Partograph Utilization and Associated Factors among Obstetric Caregivers in Public Health Facilities of Hawassa City Administration, Sidama State, Ethiopia, 2021
Received: 14-Jun-2022 / Manuscript No. jpch-22-66647 / Editor assigned: 15-Jun-2022 / PreQC No. jpch-22-66647(PQ) / Reviewed: 28-Jun-2022 / QC No. jpch-22- 66647 / Revised: 01-Jul-2022 / Manuscript No. jpch-22-66647(R) / Accepted Date: 08-Jul-2022 / Published Date: 08-Jul-2022 DOI: 10.4172/2376-127X.1000540
Abstract
Background: Globally, prolonged and obstructed labour contributed to 13% of maternal deaths which can be reduced by proper utilization of partograph during labour. Professional assisted delivery using a partograph during labour has paramount important in identifying any deviation during labor. Even though; partograph use is influenced by different factors it is not well identified in the study area. Thus the study aimed to assess partograph utilization and associated factors among obstetric caregivers in public health facilities of Hawassa City Administration, Sidama State, Ethiopia, 2021.
Methods: A facility based cross-sectional study was conducted from June 10 to June 30, 2021 among 221 study subjects sampled by simple random sampling technique in selected health facilities. Data was collected using structured self-administered questionnaire. The data was coded, cleaned, entered using Epi data version 3.1 and analyzed using SPSS version 23 statistical software. A descriptive statistics for categorical and continuous variables was done and summarized as numbers, percentages, means and standard deviation. Bi-variable and multi variable logistic regressions were performed to identify factors associated with partograph utilization. The strength of statistical association was measured by Adjusted Odds Ratios (AOR) and 95% confidence intervals. In all cases P-value, less than 0.05 were considered as statistically significant.
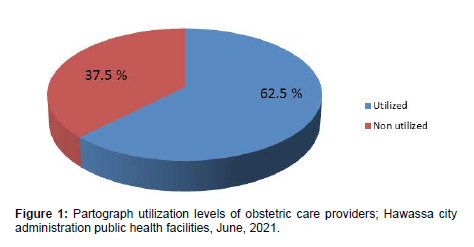
Result: From the total study participants 62.5% (95%CI: 56%, 69%) of them utilized partograph to monitor women’s in labor. Respondents educational status (AOR=0.038, 95%CI: 0.003, 0.506), profession (AOR=9.9, 95%CI: 1.06, 92.65), service training (AOR 2.28, 95% CI: 1.1, 4.7) and attitude towards partograph utilization (AOR = 3.7, 95% CI: 1.76, 7.83) were factors significantly associated with partograph utilization.
Conclusion: In this study partograph utilization level is about 62.5%. Educational status, profession, service training and attitude were significant factors associated with partograph utilization. The concerned bodies should strengthen supportive supervision and provide training to obstetric care providers in order to promote partograph utilization.
Keywords
Partograph Utilization; Obstetric Care Providers; Public Health Facilities; Ethiopia
Introduction
A partograph is graphic record of the progress of labour and relevant details of the mothers and fetus. Most of the labour related causes of maternal mortality and morbidity can be easily detected if the progress of labour is monitored using partograph. The use of partograph to manage labour improves maternal and newborn survival and reduces the need for additional interventions such as cesarean section. It also gives information about fetal and maternal condition that are all recorded on single sheet of paper [1].
The partograph consists of a graphic representation of labor and is an excellent visual resource to analyze uterine contraction, station, the effacement of the cervix, cervical dilatation, vital sign, fetal heart beat and fetal presentation in relation to time. However, poor utilization of the partograph was found in the public health institutions which reflect poor monitoring of mothers in labor and/or poor pregnancy outcome.
According to World Health Organization (WHO) reports globally, there were an estimated number of 303,000 maternal deaths in 2015. This means, that every day, nearly 830 women died from avoidable causes while during pregnancy and giving child birth. About 99% of maternal deaths occur in developing countries while around more than half of these occur in sub- Saharan Africa, most could have been preventable.
According to EDHS (Ethiopian Demographic and Health Survey) 2016 the ratio of maternal mortality in Ethiopia is 412/100,000 live births.
