On the Link between Ellagic Acid and the Immune Balance between Human Mononuclear and Colon Carcinoma Cells
Received: 29-Oct-2017 / Accepted Date: 12-Nov-2017 / Published Date: 19-Nov-2017
Abstract
Pomegranate and particularly its phenolic compound ellagic acid (EA) have been well renowned as a therapeutic remedy for a long list of illnesses including inflammation and cancer. The beneficial activity of EA has been attributed to a number of factors comprising its immunomodulatory effect. Our aim was to examine the effect of EA on the immune relationship between human peripheral blood mononuclear cells (PBMC) and colon cancer cells from two human colon carcinoma cell lines.
Keywords: Mononuclear cells; Cancer cells; Interleukins; Cross-talk
Introduction
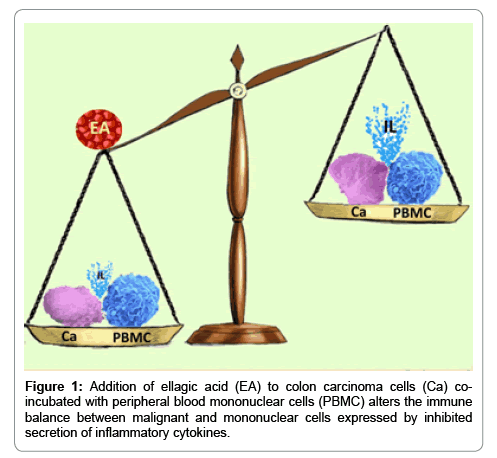
Ellagic acid (EA) is a polyphenol existing in one of the most ancient fruits, i.e., pomegranate, also known by its botanical name Punica granatum. The tree has been cultivated since centuries, it has been depicted in the mosaics of Pompeii [1], and even recommended by Avicenna for treatment of uterine bleeding [2]. Moreover, the fruit has been considered as sacred by foremost religions, for reasons thoroughly described by Langley [3]. The fruit’s juice has been highly appreciated following years of medical experience and research studies suggesting that its intake is linked with beneficial health properties such as antiinflammation, antioxidant and anti-proliferative activities [4,5]. In addition, a long list of therapeutic applications has been attributed to pomegranate and its juice, such as cardiovascular conditions, reduction of elevated blood pressure, diabetes and dental problems [5,6]. The antiinflammatory and anti-proliferative effect of EA warrants particular interest. A substantial number of studies have indicated that there is a close association between chronic inflammation and carcinogenesis (Figure 1). Development of colorectal cancer in patients suffering from ulcerative colitis or Crohn’s disease is an appropriate example for this coexistence [7]. Although genetic predisposition cannot be excluded, clinical observations such as extended and prolonged duration of inflammation, coexistence of additional inflammatory conditions and the ability of anti-inflammatory drugs to slow-down cancer development support the role of the inflammatory process in cancerogenesis [8-10]. In this sense the function of mononuclear cells and particularly the macrophages as leaders in the battle against cancer development should be acknowledged. To be effective in that task, these cells possess an array of armaments, such as inhibition of cell growth, interference with cell migration and prevention of metastases, as well as ability to produce anti-inflammatory cytokines. It should be noted that peripheral blood and tumor associated macrophages differ in their effect on carcinogenesis as it has been reviewed by Caux et al. [11] Evidently, with suppression of inflammation the possibility of cancer development should be limited. Moreover, in a previous study we have shown that HT-29 and RKO human colon carcinoma cells may activate cytokine production by mononuclear cells and to alter the immune balance between immune and cancer cells [12]. Taking into consideration the anti-proliferative ability of EA it was the aim of the present work to detect if this principal polyphenol constituent of pomegranate will affect the immune interchange between human peripheral blood mononuclear cells (PBMC) and cells from two human colon carcinoma cell lines i.e., HT-29 and RKO. The results may enlighten the way by which pomegranate exerts anti-cancer activity.
