Orthodontics and Oral Microflora: Synergism or Parasitism
Received: 03-Dec-2017 / Accepted Date: 31-May-2018 / Published Date: 06-Jun-2018
Abstract
Microorganisms cannot be seen through naked eye but we can feel their impact on us in various ways. Though only 3% of the total microbial populations are harmful to the humans without knowing, we are getting their help from the historic days eg. souring of milk, pickles, jams, dosa and idly making, wine production etc. In an average adult, there are 100 trillion human cells and 1500 trillion microbes. Thus, at best we are little more than 10% of us. Hence we are all just Petri dishes with shoes. We as orthodontists often intervene with the most important microbial habitat that is the oral cavity. Various studies have been done in relation to orthodontics and oral flora which have been unable to resolve the dilemma of the type of relationships among the two. The relationships formed and thereby the success of an orthodontic therapy depends upon both an orthodontist as well as the patient. All procedures beginning with appliance fabrication, insertion, oral hygiene maintenance and patient motivation are equally important. A balance and harmony have to be maintained from initiation throughout progression till the end of the therapy. If any of the above becomes wrong or imbalanced, orthodontic therapy fails.
Keywords: Oral ecosystem; Orthodontics; Microbes; Oral hygiene
Introduction
Microorganisms cannot be seen through naked eye but we can feel their impact on us in various ways. Though only 3% of the total microbial populations are harmful to the humans without knowing, we are getting their help from the historic days eg. souring of milk, pickles, jams, dosa and idly making, wine production etc.
Hence, we shall never underestimate a microorganism potential. In an average adult, there are 100 trillion human cells but 1500 trillion microbes. Hence, at best you are little more than 10% of you and can be rightly called Petri dishes with shoes [1]. Thus, this review article attempts to summarize the normal and abnormal flora of oral cavity, its interaction, and relation to orthodontics.
Oral ecosystem
An ecosystem is a community of living organisms (plants, animals, and microbes) in conjunction with the nonliving components of their environment (things like air, water, and mineral soil), interacting as a system linked together through nutrient cycles and energy flows.
They begin from autotrophs using solar energy for photosynthesis to the decomposers or scavengers cleaning the dead and the waste. Thus, it includes the microbial community in a specific habitat together with the abiotic surroundings [2].
The mouth as a microbial habitat
The microbes found in oral habitat are viruses, bacteria, yeasts, mycoplasma, and protozoans. Ecology of mouth is different from that in other parts of our body with the most important rule being that “Ecology changes as a child grows”.
Ecological conditions allow only particular organisms to survive while others perish. So, as ecology changes organisms also change. It acts as the culture medium for various organisms from unicellular to multicellular to survive [3].
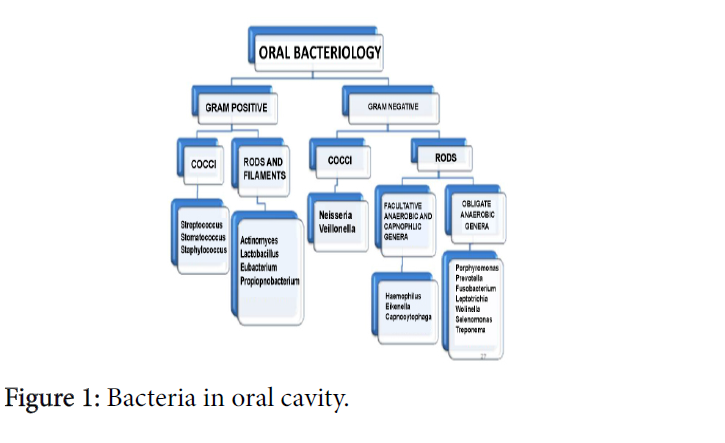
Bacteria in the oral cavity: These can be gram positive or gram negative [4] (Figure 1).
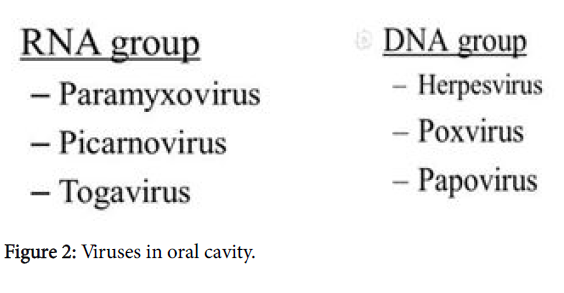
Viruses in oral cavity: These can be RNA or DNA possessing viruses [5] (Figure 2) Oral fungi.