In Ethiopia Obstructed labour/uterine rupture, hemorrhage, hypertensive disorder of pregnancy and sepsis/infection, where the four major causes of maternal mortality. Early detecting the causes and timely intervene of all obstetric complications and problems are the most important activities to prevent maternal death and perinatal mortality and morbidity.
A systematically detecting and handling complication at early stage is part of guaranteeing quality service. Among these, partograph is one of the most and cost-effective methods to prevent unnecessary delay and serve as frontrunner for obstetric caregivers.
The women who experience prolonged labor and obstructed labour are usually suffer from anemia, endometritis, hemorrhage which is postpartum, eminent and total uterine rupture, puerperal sepsis and obstetric fistula. Furthermore, it is highly related with trauma at birth, early neonatal sepsis, birth asphyxia, in and out stillbirths, and neonatal deaths early and late. Due to poor partograph utilization there could be absence of early detection of complication and improper monitoring of the progress of labour.
Proper use of partograph during delivery is to achieve whole a healthy of the mother and wellbeing of the baby with the least possible level of early intervention, early detection, manage the causes accordingly and timely referral. Therefore, strategies have to be invented to decrease maternal mortality by giving more attention to the most death causing risk factors, in the area of these strategies the use of partograph is important tool for obstetric care givers who need to be able to identify problems and complications during childbirth in early manner and refer women to higher facility for better management and treatment. Besides, partograph is the best vital tool but it is not widely used as it should be [2].
Studies done across whole African countries has been shown that the utilization of partograph is inadequate despite preparing the best tool that is easy and inexpensive for intra partum monitoring of labour. Similarly, so many different studies in Ethiopia revealed poor utilization of partograph.
Studies conducted in Addis Ababa city and Amhara region, Ethiopia identified that shortage of preprinted partograph in the public health facilities, being a general practitioner, poor knowledge and attitude towards partograph were reason for not using partograph during labor.
Even though in-service training on comprehensive emergency obstetric and neonatal care which widely include partograph utilization given by different Non-Governmental Organizations at all level, some is known about how many of them utilize it within the city health facilities. Hence, this study gives more information on the level of partograph utilization and associated factors among obstetric care providers in public health facilities of Hawassa City Administration, Sidama State, Ethiopia, 2021.
Methods and Materials
Study design, period and setting
A facility-based cross-sectional study was conducted from June 10 to June 30, 2021s in Hawassa city, Sidama State, Ethiopia. Hawassa city is capital city of Sidama state. The city is located 273 kilometers south to Addis Ababa (capital city of Ethiopia). Within the city there are a total of 2787 health providers in the governmental health facilities, of which 440 are providing obstetric care.
Population
All health professions who are working in Obstetric care unit in public health facilities of Hawassa city administration were the source population whereas all health professions who are working in Obstetric care unit of randomly selected health facilities were the study population.
Sample size determination
The sample size was calculated using single population proportion formula (n= (Z α⁄2)2 p (1-p)/d2) by considering the following assumption: 95% level of confidence=1.96, proportion (p) of 40.2% partograph utilization among health care providers in North Shoa, Ethiopia, margin of error (5%) and non-respondent rate of 10%. Accordingly, the estimated final sample size for this study
Since, the numbers of obstetric care providers assigned in Obstetric care unit of all health facilities are very small (finite), we used population reduction formula considering the total number of obstetric care providers (440) in Hawassa city public health facilities to estimate the final sample size [3].
nf=n/1+n/N
nf = final sample size
N=total number of obstetric care providers=440
nf=369.4
(1+ (369.4/440)) nf =201
Taking non-response rate, the total sample size for this study was=221
Sampling procedure
In Hawassa city there are 10 health centers, 1 primary, 1 general and 1 comprehensive specialized hospital. The calculated sample size was proportionally allocated to the randomly selected public health centers and hospitals based on the number of obstetric care providers in each facility. Finally obstetric care providers in the selected public health facilities were selected randomly as study participants until the desired sample size was attained.
Data collection procedures and data quality assurance
A structured self-administered questionnaire developed by reviewing different related literatures with modification according to the objective of this specific study was used to gather important information from each study respondent.