Materials and Methods
Cell preparation
Peripheral blood mononuclear cells (PBMC) were isolated from buffy coats obtained from venous blood of adult blood donors, using Lymphoprep-1077 (Axis-Shield PoC AS, Oslo, Norway) gradient centrifugation. The study was approved by the Ethics committee of Rabin Medical Center. Blood bank donors gave written informed consent in which they expressed their approval that certain blood components, not required for patients’ treatment, may be used for medical research. The cells were washed twice in phosphate buffered saline (PBS) and suspended in RPMI-1640 medium (Biological Industries, Beith Haemek, Israel) containing 1% penicillin, streptomycin and nystatin, 10% heat inactivated fetal bovine serum (FBS), and was designated as complete medium (CM).
Ellagic acid preparation
Ellagic acid (Sigma, Israel), was freshly dissolved in dimethyl sulfoxide (DMSO, Sigma, Israel) at a concentration of 2 mg/ml, and was further diluted in DMSO. EA was added to cultures at a final volume 10 μl/ml. DMSO was added to control cultures at 10 μl/ml.
Colon cancer cell lines
Two human colon cancer cell lines were used in the study - HT-29 and RKO obtained from American Type Cultural Collection, Rockville, MD. HT-29 cells were maintained in Mc-COY'S 5A medium and RKO cells in modified eagle medium (MEM- Biological Industries Co, Beth- Haemek, Israel) supplemented with 10% FBS, 2 mM L-glutamine and antibiotics (penicillin, streptomycin and nystatin-Biological Industries Co, Beth-Haemek, Israel). The cells were grown in T-75 culture flasks at 37°C in a humidified atmosphere containing 5% CO2.
Effect of EA on cell proliferation
The effect of EA on cell proliferation was determined using XTT cell proliferation assay kit (Biological Industries, Beith Haemek, Israel). Briefly, 0.1 ml aliquots of HT-29 or RKO cell suspension (2 × 105/ml of appropriate CM) or PBMC (1 × 106/ml of CM) were added to each one of flat bottom 96 well plates and incubated for 24 hrs with either DMSO (10 μl/ml) or EA at concentrations of 5 μg/ml, 10 μg/ml and 20 μg/ml. At the end of the incubation period, the cells were stained for proliferation according to the manufacturer’s instructions. The plates were incubated for 2-4 hrs at 37°C in a humidified atmosphere containing 5% CO2 and the absorbance was measured at 450 nm using ELISA reader.
Effect of EA on cytokine production
0.4 ml of PBMC (4 × 106/ml of CM) was incubated with 0.4 ml of CM without and with LPS (100 ng/ml) or PMA/ionomycin (1 μg/0.5 μg/ml respectively). In another set of experiments, 0.4 ml of PBMC (4 × 106/ml of CM) were incubated with 0.4 ml cells of one of the colon cancer lines (4 × 105/ml) suspended in appropriate CM. EA was added at the onset of cultures at concentrations as indicated above. Control cultures contained DMSO at 10 μl/ml. The cultures were maintained for 24 hrs at 37°C in a humidified atmosphere containing 5% CO2. At the end of the incubation period the cells were removed by centrifugation at 450 g for 10 min, the supernatants were collected and kept at -70°C until assayed for cytokine content.
Cytokine content in the supernatants
The concentration of TNFα, IL-1β, IL-6, IFNγ, IL-2, IL-10, and IL- 1ra in the supernatants was tested using ELISA kits specific for these cytokines (Biosource International, Camarillo, CA), as detailed in the guide-line provided by the manufacturer. The detection levels of these kits were: 15 pg/ml for IL-6 and 30 pg/ml for the remaining ones.
Statistics
A linear mixed model with repeated measures and assumption of compound symmetry (CS) was used to assess the effect of different concentrations of EA on spontaneous cytokine secretion by PBMC or that induced by mitogens or by colon cancer cells. SAS vs 9.4 were used for this analysis. Paired t-test was applied to compare between the level of cytokines produced with various concentrations of EA and that found in control cultures. Probability values of p<0.05 were considered as significant. The results are expressed as mean ± SEM.