Candida species is the most common. Though they are distributed throughout mouth but are found to be highest in the dorsum of tongue [5].
Oral mycoplasmas
Following are important mycoplasmas along with their specific locations in the oral cavity:
M. salivarium , pneumonia , and hominis exist in saliva, M. buccale , orale , and pneumonia exist in oral mucosa whereas, M. pneumoniae , buccale and orale commonly exist in plaque. On the other hand, M. salivarium is commonly isolated from gingival sulci and is suspected to play a role in periodontal diseases. While M. Orale has been associated with Sjogren syndrome [5].
Oral protozoans
Important oral protozoans are Entamoeba gingivalis and Trichomonas tenax [5].
Acquisition of the Resident Oral Microflora
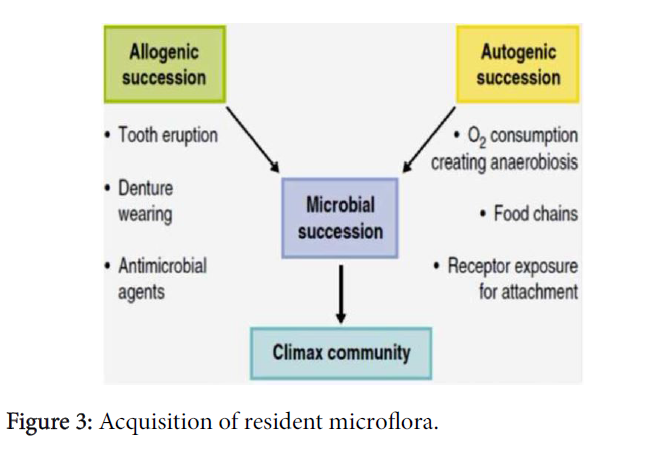
As oral cavity acts as an ecosystem thriving various life forms, it is important to understand how this ecosystem got established. It is explained as a combination of allogenic and autogenic succession as explained under [4] (Figure 3).
S. salivarius , S. mitis , and S. oralis are the pioneer species. In a newborn, S. salivarius is the most prevalent micro-organism, followed by coliforms , staphylococci , and enterococci in 1-5 days. Within hours oral cavity is colonized by low numbers of mainly facultative and aerobic bacteria. On the second day, anaerobic bacteria can be detected in the infant’s edentulous mouth. Anaerobe V. alcalescens is isolated from infants greater than 2 days old and regularly from infants after 1 week.
Anaerobic fusiform bacilli are seen in mouths younger than 2 months and from all infants before the eruption of incisors. The species colonizing the teeth after tooth eruption include Staphylococcus , Veillonella , Neisseria , Actinomyces , and Lactobacilli . Gingival crevice area also becomes habitat for a variety of anaerobic species. S. oralis , S. anginosus and S. gordonii are commonly reported to be present after the first year of life whereas, Bacteroides and spirochetes colonize around puberty.
To summarise, there are 1014 microorganisms consisting of more than 400 different types of bacteria in our oral cavity [6].
Microbial Colonies in Various Parts of Oral Cavity
Microflora of lips
Mostly occupied by facultative anaerobic streptococci especially S. mitis , S. oralis and S. constellatus [7]. Some obligate anaerobes like P. melaninogenica . Vellionela and Neisseria are also found in very low numbers. Candida albicans are also found to reside in damaged lip surfaces [8].
Microflora of buccal mucosa
Mostly Streptococci (30%) predominate though H. parainfluenzae is also common. Other species include Simonsiella , Granulicatella , Gemella , Vellionella , and Prevotella . Fish studies show periodontal problem causing species reside in buccal epithelial cells of healthy people wherein F. nucleatum carries S. cristatus via coaggregation [8].
Microflora of tongue
Dorsum of tongue supports maximum bacterial density with Streptococci (40%) being the most common especially salivarius and mitis group. Anaerobic Streptococci and Rothia mucilaginosa are also exclusively found on tongue [8].
Microflora of gingiva
It is resided by facultative and obligate anaerobes like Streptococcus , Actinomyces , Eubacterium , Fusobacterium , Prevotella and Treponema [8].