The structured questionnaire were pretested on 5% of the total sample size in nearby health center. Data collectors and principal investigator was participated during the pretest. Then the questionnaire was assessed for its clarity, logical flow, length and completeness and the necessary correction was made before the actual data collection. We used 3 degree holder nurses for facilitating the data collection process after giving two days training regarding the objective of the study, relevance of the study and informed consent [4].
Operational definition
Obstetric care providers: This category includes medical doctor, midwifery, nurse and health officers which have given delivery service by regular time, rotation and duty time.
Partograph utilization: This was measured based on the number of Obstetric care providers who have been using partograph during monitoring labor.
Knowledge level: In order to determine knowledge level of the respondents, using structured self-administered questionnaire scores were computed for knowledge assessing questions. One point was allocated to a correct response which is appropriate for partograph utilization & 0 for incorrect response. For each knowledge assessing question correct answers were summed together and the mean score was computed for the total respondent’s response which was 4. Those who scored above (>) the mean score (4) were taken as good knowledge level where as those who were scored below (<) the mean score were taken as poor knowledge level.
Attitude: Obstetric care provider’s attitude towards partograph utilization was assessed using different Likert scales for different questions. It was measured by total score dichotomized into favorable and an unfavorable attitude taking the mean score as a (Mean score or more (≥ 6 = favorable attitude and less than the mean score unfavorable attitude).
Data Management and Analysis
The data were checked, cleaned and entered using Epi-data version 3.1 and exported to Statistical Package for Social Sciences (SPSS) version 23 for analysis. The descriptive analysis such as frequency distribution, percentages, mean and Standard Deviation (SD) were used.
Both bi variable and multi variable logistic regression models were fitted to identify factors associated with partograph utilization. To identify factors associated with the outcome variable, a bi- variable logistic regression analysis was performed for each independent variable and Crude Odds Ratio (COR) with 95% confidence intervals was obtained. Those variables that have p-value less than 0.25 on bivariable analysis were considered for multi-variable analysis. The presence and strength of statistical association was measured by Adjusted Odds Ratios (AOR) and 95% confidence intervals. In all cases P-value, less than 0.05 was considered as statistically significant. Finally the results were presented using tables, graphs and charts.
Results
Socio demographic and work related characteristics of the respondents A total of 216 obstetric care providers were included in the study with a response rate of 97.7%. The minimum and the maximum age of the respondents were 21 years and 49 years respectively. The mean (+ SD) age of the study subjects was 28.9 years (± 4.9). About 135 (62.5) % of the respondents were found in the age group 20 to 29 years. Around 165 (76.4%) of the study participants were females [5].
Majority of the respondents 139 (64.4%) were Protestant by religion followed by Orthodox 64 (29.6%). Concerning marital status about 107 (49.5%) of the study participants were single.
Around 162 (75%) of the study participants were degree holder. Regarding profession more than half 123(56.9%) of the respondents were B.sc Midwives. More than seven in ten 168 (77.8%) were currently working in Hospital. As far as service year is concerned greater than half 112 (51.9%) of the study participants have six year and above service provision experience.
More than seven in ten 154 (71.3%) of obstetric care providers were working in labor ward with 81 (37.5%) professional number per shift of 6 or more.
Regarding obstetric training about 128 (59.3%) of the participants had taken basic obstetric trainings of which around 82 (38%) had taken BEmONC (Table 1).