Results
Effect of EA on cell viability
Incubation of PBMC for 24 hrs with 10 and 20 μg/ml of EA revealed reduced cell proliferation (F2,10=8.22, p=0.0077) being significantly lower at EA concentration of 20 μg/ml by 29% (p=0.015). 24 hrs of incubation of either HT-29 or RKO colon cancer cells with concentrations of EA between 5 μg/ml and 20 μg/ml had no effect on cell proliferation examined by XTT cell proliferation test (F3,24=2.09, p=0.128 and F3,24=2.3, p=0.108, respectively, Table 1).
| EA | PBMC | HT-29 | RKO | |||
|---|---|---|---|---|---|---|
| Absorbance at 450 nm | P* | Absorbance at 450 nm | P* | Absorbance at 450 nm | ||
| 0 | 1141±119 | 2190±172 | 1277±250 | |||
| 5 µg/ml | - | NS | 2215±84 | NS | 1202±204 | NS |
| 10 µg/ml | 1088±76 | NS | 2345±91 | NS | 1336±210 | NS |
| 20 µg/ml | 793±58 | 0.015 | 2138±164 | NS | 1214±219 | NS |
Note:PBMC, HT-29 or RKO cells were incubated without (0) or with EA at concentrations as indicated. After 24 hrs, cell proliferation was tested using XTT test as described in Materials and Methods section. The results are expressed as Mean ± SEM of 9 experiments. P* value represents statistically significant difference from cells incubated without EA. NS - not statistically significant
Table 1: Effect of EA on cell proliferation (XTT test).
Effect of EA on spontaneous secretion of cytokines
The spontaneous production of all cytokines tested in the current study was not modified by 24 hrs of incubation of PBMC with EA at concentrations as indicated (p>0.1, Tables 2 and 3).
| EA µg/ml |
TNFα, ng/ml (n=6) |
IL-1β, ng/ml (n=6) |
IL-6, ng/ml (n=6) |
IFNγ, ng/ml (n=6) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean±SEM | P* | Mean±SEM | P* | Mean±SEM | P* | Mean±SEM | P* | ||||||
| Spontaneous | |||||||||||||
| 0 | 0.21±0.04 | 1.91±0.58 | 5.32±1.61 | 0.62±0.03 | |||||||||
| 5 | 0.19±0.01 | NS | 1.29±0.28 | NS | 7.56±2.13 | NS | 0.61±0.03 | NS | |||||
| 10 | 0.21±0.01 | NS | 1.50±0.35 | NS | 9.90±2.22 | NS | 0.64±0.01 | NS | |||||
| 20 | 0.19±0.01 | NS | 1.67±0.22 | NS | 8.60±1.51 | NS | 0.60±0.02 | NS | |||||
| LPS-induced | PMA-induced | ||||||||||||
| 0 | 0.50±0.1 | 5.92±0.26 | 17.04±0.71 | 34.1±6.09 | |||||||||
| 5 | 0.49±0.09 | NS | 5.86±0.12 | NS | 16.73±0.41 | NS | 32.7±5.20 | NS | |||||
| 10 | 0.49±0.08 | NS | 5.51±0.20 | 0.063 | 16.10±0.31 | 0.070 | 26.9±3.90 | 0.054 | |||||
| 20 | 0.41±0.09 | NS | 4.36±0.50 | 0.013 | 14.46±0.66 | 0.045 | 27.8±5.02 | 0.012 | |||||
Note:PBMC were incubated for 24 hrs without (spontaneous) or with either LPS or PMA as described in materials and Methods, in the absence (0) or the presence of EA at concentrations as indicated. The level of cytokines in the supernatants was tested by ELISA. The results are expressed as Mean ± SEM of 6 experiments. P* value represents statistically significant difference from cells incubated without EA. NS - not statistically significant
Table 2: Effect of EA on pro-inflammatory cytokine production.