Microbial flora of tooth
The proximal surface of tooth harbors the following Gram positive and Gram negative obligate and facultative anaerobes: Neisseria , Streptococcus , Actinomyces , Prevotella , and Veillonella .
Pit and Fissure area of tooth harbors Gram-positive facultative anaerobes like Streptococcus and Actinomyces.
The Gingival crevice harbors the following Gram positive and Gram negative facultative and obligate anaerobes: Streptococcus, Actinomyces , Eubacterium , Fusobacterium , Prevotella and Treponema [9].
Types of Flora
Flora is of three types:
Resident flora
It represents those microorganisms that are demonstrated by culture, staining and immunologic techniques to be constantly found in given areas of the body for a given age. Resident flora depends on nutritional and physiological factors. It is absent in lungs and upper part of small intestine [4].
Intermediate/supplemental flora
Those bacterial species that are nearly always present, but in low numbers, that is, less than 1% of total viable count. These organisms may become indigenous if the environment changes. For e.g., Lactobacillus species are normally found in low levels in plaque [7].
Transient flora
Those microbial types that inhabit the host, particularly the skin and mucous membranes for short period of time-hours to days [7].
Microbial Relationships
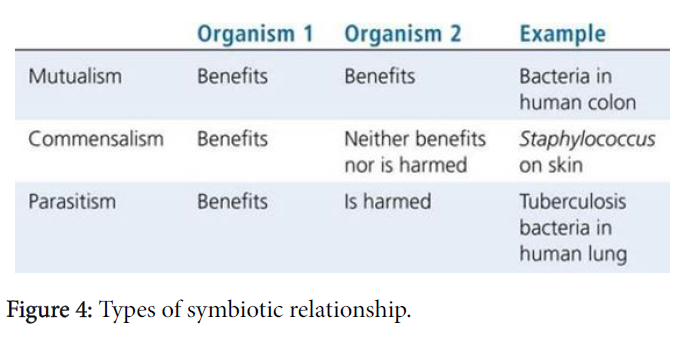
The oral cavity supports complex microbial communities. Common interactions are symbiosis, commensalism, antibiosis, and synergism [10]. There are three types of symbiotic relationships (Figure 4).
Defense Mechanisms In Oral Cavity
As oral cavity has to deal with significant amount of microbes, their communities and biofilms, it becomes essential to deal with them to prevent diseases and degradation of oral tissues. Although these communities tend to live harmoniously in oral environment but in case they become pathogenic or if our oral tissues are invaded by foreign microbes then it becomes essential to defend against this invasion [2,10].
• This protection is provided by:
• The Integrity of the oral mucosa
• Lymphoid tissue
• Saliva
• Gingival crevicular fluid
• Immune system
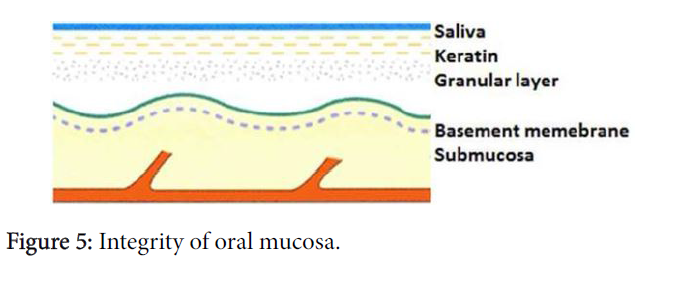
The integrity of the oral mucosa
Integrity of oral mucosa-epithelium and connective tissue acts as a single unit and prevents entry of microbes (Figure 5).
Lymphoid tissue
Lymphoid tissue is a collection of lymphocytic cells present in different locations which show appropriate immunological response against the invading microbes which includes the palatine and lingual tonsils consisting of B and T cells, salivary gland lymphoid tissue possessing secretory IgA, gingival lymphoid tissue displaying immunological response to plaque and the scattered submucosal lymphoid cells.
