployed to Iraq/Afghanistan vs. those were not.
| With Spirometry (n=361) | Without Spirometry (n=6790) | p-value* | |
| Age (year): mean (std dev) | 37.04 (10.85) | 34.88 (9.83) | <0.001 |
| Smoker: n (%) | 126 (34.9) | 344 (5.1) | <0.001 |
| Deployed in Iraq/Afghanistan: n (%) | 263 (72.9) | 1553(22.9) | <0.001 |
| Female: n (%) | 47 (13.0) | 1029 (15.2) | <0.001 |
| TBI: n (%) | 334 (92.5) | 384 (5.7) | <0.001 |
| PTSD: n (%) | 153 (42.4) | 655 (9.6) | <0.001 |
Table 7: Comparisons of veterans with vs. without a spirometry evaluation.
| Non Iraq/Afghanistan (n=98) | Iraq/Afghanistan (n=263) | p-value | |
| Age (year) | 38.67 (11.92) | 36.43 (10.37) | 0.11 |
| Height (in) | 68.90 (3.60) | 69.10 (3.29) | 0.64 |
| Weight (pd) | 193.30 (35.45) | 193.75 (34.39) | 0.92 |
| FEV1 | 3.43 (0.87) | 3.68 (0.79) | 0.009 |
| FVC | 4.44 (1.14) | 4.73 (0.94) | 0.029 |
| FEV1/ FVC | 77.53 (7.99) | 77.97 (7.42) | 0.63 |
Table 8: Comparision of means (standard deviations) of FEV1, FVC, FEV1/ FVC, at rest, age, height and weight between veterans in the two groups who had spirometry.
Constrictive Bronchiolitis after Deployment to Iraq
In this descriptive case series from Matt King and Robert Miller at Vanderbilt University, 80 soldiers from Fort Campbell, Kentucky, with inhalational exposures during service in Iraq and Afghanistan were evaluated for dyspnea on exertion that prevented them from meeting the U.S. Army’s standards for physical fitness [2].
The soldiers underwent extensive evaluation of their medical and exposure history, physical examination, pulmonary-function testing, and high-resolution computed tomography (CT). A total of 49 soldiers underwent thoracoscopic lung biopsy after noninvasive evaluation did not provide an explanation for their symptoms. Data on cardiopulmonary-exercise and pulmonary-function testing were compared with data obtained from historical military control subjects.
Among the soldiers who were referred for evaluation, a history of inhalational exposure to a 2003 sulfur-mine fire in Iraq was common but not universal. Of the 49 soldiers who underwent lung biopsy, all biopsy samples were abnormal, with 38 soldiers having changes that were diagnostic of constrictive bronchiolitis. In the remaining 11 soldiers, diagnoses other than constrictive bronchiolitis that could explain the presenting dyspnea were established. All soldiers with constrictive bronchiolitis had normal results on chest radiography, but about one quarter were found to have mosaic air trapping or centrilobular nodules on chest CT. The results of pulmonary-function and cardiopulmonaryexercise testing were generally within normal population limits but were inferior to those of the military control subjects.
In 49 previously healthy soldiers with unexplained exertional dyspnea and diminished exercise tolerance after deployment, an analysis of biopsy samples showed diffuse constrictive bronchiolitis, which was possibly associated with inhalational exposure, in 38 soldiers (Figure 7).