| EA µg/ml |
IL-10 ng/ml (n=6) |
IL-1ra ng/ml (n=6) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Spontaneous | LPS-induced | Spontaneous | LPS-induced | |||||||
| Mean±SEM | P* | Mean±SEM | P* | Mean±SEM | P* | Mean±SEM | P* | |||
| 0 | 0.66±0.03 | 0.81±0.16 | 0.79±0.14 | 1.91±0.20 | ||||||
| 5 | 0.69±0.03 | NS | 0.84±0.06 | NS | 0.75±0.08 | NS | 1.80±0.15 | NS | ||
| 10 | 0.81±0.06 | NS | 0.78±0.03 | NS | 0.85±0.07 | NS | 1.60±0.16 | NS | ||
| 20 | 0.66±0.03 | NS | 0.66±0.03 | 0.026 | 0.73±0.09 | NS | 1.47±0.15 | 0.017 | ||
Note:PBMC were incubated for 24 hrs without (spontaneous) or with LPS as described in Materials and Methods in the absence (0) or the presence of EA at concentrations as indicated. The level of cytokines in the supernatants was tested by ELISA. The results are expressed as Mean ± SEM of 6 experiments. P* value represents statistically significant difference from cells incubated without EA. NS - not statistically significant
Table 3: Effect of EA on anti-inflammatory cytokine production.
Effect of EA on cytokine production induced by LPS or PMA
LPS induced TNFα generation was not affected by 24 hrs of incubation with EA at concentrations as indicated (F3,15=1.84, p=0.183). LPS- stimulated IL-1β, IL-6, IL-10 and IL-1ra production and PMA promoted IFNγ secretion were dose dependently reduced following 24 hrs of incubation with EA at 5 μg/ml-20 μg/ml (F3,15=9.59, p<0.001, F3,15=4.71, p=0.016, F3,15=3.32, p=0.049, F3,15=5.3, p=0.011, respectively, and F3,15=6.58, p=0.0047 for IFNγ). The reduction of cytokine secretion by stimulated PBMC was statistically significant at EA concentration of 20μg/ml only and was lowered by 26% for IL-1β, 15% for IL-6, 18.5% for IL-10, 23% for IL-1ra and 18.5% for IFNγ. At lower concentrations of EA the degree of reduced cytokine secretion did not reach statistically significance (Tables 2 and 3).
Effect of EA on cytokine production induced by HT-29 and RKO cells
Pro-inflammatory cytokines: The secretion of TNFα, IL-1β and IL-6 by PBMC induced by cells of both colon cancer lines was significantly inhibited by 24 hrs of incubation with EA at concentrations between 5 and 20 μg/ml (F3,15=15.8, p<0.001, F3,15=64.53, p<0.001, and F3,15=44.49 p<0.001, respectively for HT-29 induced cytokine secretion and F3,15=6.68, p<0.001, F3,15=1816, p<0.001, F3,15=24.34, p<0.001, respectively for RKO-induced production). EA caused reduced IFNγ secretion induced by HT-29 cells only (F3, 15=4.46, p=0.02), whereas that induced by RKO cells was not affected (F3, 15=1.86, p=0.18). Reduced IL-1β and IL-6 secretion induced by cancer cells was observed at EA concentration as low as 5 μg/ml, and reached 50% inhibition and more at EA concentration of 20 μg/ml (Table 4).