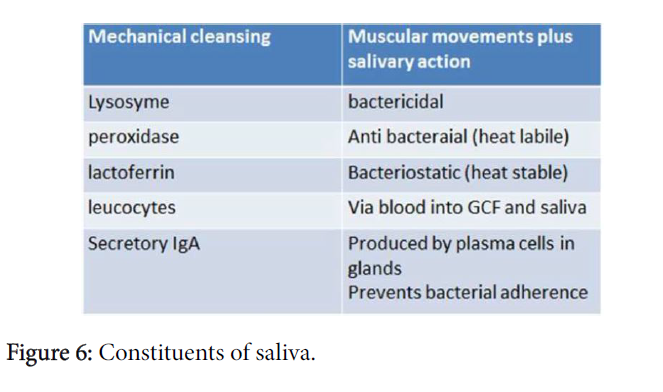
Saliva
Saliva bathes the oral cavity with each of its constituents displaying antibacterial and defense activity [2] (Figure 6).
Gingival crevicular fluid
GCF-gingival crevicular fluid provides protection by its constituents which include IgG, IgM, IgA, protein complement, enzymes, electrolytes, polymorphs, B lymphocytes, T lymphocytes and macrophages [10].
Immune system
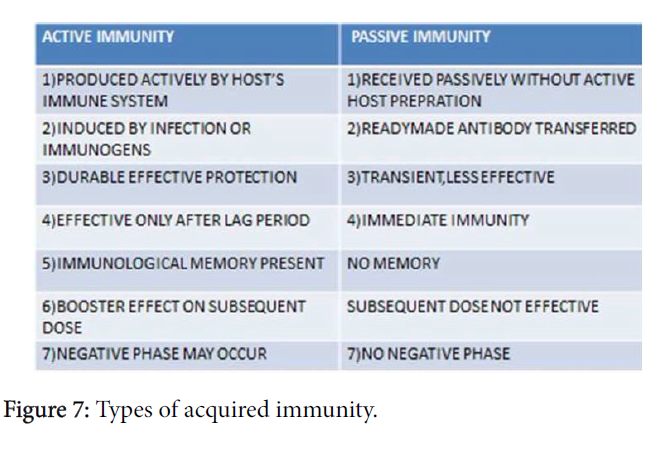
Traditionally term “immunity” refers to resistance exhibited by host towards injury caused by microorganisms and their products. It can be classified as:-
Innate immunity: It is resistance to infection by virtue of one’s own genetic and constitutional makeup. It may be specific to a particular organism or nonspecific working against various pathogens.
Acquired immunity: It is the resistance to infection acquired during the lifetime. It may be active or passive immunity (Figure 7).
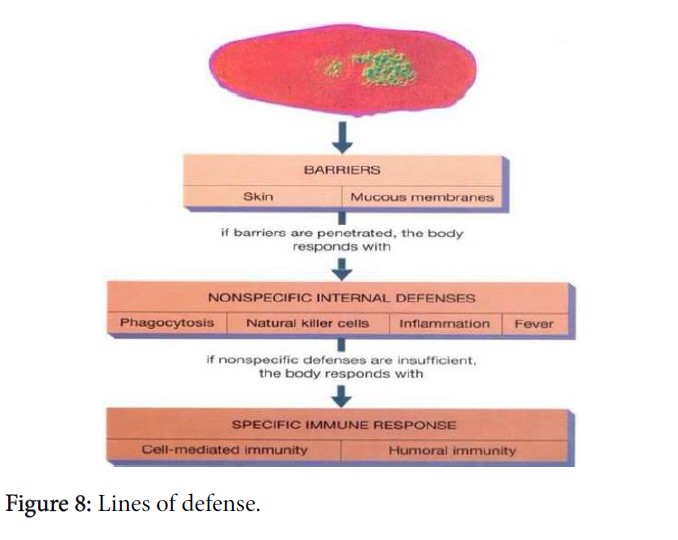
Thus, to summarize the human body is said to display three lines of defense against any invading pathogen that is the external barrier followed by the nonspecific internal defenses which if found to be insufficient are followed by a specific immune response (Figure 8).
Oral Microflora and Orthodontics
The relation of oral microflora and orthodontics has always been a controversial issue. While one side of the coin states malocclusion leads to gingivitis and other periodontal problems due to difficulty in oral hygiene maintenance, hence orthodontic treatment can subside it. In this support, Poulton showed positive effects on all perioral structures following orthodontic treatment and Lang showed improved periodontal conditions upon molar uprighting. While, Melson’s study showing intrusion of periodontally compromised teeth leading to the formation of new attachment gave rise to the other side of the story [11-13]. The other side says that orthodontic attachments during treatment make oral hygiene maintenance difficult hence leading to periodontal breakdown and intrusion, in particular, can lead to the conversion of supragingival plaque to subgingival hence, worsening the condition [14-16]. To conclude, a confluence of orthodontic treatment along with strict oral hygiene procedure is advocated to maintain the health of oral tissues.