| Variables Frequency Percent | |||
|---|---|---|---|
| Age in years (n=216) | |||
| 20-29 | 135 | 62.5 | |
| 30-39 | 71 | 32.9 | |
| 40-49 | 10 | 4.6 | |
| Sex (n=216) | |||
| Female | 165 | 76.4 | |
| Male | 51 | 23.6 | |
| Religion (n=216) | |||
| Protestant | 139 | 64.4 | |
| Orthodox | 64 | 29.6 | |
| Muslim | 7 | 3.2 | |
| Catholic | 6 | 2.8 | |
| Marital status (n=216) | |||
| Single | 107 | 49.5 | |
| Married | 99 | 45.8 | |
| Divorced | 10 | 4.6 | |
| Educational status (n=216) | |||
| Diploma | 43 | 19.9 | |
| Degree | 162 | 75 | |
| MSc and above | 11 | 5.1 | |
| Profession (n=216) | |||
| Gynaecologist/Obstetrician | 7 | 3.2 | |
| General practitioner | 14 | 6.5 | |
| Health Officer | 7 | 3.2 | |
| B.Sc. Nurse | 15 | 6.9 | |
| Diploma Nurse | 16 | 7.4 | |
| B.Sc. Midwives | 123 | 56.9 | |
| Diploma Midwives | 30 | 13.9 | |
| IESO | 4 | 1.9 | |
| Health facility (n=216) | |||
| Hospital | 168 | 77.8 | |
| Health centre | 48 | 22.2 | |
| Service year (n=216) | |||
| <2 | 51 | 23.6 | |
| 2-5 | 53 | 24.5 | |
| >6 | 112 | 51.9 | |
| Working unit/ward (n=216) | |||
| Antenatal unit | 34 | 15.7 | |
| Labor ward | 154 | 71.3 | |
| Postnatal | 14 | 6.5 | |
| Family planning | 14 | 6.5 | |
| Professional number per shift (n=216) | |||
| 1 per shift | 9 | 4.2 | |
| 2 per shift | 47 | 21.8 | |
| 3 per shift | 42 | 19.4 | |
| 4 per shift | 19 | 8.8 | |
| 5 per shift | 18 | 8.3 | |
| 6 or more per shift | 81 | 37.5 | |
| Service training (n=216) | |||
| Yes | 127 | 58.8 | |
| No | 89 | 41.2 | |
| Received training (n=127) | |||
| BEmONC | 82 | 38 | |
| Advanced life support | 45 | 20.8 | |
Knowledge towards partograph utilization
When we consider knowledge towards partograph utilization all of 216(100%) the study participants heard about partograph and correctly know what partograph is. Concerning components of partograph all of 216(100%) the respondents know the different components of partograph. Majority 185(85.6%) of the study participants exactly know when to start plotting on the partograph during attending women in labor whereas more than half of 116(53.7%) obstetric care providers do not know the frequency to use partograph once active phase of labor started. Over all about 165(76.4%) of the study participants scored greater or equal to the mean score (4) indicating that this number of participants have good level of knowledge towards partograph utilization (Table 2).
| Variables Frequency Percent | |||
|---|---|---|---|
| Heard about partograph (n=216) | |||
| Yes | 216 | 100 | |
| No | 0 | 0 | |
| What partograph is (n=216) | |||
| A tool to be used in active phase of labor | 139 | 64.4 | |
| A graphic method of recording first stage of labor | 37 | 17.1 | |
| A silent feature of recording the whole process of labor | 40 | 18.5 | |
| Components of partograph (n=216) | |||
| Assessment of fetal wellbeing | 82 | 38 | |
| Assessment of maternal well being | 40 | 18.5 | |
| Assessment of labor progress | 94 | 43.5 | |
| When do you start plotting on partograph (n=216) | |||
| When labor is diagnosed | 16 | 7.4 | |
| At 4 cm cervical dilatation | 185 | 85.6 | |
| At 3 cm cervical dilatation | 15 | 6.9 | |
| How often used once active phase of labor started (n=216) | |||
| Once/30 minute | 100 | 46.3 | |
| Once/hour | 39 | 18.1 | |
| Once/4 hour | 69 | 31.9 | |
| Once/6 hour | 8 | 3.7 | |
| Variables Frequency Percent | |||
|---|---|---|---|
| Using partograph is beneficial for labouring women (n=216) | |||
| Strongly agree | 175 | 81 | |
| Agree | 36 | 16.7 | |
| Uncertain | 3 | 1.4 | |
| Disagree | 2 | 0.9 | |
| Partograph is very favourable in alerting skill birth attendant (n=216) | |||
| Strongly agree | 166 | 76.9 | |
| Agree | 41 | 19 | |
| Uncertain | 4 | 1.9 | |