EA µg/ml |
TNFα, ng/ml (n=6) |
IL-1β, ng/ml (n=6) |
IL-6, ng/ml (n=6) |
IFNγ, ng/ml (n=6) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean±SEM | P* | Mean±SEM | P* | Mean±SEM | P* | Mean±SEM | P* | |||||||
| HT-29-induced | ||||||||||||||
| 0 | 0.62±0.06 | 7.40±0.47 | 27.44±3.32 | 2.26±0.41 | ||||||||||
| 5 | 0.56±0.07 | NS | 6.05±0.51 | 0.002 | 24.79±3.36 | 0.02 | 2.00±0.32 | NS | ||||||
| 10 | 0.57±0.07 | NS | 5.75±0.49 | <0.001 | 23.61±3.31 | 0.013 | 1.82±0.23 | NS | ||||||
| 20 | 0.46±0.07 | <0.006 | 3.47±0.29 | <0.001 | 13.39±2.31 | <0.001 | 1.61±0.19 | 0.049 | ||||||
| RKO-induced | ||||||||||||||
| 0 | 0.58±0.09 | 5.54±0.70 | 29.94±3.16 | 3.69±1.04 | ||||||||||
| 5 | 0.67±0.05 | NS | 5.57±0.90 | NS | 26.09±3.02 | 0.004 | 2.99±0.40 | NS | ||||||
| 10 | 0.61±0.06 | NS | 4.12±0.44 | 0.018 | 23.40±3.32 | 0.03 | 3.41±0.43 | NS | ||||||
| 20 | 0.47±0.08 | 0.047 | 2.50±0.44 | 0.001 | 11.22±1.61 | <0.001 | 2.46±0.37 | NS | ||||||
Note:PBMC were incubated for 24 hrs with HT-29 or RKO colon cancer cells in the absence (0) or the presence of EA at concentrations as indicated. The level of cytokines in the supernatants was tested by ELISA. The results are expressed as Mean ± SEM of 6 experiments. P* value represents statistically significant difference from cells incubated without EA. NS - not statistically significant
Table 4: Effect of EA on pro-inflammatory cytokine production.
Anti-inflammatory cytokines: The generation of the antiinflammatory cytokines IL-1ra and IL-10 by PBMC induced by HT-29 or RKO cells was significantly inhibited following incubation with 5-20 μg/ml of EA (F3,15=14.3, p<0.001, F3,15=6.73, p=0.0043, respectively for HT-29 induced cytokine secretion and F3,15=14.85, p<0.001, F3,15=5.38, p=0.01, respectively for RKO- induced production). IL- 1ra production induced by both HT-29 and RKO cells was decreased by all three concentrations of EA used in the study, reaching 40% and 54% inhibition, respectively at 20 μg/ml of EA, whereas IL-10 secretion induced by HT-29 cells was only slightly reduced by EA (Table 5).
| IL-10 ng/ml (n=7) |
IL-1ra ng/ml (n=7) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| EA µg/ml |
HT-29- induced | RKO-induced | HT-29-induced | RKO-induced | ||||||
| Mean±SEM | P* | Mean±SEM | P* | Mean±SEM | P* | Mean±SEM | P* | |||
| 0 | 0.79±0.11 | 0.77±0.14 | 1.50±0.22 | 1.50±0.28 | ||||||
| 5 | 0.74±0.12 | 0.031 | 0.90±0.10 | NS | 1.35±0.22 | 0.05 | 1.34±0.19 | NS | ||
| 10 | 0.71±0.12 | 0.022 | 0.76±0.11 | NS | 1.20±0.16 | 0.011 | 1.16±0.16 | 0.045 | ||
| 20 | 0.71±0.11 | 0.018 | 0.75±0.12 | NS | 0.90±0.15 | 0.006 | 0.69±0.12 | 0.009 | ||
Note:PBMC were incubated for 24 hrs with HT-29 or RKO colon cancer cells in the absence (0) or the presence of EA at concentrations as indicated. The level of cytokines in the supernatants was tested by ELISA. The results are expressed as Mean ± SEM of 7 experiments. P* value represents statistically significant difference from cells incubated without EA. NS - not statistically significant
Table 5: Effect of EA on anti-inflammatory cytokine production.