Deleterious Effects of Orthodontic Treatment
Root resorption
Movement of a tooth over a long distance, application of an excessive amount of force or touching the alveolar cortices often leads to root resorption. Wherein, the root tip is found to be more prone to resorption than the lateral surface [17]. The following factors make a root more susceptible to resorption;
• Preexisting apical resorption
• Short, narrow roots
• Traumatic bite
• Trauma to anterior teeth
While few noted more resorption in endodontically treated teeth than vital ones [18], others reported no difference attributing tooth movement to be caused by inflammatory process occurring in the periodontium unaltered by the pulp chamber [19].
Gingival recession
Many studies reported dehiscence and recession during forward tooth movement [20,21]. Whereas, Wenstrom highlighted the role of thickness and volume of attached gingiva in the same [22]. Artun and Krogstad mentioned that recessions have tendency to progress during orthodontic treatment [23]. Wherein, Andlin and Sobock noted that recession in lower incisors region was more common during orthodontic treatment [24].
Abrasion and hard tissue effects
Though debonding brackets have always been associated with enamel loss. Many studies show that ceramic bracket removal causes marked enamel tear outs [25]. About 30 to 42 um enamel loss occurs through polishing, etching procedures and debonding of brackets, however, 72 um enamel loss occurs if bracket debonds repeatedly [26]. Thermal debonding or removal of silane component for ceramic brackets is better to reduce this effect. Zachrisson et al. found metal brackets to be better than ceramic brackets in this regard [27].
Plaque
According to Mizrahi banding procedure leads to plaque accumulation as loss of cement leads to its replacement by plaque beneath the bands [28]. According to Gwinnett and Ceen, plaque occupies space between composite cement and enamel [29]. Brackets, elastomeric ligatures, and other orthodontic attachments also make oral hygiene maintenance difficult and often attract plaque [30].
Demineralization
O’rielly and Featherstone mentioned about the loss of superficial enamel below the plaque formed under cemented bands [31]. According to Ceen and Gwinnett frequency of white spot, lesions is 50% in fixed appliance treatment. According to Gorelick and coworkers and Lundstrom and Krasse the main sites of demineralization are anterior maxilla and posterior mandible region. Geiger et al. highlighted a direct relation between duration of treatment and demineralization [32,33].
Bacterial proliferation
Sakamaki and Bahn noted that lactobacilli actively grow on fixed appliance followed by S. mutans. Corbett et al. found this growth to be more in banded cases than non-banded. Mattingl Y and Scheie et al. found that flora reduces during banding in both saliva and plaque but increases after 3 months and this increase in saliva is exponential with a number of bands and brackets. Kristofferson found that molars susceptibility to caries increases with bands and brackets on the proximal side. Schglenhauf found that fixed appliances retain more S. mutans than removable appliances.
Caries
Zachrisson and Zachrisson found a shift in the location of caries from proximal to buccal and lingual. Ingervall found the band around tooth acts as caries protector (if properly contoured). Corbett mentioned that caries problem arises only when a band is loose. Andermann found that caries occurs adjacent to bands particularly gingivally so bands should never be placed subgingivally [34].
Gingivitis and periodontal problems
Renglli et al., Zachrisson, Legott and Huser found that subgingival bands and crown cause gingival inflammation and attachment loss [35]. Ericsson found that subgingival margins displace plaque subgingivally and cause periodontal problems [36]. Diamanti et al. stated that P. gingivalis, P. intermidia, and Actinomyces predominate in these areas otherwise [37]. Muller and Flores de Jacoby found that spirochetes, mobile rods, and fusiform organisms increase with time whereas cocci decrease and that that active plates and functional appliance do not lead to a new periodontal problem. Atherton found the removal of these brackets bands with good hygiene corrects the problem. Freundorfer found banded tooth has more spirochetes than bonding cases. Miethke and Bernimoulin did a long-term study and found periodontal condition deteriorates after 1st year in banding cases more than in bonding cases [38]. However, Pender told that removable palatal plates lead to inflammation of the palatal gingiva, in case of poor hygiene [39].