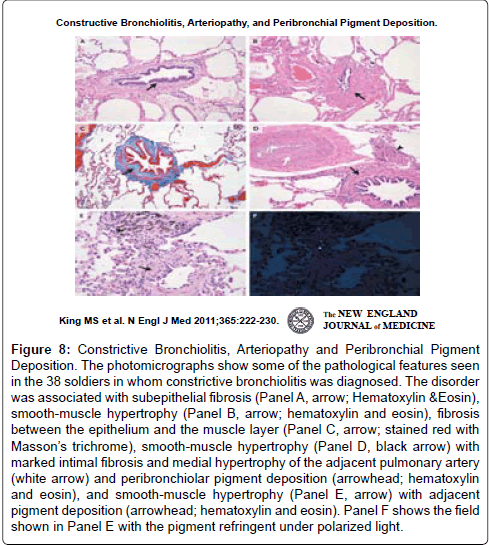
Figure 8: Constrictive Bronchiolitis, Arteriopathy and Peribronchial Pigment Deposition. The photomicrographs show some of the pathological features seen in the 38 soldiers in whom constrictive bronchiolitis was diagnosed. The disorder was associated with subepithelial fibrosis (Panel A, arrow; Hematoxylin &Eosin), smooth-muscle hypertrophy (Panel B, arrow; hematoxylin and eosin), fibrosis between the epithelium and the muscle layer (Panel C, arrow; stained red with Masson’s trichrome), smooth-muscle hypertrophy (Panel D, black arrow) with marked intimal fibrosis and medial hypertrophy of the adjacent pulmonary artery (white arrow) and peribronchiolar pigment deposition (arrowhead; hematoxylin and eosin), and smooth-muscle hypertrophy (Panel E, arrow) with adjacent pigment deposition (arrowhead; hematoxylin and eosin). Panel F shows the field shown in Panel E with the pigment refringent under polarized light.
Future Research Trends
The Denver Working Group on Post-Deployment Health paper in an upcoming issue of the JOEM, is regarding expert recommendation to promote surveillance pre- and post-deployment in regions of conflict, such as Iraq and Afghanistan. The recommendations take into account risks of new-onset asthma and bronchiolitis. With the December 2011 withdrawal from Iraq, U.S. forces are now heavily concentrated in Afghanistan, which has a different geological terrain and many small burn pits. We are studying mouse models of Iraq and Afghanistan War Lung Injury (IAW-LI) with dust from these respective locations, normalizing surface area to particle size, so that equivalent doses of dust from each respective country may be given to mice.
The objective of the Denver Working Group was to review inhalational exposures and respiratory disease risks in US military personnel deployed to Iraq and Afghanistan and to develop consensus recommendations for medical screening and diagnostic referral.
This Working Group comprised physicians and exposure scientists from academia and from the Departments of Defense and Veterans Affairs was convened in February 2010.
Despite uncertainty about the number of people affected and risk factors for adverse pulmonary outcomes in this occupational setting, the Working Group recommended: (1) standardized approaches to pre- and post-deployment medical surveillance; (2) criteria for medical referral and diagnosis; and (3) case definitions for major deploymentrelated lung diseases.
A key conclusion of the Denver Working Group is that there is a need for targeted, practical medical surveillance for lung diseases and for a standardized diagnostic approach for all symptomatic deployed personnel [15] (Tables 1-3).
| Standardized questionnaire eliciting |
| Smoking history |
| Pertinent medical history |
| Respiratory symptoms |
| Spirometry (before and after bronchodilator) |
| Exercise capacity evaluation (Physical Readiness Test) including I- or 2-mile run times |
Table 1: Recommended components of pre- and post deployment medical surveillance.
| Persistent (more than 3 months), unexplained cough, shortness of breath, or wheezing/chest tightness |
| Any abnormal spirometry pattern (below the lower limit of normal) |
| Excessive decline in forced expiratory volume in 1 s or forced vital capacity, defined as a 15% or more decrease in either parameter between pre- and post deployment testing, even if spirometry is within the normal range |
| A 10% or more decline comparing pre- and post deployment spirometry if new onset respiratory symptoms are also reported |
| Excessive decline in Physical Readiness Test compared with pre-deployment testing |
Table 2: Findings on post deployment medical testing that should prompt diagnostic referral.
| Comprehensive medical questionnaire, including full occupational exposure history |
| Physical examination, with particular attention to cardiopulmonary findings and body mass index |
| Full pulmonary function tests (lung volumes). DLCO, pre- and post bronchodilator spirometry |
| Methacholine challenge |
| High-resolution computed tomography-prone and supine, expiratory views |
| Maximum exercise tolerance testing with arterial blood gases and full metabolic exercise |
| Consider referral for surgical lung biopsy to assess constrictive bronchiolitis on a case-by-case basis |
| DLCO. diffusion capacity for carbon monoxide |
Table 3: Recommended approach to diagnostic testing for post deployment patients referred for further evaluation.
References
- Szema AM, Peters MC, Weissinger KM, Gagliano CA, Chen JJ (2010) New-onset asthma among soldiers serving in Iraq and Afghanistan. Allergy Asthma Proc 31: 67-71.