Discussion
The beneficial effect of pomegranate juice in general and EA in particular on the immune system is well recognized. In a double blind study Shema-Didi et al. [13] have administered 100 ml. of pomegranate juice three times a week to 101 patients being on chronic dialysis and concluded that the patients showed reduced oxidative stress and lower incidents of inflammation morbidity. Other studies revealed that EA was able to promote expression of innate immune mediators justifying its use in immune-mediated diseases [14-16]. It has been reported that EA caused a significant inhibition on the production of the proinflammatory cytokines TNFα and IL-6 by murine RAW macrophages [17]. As for its effect on human PBMC, Anderson and Teuber [18] have found that EA decreased the secretion of IL-13 and TNFα, but not that of IL-2 and IL-4. In our hands, while unstimulated cells did not show any immune response following incubation with EA, it inhibited the generation of almost all cytokines examined except that of TNFα by LPS-stimulated PBMC. The results became quite different when PBMC were induced for cytokine production by both HT-29 and RKO colon carcinoma cells. In both cases the cells were intensely stimulated and inhibited the production of all cytokines examined in the present work. These findings support the results observed in previous studies in our laboratory in which we have repeatedly demonstrated the existence of an immune dialogue between PBMC and colon cancer cells from the two lines [12,19-21]. Application of EA as an additional therapy for malignant diseases has been forwarded both in vitro and in experimental models in vivo [22]. MCF-7 breast cancer cells treated with EA showed inhibited proliferation due to interference with the cell cycle [23,24]. Cell proliferation assays in the present study showed that EA does not affect cancer cells of the both lines. These results are rather unanticipated since they are in certain discordance with reports in the literature. Observations demonstrating the inhibitory effect of EA on cell proliferation have been reported with colon and prostate cancer cells [25-27]. Administration of EA to rats with dimethylhydrazine induced colon carcinoma resulted in marked inhibition of a number of inflammatory mediators including IL-6 and TNFα [28]. Umesalma et al. [29] have shown that EA was able to decrease proliferation of HCT-15 colon adenocarcinoma cells via inhibition of alkaline phosphatase and lactate dehydrogenase activities. Similar findings have been reported with HCT-116 and CaCo-2 colon cancer cells lines [30-32]. Inhibited cell proliferation by EA has been reported in several types of malignant cells such as human glioblastoma cells [33] and human pancreatic carcinoma cells [34]. Human adenocarcinoma epithelial cells (A549) treated with EA showed repressed IL-8 and TNFα production [35]. Apparently, the anti-proliferative effect of EA is expressed by a several mechanisms reviewed by Chen et al. [34] and Zhang et al. [36]. The discrepancy between these reports and our findings might be related to the type of cells, EA concentration and the methods applied to assess cell proliferation. Thus, while pomegranate juice was shown to inhibit HT-29 colon cancer cells proliferation, EA itself, similarly to our findings was futile [37].
The main outcome from the current study was the activity that various EA concentrations exerted on the cross-talk between immune and cancer cells. While lower EA concentrations decreased IL-1β, IL-6, IL-1ra and IL-10 production by PBMC incubated with HT-29 cells, higher concentration inhibited the production of all cytokines examined, except IFNγ. A concentration dependent inhibitory effect was observed also when EA was added to PBMC co-cultured with RKO cells. However, in that setting, higher doses of EA did not affect IFNγ and IL-10 production. It is reasonable to assume that inhibited secretion of pro-inflammatory cytokines will reduce the process of inflammation and will cause a deceleration in cancer progress [38]. It is notable that in the living organism tissue associated macrophages are tightly related to tumor growth and progress in addition to PBMC, as it has been reviewed by Bingle et al. [39].
Conclusion
The observations in the present work suggest that the altered immune cross-talk between PBMC and colon carcinoma cells, at least from the two lines examined, is indicative for the existence of an additional mechanism by which cells specialized in immune protection may abolish cancer progression.
Acknowledgement
The authors thank to Ms. Tzippy Shochat, MSc, Statistical Consultant, Rabin Medical Center, Beilinson Hospital, for her indispensable help in the statistical calculations.
References
- Melillo L (1994) Diuretic plants in the paintings of Pompeii. Am J Nephrol 14:423-425.
- Mobli M, Qaraaty M,Amin G, Haririan I, Hajimahmoodi M, et al. (2015) Scientific evaluation of medicinal plants used for the treatment of abnormal uterine bleeding by Avicenna. Arch Gynecol Obstet 292:21-35.
- Sreekumar S, Sithul H, Muraleedharan P, Azeez JM, Sreeharshan S (2014)Pomegranate fruit as a rich source of biologically active compounds. Biomed Res Int.
- Jurenka JS (2008) Therapeutic applications of pomegranate (Punicagranatum L.): A review. Altern Med Rev 13: 128-144.
