Paediatric Feeding Disorder
Received: 02-Aug-2022 / Manuscript No. nnp-22-69981 / Editor assigned: 04-Aug-2022 / PreQC No. nnp-22-69981 / Reviewed: 18-Aug-2022 / QC No. nnp-22-69981 / Revised: 22-Aug-2022 / Manuscript No. nnp-22-69981 / Published Date: 29-Aug-2022 DOI: 10.4172/2572-4983.1000253
Abstract
Pediatric feeding disorders (also termed avoidant/restrictive food intake disorders) are conditions in which a child avoids eating or limits what or how much he or she will eat. This leads to problems including weight loss, nutritional deficiency, need for nutritional supplements, or problems with daily functioning. These disorders often limit a child’s ability to participate in normal social activities such as eating with others, and disrupt family functioning.
Introduction
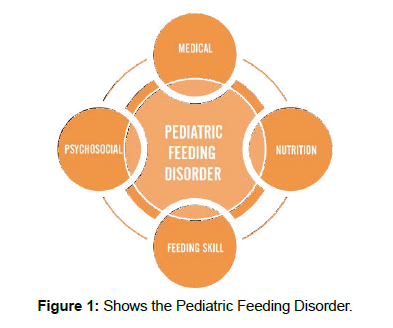
Feeding is a complex process that requires interaction of the central and peripheral nervous systems, oropharyngeal mechanism, cardiopulmonary system, and gastrointestinal (GI) tract with support from craniofacial structures and the musculoskeletal system. This coordinated interaction requires acquisition and mastery of skills appropriate for a child’s physiology and developmental stage. In children, feeding occurs in the context of the caregiver-child dyad [1]. A disruption in any of these systems places a child at risk for a feeding disorder and associated complications . Often, more than 1 system is disrupted, contributing to the development and persistence of pediatric feeding disorders (PFDs) [2] . Hence, effective assessment and treatment of PFDs require the involvement of multiple disciplines. The lack of a universally accepted definition has, however, hindered collaborative care [3]. (Figure 1)
Medical factors
Nutritional factors
Feeding skill factors
Psychosocial factors
Psychosocial Dysfunction
Causes
For most children, there is not just one thing that causes a feeding disorder. Most often, it is a combination of factors [4].
Things that can contribute to the development of a feeding disorder include:
Child temperament (slow to adapt, easily over-stimulated)
Pain or discomfort with feeding (from things like reflux and allergy)
Negative experiences with feeding (pain, coughing, vomiting or gagging during feeding)
Negative experiences related to the mouth (history of NG tubes, oral procedures, being on a ventilator, surgeries)
Slow emptying of the stomach
Poor oral motor skills (dysphagia)
Low muscle tone or high muscle tone
Developmental delays
Certain developmental disabilities, such as autism spectrum disorder [5].
Anxiety
ADHD
Sensory differences (hypersensitivity to taste, smell, texture)
Chronic health problems (ear infections, frequent respiratory infections, dental problems, seizures)
Parent-child conflict, parental anxiety
Diagnosis
Depending on the child’s history and current problems, the evaluation may include some or all of the following:
Review of medical history, growth pattern, developmental history, and current symptoms
Assessment of dietary intake by a registered dietician [6].
Evaluation by a physician or nurse practitioner with expertise in feeding and feeding disorders
Evaluation of feeding behaviors by a clinical psychologist [7].
Evaluation of oral motor skills, chewing and swallowing by a speech-language pathologist
Special tests to evaluate swallowing, such as a barium swallow or endoscopic assessment [8-9]
Evaluation by a pediatric gastroenterologist to determine if problems of the GI tract (GE reflux, constipation, delayed emptying, or other GI disorders) are contributing to feeding problems[10]
Evaluation of motor skills, posture, and sensory issues by a pediatric OT or PT
Blood work to evaluate nutrition status or to screen for medical conditions that can contribute to feeding problems.
Vaccination is disease-specific
Immune responses are very specific, and that is the reason we need to have a specific vaccine for each The immune system responds separately to each pathogen it encounters . It cannot be ‘overloaded’ by giving the full range of currently available vaccines or by having multiple antigens in one vaccine. A healthy immune system can generate hundreds of millions of T and B cells, each of which targets one particular antigen. However, pathogens can sometimes overwhelm the immune response. Vaccines give the immune system a head start by allowing it to learn and remember what a pathogen looks like, providing valuable protection against aggressive pathogens.
Pre-formed antibodies provide immediate protection
It takes around 7–21 days after being vaccinated to generate an effective immune response in healthy individuals. Most vaccines work by switching on a person’s immune system to make the antibodies, cytokines and memory cells needed to protect against infection. However, this kind of active immune response takes 7–21 days to fully develop. Sometimes, in the case of overwhelming and dangerous infections, an unwell person may receive pre-formed antibodies as part of their medical treatment to prevent or combat the infection. These either come from healthy blood donors or are produced in a laboratory, as they can act much more quickly to help the person fight off the infection This is known as ‘passive immunisation’. However, these antibodies don’t stay in the body for very long—it is better to make antibodies through being vaccinated wherever possible.
Conclusion
These proposed diagnostic criteria for PFD use a conceptual framework that goes beyond disease-oriented or unilateral diagnostic paradigms, defining PFD as restricted oral intake that is not age appropriate and leads to dysfunction in at least one of 4 closely related, complementary domains. Adoption of this definition by healthcare professionals from all disciplines will establish a common terminology that could have widespread impact on clinical practice, education, research, and advocacy.
Acknowledgement
None
Conflicts of interest
The author declares they have no competing conflicts of interest.
Funding
The study has no funding source.
References
- Bratteby LE,Garby L, Groth T, Schneider W, Wadman B (1968) Studies on erythro-kinetics in infancy XIII The mean life-span and the life-span frequency function of red blood cells formed during foetal life. Act Paediat Scand 57-311.
- OskiFA, Naiman JL (1966) Hematologic problems of the newborn. W B Saunders CompanyBaltimore 19-66.
- Smith CA (1959) The physiology of the newborn infant. 3Charles C Thomas PublisherPhiladelphia.
- Guest GM, Brown EW (1957) Erythrocytes and hemoglobin of the blood in infancy and childhood III Factors in variability statistical studies. Mer J Dis Child93-486.
- Gairdner D, Marks J, Roscoe (1952) Blood formation in infancy Part I The normal bone marrow. Arch Dis Child 27-128.
- Sturgeon P (1950) Volumetric and microscopic pattern of bone marrow in normal infants and children. Pediatr 7-577.
- Sturgeon P (1951) Volumetric and microscopic pattern of bone marrow in normal infants and children. Pediatr 7-642.
- Sturgeon P (1951)Volumetric and microscopic pattern of bone marrow in normal infants and children. Pediatr 7-774.
- Glaser K, Limarzi L, Poncher HG (1950) Cellular composition of the bone marrow in normal infants and children. Pediatr 6-789.
- Garby L, Sjolin S, Vuille J (1963) Studies on erythro-kinetics in infancy III Disappearance from plasma and red cell uptake of radioactive iron injected intravenously Acta Paediat Scand 52-537
Indexed at, Crossref, Google Scholar
Indexed at, Google Scholar, Cross ref
Indexed at, Crossref, Google Scholar
Citation: Jose R (2022) Paediatric Feeding Disorder. Neonat Pediatr Med 8: 253. DOI: 10.4172/2572-4983.1000253
Copyright: © 2022 Jose R. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 1719
- [From(publication date): 0-2022 - Dec 23, 2025]
- Breakdown by view type
- HTML page views: 1281
- PDF downloads: 438