Cleaning of Removable Appliances
• Cleaning with a toothbrush under running water.
• Cleaning in a water bath containing a cleanser tablet. According to Rabe et al. tablet cleansers lead to corrosion of silver solder connections [40]. They are effective only if used from 1st day because if plaque is formed once then it is inefficient in its complete removal.
• Ultrasonic bath: Diedrich says complete removal occurs by an ultrasonic bath (ULTRACLIN) though at a high cost.
• Chlorhexidine: It may be used as
a) SRD (slow release dosage): Releases continuously for 1 week (Friedman and Dyskind).
b) As varnishes (cervitec): According to Huizinga et al., Petersson et al. and Lynch and Beighton use of chlorhexidine as the varnish are better than oral rinse.
Ogaard found that plaque retention cervically or under a band leads to demineralization and even after 5 years, the condition of lesions may worsen especially in mandibular canines and premolars and maxillary laterals so to prevent this fluoride varnish at 3 months interval after orthodontic treatment is a better alternative.
Cleaning of Fixed Appliances
• According to Lundstrom and Hotz, there are 3 phases of prophylaxis [40]:
1) Preventive measures before treatment which include patient motivation, oral hygiene training, professional tooth cleaning and diet counseling.
2) Preventive measures during active treatment which includes control of oral hygiene, fluoride applications, diet counseling and chemical plaque control.
3) Preventive measures during retention which includes control of hygiene, fluoride applications, remineralization procedures and diet counseling.
• For any orthodontic case following requisites are needed:
a) Reduce periodontal risk
b) Reduce caries risk
c) Treatment of all carious lesions
d) Patient instruction and motivation
e) Efficient recall system
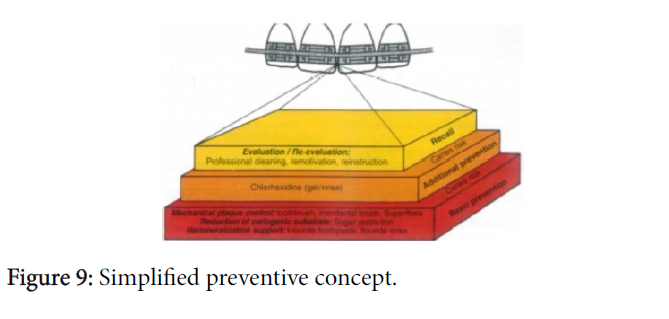
• Following simplified preventive concept is recommended (Figure 9).
1) Basic prevention:
a) Oral hygiene and fluoride toothpaste with dental floss
b) Oral prophylaxis
c) Flouride rinses
d) Flouride varnish on high risk surfaces
e) Diet counselling
2) Supplementary prevention
• As Chemical plaque control by chlorhexidine:
1) As a gel in custom trays
2) As varnish on high risk surfaces
3) Recall
a) Professional tooth cleaning
b) Remotivation and reconstruction
c) Evaluation of additional preventive measures
Principles of Optimal Orthodontic Treatment in Relation to Oral Hygiene
• For orthodontic attachments, bonding is preferred.
• Shortened bands so that margins present supragingivally.
• Prevent demineralisation by applying flouride varnish around bracket bases (3 months recall).
• Use GIC for banding.
• Loose bands and brackets should be recemented.
• Remove excess adhesive and cement remnants.
• Prevent labial tipping of lower incisors particularly if gingival propria is narrow and thin.
• For retainers with less interference, use a flouride releasing material.
• Intentional use of Hawthorne effect to improve oral hygiene compliance [41].
• Use of complementary aids like single tufted toothbrushes, chemical cleaning and horizontal scrub technique [42].
• Instituting oral hygiene programme prior to orthodontic treatment [43].
• Use of self-ligating brackets which promote less plaque adhesion [44].
Conclusion
Microbes are an important part of our oral cavity. The success of an orthodontic therapy depends upon both orthodontists as well as the patient. From fabrication to insertion of an appliance and from oral hygiene maintenance to patient motivation all are equally important. A balance and harmony have to be maintained during initiation, progression and at the end of the therapy. If any of the above becomes wrong or imbalanced, orthodontic therapy will fail.