- Sahebkar A, Ferri C, Giorgini P, Bo S, Nachtigal P, et al. (2017) Effects of pomegranate juice on blood pressure: A systematic review and meta-analysis of randomized controlled trials. Pharmacol Res 115: 149-161.
- Yang GY, Taboada S, Liao J (2009) Inflammatory bowel disease: A model of chronic inflammation-induced cancer. Methods Mol Biol 511: 193-233.
- Itzkowitz SH, Yio X (2004) Inflammation and cancer IV. Colorectal cancer in inflammatory bowel disease: the role of inflammation. Am J Physiol Gastrointest Liver Physiol 287: G7-17.
- Triantafillidis JK, Nasioulas G, Kosmidis PA (2009) Colorectal cancer and inflammatory bowel disease: epidemiology, risk factors, mechanisms of carcinogenesis and prevention strategies. Anticancer Res 29: 2727-2737.
- Kraus S, Arber N (2009) Inflammation and colorectal cancer. Curr Opin Pharmacol 9: 405-410.
- Caux C, Ramos RN, Prendergast GC,Bendriss-Vermare N,Ménétrier-Caux C (2016) A milestone review on how macrophages affect tumor growth. Cancer Res 76: 6439-6442.
- Bessler H, Djaldetti M (2010) Role of the equilibrium between colon cancer and mononuclear cells in cytokine production.Biomed Pharmacother 64: 706-711.
- Shema-Didi L, Sela S,Ore L,Shapiro G, Geron R, et al. (2012) One year of pomegranate juice intake decreases oxidative stress, inflammation, and incidence of infections in hemodialysis patients: a randomized placebo-controlled trial. Free Radic Biol Med 53: 297-304.
- Promsong A,Chung WO, Satthakarn S, Nittayananta W (2015) Ellagic acid modulates the expression of oral innate immune mediators: potential role in mucosal protection. J Oral Pathol Med 44: 214-221.
- Gracious RR, Selvasubramanian S, Jayasundar S (2001) Immunomodulatory activity of Punicagranatum in rabbits: A preliminary study.J Ethnopharmacol 78: 85-92.
- Allen CT,Peden-Adams MM,EuDaly J,Keil DE (2003) Subchronic exposure to ellagic acid impairs cytotoxic T-cell function and suppresses humoral immunity in mice. Immunopharmacol Immunotoxicol 25: 409-422.
- Seo CS, Jeong SJ, Yoo SR, Lee NR, Shin HK (2016) Quantitative analysis and in vitro anti-inflammatory effects of gallic acid, ellagic acid, and quercetin from radix sanguisorbae. Pharmacogen Mag 12: 104-108.
- Anderson KC, Teuber SS (2010) Ellagic acid and polyphenolics present in walnut kernels inhibit in vitro human peripheral blood mononuclear cell proliferation and alter cytokine production. Ann NY Acad Sci 1190: 86-96.
- Bessler H, Djaldetti M (2017) Capsaicin modulates the Immune cross talk between human mononuclears and cells from two colon carcinoma lines. Nutr Cancer 69: 14-20.
- Bessler H, Djaldetti M (2016) Vitamin B6modifies the immune cross-talk between mononuclear and colon carcinoma cells. Folia Biol (Praha) 62: 47-52.
- Djaldetti M, Bessler H (2017) Probiotic strains modulate cytokine production and the immune interplay between human peripheral blood mononuclear cells and colon cancer cells. FEMS Microbiol Lett 364: 1-5.
- Adhami VM, Khan N, Mukhtar H (2009) Cancer chemoprevention by pomegranate: Laboratory and clinical evidence. Nutr Cancer 61: 811-815.
- Chen HS, Bai MH, Zhang T, Li GD, Liu M (2015)Ellagic acid induces cell cycle arrest and apoptosis through TGF-β/Smad3 signaling pathway in human breast cancer MCF-7 cells. Int J Oncol 46: 1730-1738.