- King MS, Eisenberg R, Newman JH, Tolle JJ, Harrell FE Jr, et al. (2011) Constrictive bronchiolitis in soldiers returning from Iraq and Afghanistan. N Engl J Med 365: 222-230.
- Szema AM, Schmidt MP, Lanzirotti A, Harrington AD, Lyubsky S, et al. (2012) Titanium and iron in lung of a soldier with nonspecific interstitial pneumonitis and bronchiolitis after returning from Iraq. J Occup Environ Med 54: 1-2.
- Szema AM, Salihi W, Savary K, Chen JJ (2011) Respiratory symptoms necessitating spirometry among soldiers with Iraq/Afghanistan war lung injury. J Occup Environ Med 53: 961-965.
- Izbicki G, Chavko R, Banauch GI, Weiden MD, Berger KI, et al. (2007) World Trade Center "sarcoid-like" granulomatous pulmonary disease in New York City Fire Department rescue workers. Chest 131: 1414-1423.
- Smith B, Wong CA, Smith TC, Boyko EJ, Gackstetter GD; Margaret A. K., Ryan for the Millennium Cohort Study Team (2009) Newly reported respiratory symptoms and conditions among military personnel deployed to Iraq and Afghanistan: a prospective population-based study. Am J Epidemiol 170: 1433-1442.
- Alberdi Odriozola JC, Díaz Jiménez J, Montero Rubio JC, Mirón Pérez IJ, Pajares Ortiz MS, et al. (1998) Air pollution and mortality in Madrid, Spain: a time-series analysis. Int Arch Occup Environ Health 71: 543-549.
- Anderson HR, Atkinson RW, Bremner SA, Marston L (2003) Particulate air pollution and hospital admissions for cardiorespiratory diseases: are the elderly at greater risk? Eur Respir J Suppl 40: 39s-46s.
- Anderson JO, Thundiyil JG, Stolbach A (2012) Clearing the air: a review of the effects of particulate matter air pollution on human health. J Med Toxicol 8: 166-175.
- Ascherio A, Chase R, Coté T, Dehaes G, Hoskins E, et al. (1992) Effect of the Gulf War on infant and child mortality in Iraq. N Engl J Med 327: 931-936.
- Bai N, Khazaei M, van Eeden SF, Laher I (2007) The pharmacology of particulate matter air pollution-induced cardiovascular dysfunction. Pharmacol Ther 113: 16-29.
- Berglind N, Bellander T, Forastiere F, von Klot S, Aalto P, et al. (2009) Ambient air pollution and daily mortality among survivors of myocardial infarction. Epidemiology 20: 110-118.
- Brunekreef B, Holgate ST (2002) Air pollution and health. Lancet 360: 1233-1242.
- Buzea C, Pacheco II, Robbie K (2007) Nanomaterials and nanoparticles: sources and toxicity. Biointerphases 2: MR17-71.
- Rose C, Abraham J, Harkins D, Miller R, Morris M, et al. (2012) Overview and recommendations for medical screening and diagnostic evaluation for postdeployment lung disease in returning US warfighters. J Occup Environ Med 54: 746-751.
Relevant Topics
- Child Health Education
- Construction Safety
- Dental Health Education
- Holistic Health Education
- Industrial Hygiene
- Nursing Health Education
- Occupational and Environmental Medicine
- Occupational Dermatitis
- Occupational Disorders
- Occupational Exposures
- Occupational Medicine
- Occupational Physical Therapy
- Occupational Rehabilitation
- Occupational Standards
- Occupational Therapist Practice
- Occupational Therapy
- Occupational Therapy Devices & Market Analysis
- Occupational Toxicology
- Oral Health Education
- Paediatric Occupational Therapy
- Perinatal Mental Health
- Pleural Mesothelioma
- Recreation Therapy
- Sensory Integration Therapy
- Workplace Safety & Stress
- Workplace Safety Culture
Recommended Journals
Article Tools
Article Usage
- Total views: 17224
- [From(publication date):
April-2013 - Sep 03, 2025] - Breakdown by view type
- HTML page views : 12422
- PDF downloads : 4802