However, we must conclude by turning the coin which also claims that orthodontic treatment during childhood or adolescence leads to moderate improvements in the emotional and social well-being dimensions of oral health-related quality of life, although the evidence is of low and moderate quality [45].
Acknowledgement
It is my pleasant privilege and honor to express my sincere and heartfelt gratitude to Dr. Manish Goyal and Dr. Akshita Sharma for their selfless support throughout.
References
- Ananthanarayan R (2013) Textbook of Microbiology. Hyderabad University Press.
- Greenberg MS, Glick M (2003) Jonathan A Burket's Oral Medicine. 11th edn. New York: BC Decker Inc.
- Siqueira J, Fouad A, Rôças I (2012) Pyrosequencing as a tool for better understanding of human microbiomes. J Oral Microbiol 4: 10743.
- Aas J, Paster B, Stokes L, Olsen I, Dewhirst F (2005) Defining the normal bacterial flora of the oral cavity. J Clin Microbiol 43: 5721-5732.
- Samaranayake L (2011) Essential microbiology for dentistry. 4th edn. Churchill Livingstone Elsevier, Edinburgh.
- Preza D, Olsen I, Willumsen T, Grinde B, Paster B (2009) Diversity and site-specificity of the oral microflora in the elderly. Eur J Clin Microbiol Infect Dis 28: 1033-1040.
- Marsh P, Lewis M, Rogers H, Williams D, Wilson M, et al. (2016) Marsh and Martin's oral microbiology. Elsevier, Churchill Livingstone.
- Horz H, Conrads G (2011) Methanogenic Archaea and oral infections-ways to unravel the black box. J Oral Microbiol 3: 5940.
- Diaz P, Chalmers N, Rickard A, Kong C, Milburn C, et al. (2006) Molecular characterization of subject-specific oral microflora during initial colonization of enamel. Appl Environ Microbiol 72: 2837-2848.
- Newman M, Takei H, Klokkevold P, Carranza F. Carranza's Clinical Periodontology. 12th edn. St. Louis. Elsevier Saunders; 2015.
- Jukka A (1972) Relationship between malalignment of the teeth and periodontal disease. Eur J Oral Sci 80: 104-110.
- Silness J, Røynstrand T (1985) Relationship between alignment conditions of teeth in anterior segments and dental health. J Clin Periodontol 12: 312-20.
- Ingervall B, Jacobsson U, Nyman S (1977) A clinical study of the relationship between crowding of teeth, plaque and gingival condition. J Clin Periodontol 4: 214-22.
- Buckley LA (1981) The relationships between malocclusion, gingival inflammation, plaque and calculus. J Periodontol 52: 35-40.
- Helm S, Petersen PE (1989) Causal relation between malocclusion and periodontal health. Acta Odontol Scand 47: 223-8.
- Lang NP, Hill RW (1977) Radiographs in periodontics. J Clin Periodontol 4: 16-28.
- Graber TM, Vanasdall RL (1994) Orthodontics: Current principles and techniques. St. Louis, Mosby: 41-42.
- Spurrier SW, Hall SH, Joondeph DR, Shapiro PA, Riedel RA (1990) A comparison of apical root resorption during orthodontic treatment in endodontically treated and vital teeth. Am J Orthod Dentofacial Orthop 97: 130-4.
- Ioannidou-Marathiotou I, Zafeiriadis AA, Papadopoulos MA (2013) Root resorption of endodontically treated teeth following orthodontic treatment: A meta-analysis. Clin Oral Investig 17: 1733-44.
- Thilander B, Nyman S, Karring T, Magnusson I (1983) Bone regeneration in alveolar bone dehiscences related to orthodontic tooth movements. Eur J Orthod 5: 105-14.
- Bernimoulin J, Curilovié Z (1977) Gingival recession and tooth mobility. J Clin Periodontol 4: 107-14.
- Wennström JL (1987) Lack of association between width of attached gingiva and development of soft tissue recession. A 5-year longitudinal study. J Clin Periodontol 14: 181-4.
- Artun J, Krogstad O (1987) Periodontal status of mandibular incisors following excessive proclination. A study in adults with surgically treated mandibular prognathism. Am J Orthod Dentofacial Orthop 91: 225-32.