- Vini R, Sreeja S (2015) Punicagranatum and its therapeutic implications on breast carcinogenesis: A review. Biofactors 41: 78-89.
- Khan SA (2009) The role of pomegranate (Punicagranatum L.) in colon cancer. Pak J Pharm Sci 22: 346-354.
- Bell C, Hawthorne S (2008) Ellagic acid, pomegranate and prostate cancer: A mini review. J Pharm Pharmacol 60: 139-144.
- Eskandari E, Heidarian E, Amini SA,Saffari-Chaleshtori J (2016) Evaluating the effects of ellagic acid on pSTAT3, pAKT, and pERK1/2 signaling pathways in prostate cancer PC3 cells. J Cancer Res Ther 12: 1266-1271.
- Umesalma S, Sudhandiran G (2010) Differential inhibitory effects of the polyphenol ellagic acid on inflammatory mediators NF-kappaB, iNOS, COX-2, TNF-alpha, and IL-6 in 1,2-dimethylhydrazine-induced rat colon carcinogenesis. Basic Clin Pharmacol Toxicol 107: 650-655.
- Umesalma S, Nagendraprabhu P, Sudhandiran G (2015) Ellagic acid inhibits proliferation and induced apoptosis via the Akt signaling pathway in HCT-15 colon adenocarcinoma cells. Mol Cell Biochem 399: 303-313.
- Yousef AL,El-Masry OS, Yassin EH (2016)The anti-oncogenic influence of ellagic acid on colon cancer cells in leptin-enriched microenvironment. TumourBiol 37: 13345-13353.
- Zhao J,Li G, Bo W, Zhou Y,Dang S, et al. (2017) Multiple effects of ellagic acid on human colorectal carcinoma cells identified by gene expression profile analysis. Int J Oncol 50: 613-621.
- Seeram NP, Adams LS, Henning SM, Niu Y, Zhang Y, et al. (2005) In vitro antiproliferative, apoptotic and antioxidant activities of punicalagin, ellagic acid and a total pomegranate tannin extract are enhanced in combination with other polyphenols as found in pomegranate juice. J Nutr Biochem 16: 360-367.
- Wang D, Chen Q, Liu B, Li Y, Tan Y, et al. (2016) Ellagic acid inhibits proliferation and induces apoptosis in human glioblastoma cells. Acta Cir Bras 31: 143-149.
- Cheng H, Lu C, Tang R, Pan Y, Bao S, et al. (2017) Ellagic acid inhibits the proliferation of human pancreatic carcinoma PANC-1 cells in vitro and in vivo. Oncotarget 8: 12301-12310.
- Gauliard B, Grieve D, Wilson R, Crozier A, Jenkins C, et al. (2008) The effects of dietary phenolic compounds on cytokine and antioxidant production by A549 cells. J Med Food 11: 382-384.
- Zhang HM, Zhao L,Li H,Xu H, Chen WW, et al. (2014) Research progress on the anticarcinogenicactions and mechanisms of ellagic acid. Cancer Biol Med 11: 92-100.
- Adams LS, Seeram NP, Aggarwal BB, Takada Y, Sand D, et al. (2006) Pomegranate juice, total pomegranate ellagitannins, and punicalagin suppress inflammatory cell signaling in colon cancer cells. J Agric Food Chem 54: 980-985.
- Rocha A, Wang L, Penichet M,Martins-Green M (2012) Pomegranate juice and specific components inhibit cell and molecular processes critical for metastasis of breast cancer. Breast Cancer Res Treat 136: 647-658.
- Bingle L, Brown NJ, Le wis CE (2002) The role of tumour-associated macrophages in tumour progression: implications for new anticancer therapies. J Pathol 196: 254-265.
Citation: Bessler H, Djaldetti M (2017) On the Link Between Ellagic Acid and the Immune Balance Between Human Mononuclear and Colon Carcinoma Cells. Immunol Curr Res 1: 101.
Copyright: © 2017 Bessler H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 4281
- [From(publication date): 0-2017 - Jul 12, 2025]
- Breakdown by view type
- HTML page views: 3410
- PDF downloads: 871