- Andlin-Sobocki A, Marcusson A, Persson M (1991) 3-Year observations on gingival recession in mandibular incisors in children. J Clin Periodontol 18: 155-9.
- Pus MD, Way DC (1980) Enamel loss due to orthodontic bonding with filled and unfilled resins using various clean-up techniques. Am J Orthod 7: 269-83.
- Thompson RE, Way DC (1981) Enamel loss due to prophylaxis and multiple bonding/debonding of orthodontic attachments. Am J Orthod 79: 282-95.
- Zachrisson BU, Skogan O, Höymyhr S (1980) Enamel cracks in debonded, debanded, and orthodontically untreated teeth. Am J Orthod 77: 307-19.
- Mizrahi E (1982) Enamel demineralization following orthodontic treatment. Am J Orthod 82: 62-7.
- Gwinnett AJ, Ceen RF (1979) Plaque distribution on bonded brackets: A scanning microscope study. Am J Orthod 75: 667-77.
- Türkkahraman H, Sayin MO, Bozkurt FY, Yetkin Z, Kaya S, et al. (2005) Archwire ligation techniques, microbial colonization, and periodontal status in orthodontically treated patients. Angle Orthod 75: 231-6.
- O'Reilly MM, Featherstone JD (1987) Demineralization and remineralization around orthodontic appliances: An in vivo study. Am J Orthod Dentofacial Orthop 92: 33-40.
- Gorelick L, Geiger AM, Gwinnett AJ (1982) Incidence of white spot formation after bonding and banding. Am J Orthod 81: 93-8.
- Lundström F, Krasse B (1987) Streptococcus mutans and lactobacilli frequency in orthodontic patients: The effect of chlorhexidine treatments. Eur J Orthod 9: 109-16.
- Pradeep S (2014) Determination of microbiological flora of different hygienic ligatures techniques: An in vivo study. Int J Curr Microbiol App Sci 3: 739-746.
- Zachrisson S, Zachrisson BU (1972) Gingival condition associated with orthodontic treatment. Angle Orthod 42: 26-34.
- Ericsson I, Thilander B, Lindhe J, Okamoto H (1977) The effect of orthodontic tilting movements on the periodontal tissues of infected and non-infected dentitions in dogs. J Clin Periodontol 4: 278-93.
- Diamanti-Kipioti A, Gusberti FA, Lang NP (1987) Clinical and microbiological effects of fixed orthodontic appliances. J Clin Periodontol 14: 326-33.
- Miethke RR, Bernimoulin JP (1988) Effects of bands and brackets on the marginal periodontium. Fortschr Kieferorthop 49: 160-9.
- Pender N (1986) Aspects of oral health in orthodontic patients. Br J Orthod 13:95-103.
- Bourzgui F (2012) Orthodontics-Basic Aspects and Clinical Considerations. CC BY.
- Feil PH, Grauer JS, Gadbury-Amyot CC, Kula K, McCunniff MD (2002) Intentional use of the Hawthorne effect to improve oral hygiene compliance in orthodontic patients. J Dent Educ 66: 1129-1135.
- Zachrisson BU (1974) Oral hygiene for orthodontic patients: Current concepts and practical advice. Am J Orthod 66: 487-97.
- Yeung SCH, Howell S, Fahey P (1989) Oral hygiene program for orthodontic patients. Am J Orthod Dentofac Orthop 96: 208-13.
- Pellegrini P, Sauerwein R, Finlayson T, McLeod J, Covell Jr DA, et al. (2009) Plaque retention by self-ligating vs elastomeric orthodontic brackets: Quantitative comparison of oral bacteria and detection with adenosine triphosphate-driven bioluminescence. Am J Orthod Dentofac Orthop 135: 426.
- Hanieh J, Mario V, Philip EB (2017) Does orthodontic treatment before the age of 18 years improve oral health-related quality of life? A systematic review and meta-analysis. Am J Orthod Dentofac Orthop 151: 644-55.
Citation: Chawla R, Shetty KS, Prakash AT, Rathore APS, Saroch S (2018) Orthodontics and Oral Microflora: Synergism or Parasitism. J Interdiscipl Med Dent Sci 6: 234.
Copyright: © 2018 Chawla R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 5183
- [From(publication date): 0-2018 - Dec 10, 2025]
- Breakdown by view type
- HTML page views: 4228
- PDF downloads: 955