| Disagree | 5 | 2.3 | |
| Using partograph care providers can able to identify problems (n=216) | |||
| Strongly agree | 160 | 74.1 | |
| Agree | 47 | 21.8 | |
| Disagree | 9 | 4.2 | |
| Skill birth attendant must use partograph on every mother (n=216) | |||
| Strongly agree | 130 | 60.2 | |
| Agree | 51 | 23.6 | |
| Disagree | 22 | 10.2 | |
| Strongly disagree | 13 | 6 | |
| Using partograph enables care providers perform basic intervention (n=216) | |||
| Strongly agree | 127 | 58.8 | |
| Agree | 66 | 30.6 | |
| Uncertain | 8 | 3.7 | |
| Disagree | 15 | 6.9 | |
| Using partograph is not beneficial as the estimate is exaggerated (n=216) | |||
| Strongly agree | 22 | 10.2 | |
| Agree | 34 | 15.7 | |
| Uncertain | 24 | 11.1 | |
| Disagree | 79 | 36.6 | |
| Strongly disagree | 57 | 26.4 | |
| Using partograph misleads management (n=216) | |||
| Strongly agree | 25 | 11.6 | |
| Agree | 37 | 17.1 | |
| Uncertain | 20 | 9.3 | |
| Disagree | 78 | 36.1 | |
| Strongly disagree | 56 | 25.9 | |
Attitude towards partograph utilization
Attitudes of study participants towards partograph utilization was assessed using attitude related questions. Majority 175 (81%) of the respondents strongly agree that following women in labor using partograph was beneficial. Around 166 (76.9%) of obstetric care providers strongly agree on the fact that partograph is very favorable for alerting skill birth attendant if there is any deviation from normal and also about 160 (74.1%) of the study participants strongly agree that using partograph health care provider can be able to identify problems and recognize complications early. From the total respondents half 51 (23.6%) of them agreed on the truth that every skill birth attendant must use partograph on every laboring mother and about 127 (58.8%) strongly agree on the fact of using partograph can enables health care providers perform essential basic interventions and make referrals to appropriate levels of care [6].
Among the total respondents seven tee nine (36.6%) of them disagree on the concept that using partograph is not beneficial as the estimate it gives is exaggerated. More than quarter 56 (25.9%) of obstetric care providers strongly disagree on the idea that using partograph misleads management as the progress of labor and the partograph alert line are not aligned in most laboring women.
Generally depending on the mean score (≥ 6) highest proportion 146(67.6%) of the study participants had favorable attitude towards partograph utilization whereas only 70(32.4%) of the participants had unfavorable attitude towards partograph utilization (Table 3).
Partograph utilization
According to our assessment on partograph utilization majority of 192(88.9%) the study participants stated that partograph is always available in their health facility. Two hundred six (95.4%) of the respondents consider partograph as useful in obstetric review and also around 161 (74.5%) responded that it is a managerial policy that all women in labor should monitored with a partograph (Table 4).
| Variables Frequency Percent | |||
|---|---|---|---|
| Partograph availability (n=216) | |||
| Yes | 192 | 88.9 | |
| No | 24 | 11.1 | |
| Do you use partograph to monitor labor (n=216) | |||
| Yes | 135 | 62.5 | |
| No | 81 | 37.5 | |
| If yes how often used | |||
| Routinely | 119 | 55.1 | |
| Rarely | 8 | 3.7 | |
| Occasionally | 8 | 3.7 | |
| Do you consider partograph useful in obstetric review (n=216) | |||
| Yes | 206 | 95.4 | |
| No | 10 | 4.6 | |
| Managerial policy that women should monitored with partograph, n=216 | |||
| Yes | 161 | 74.5 | |
| No | 55 | 25.5 | |
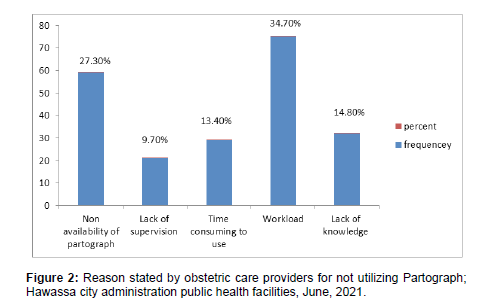
| What make difficult to use partograph (n=216) | |||
| Non availability of partograph | 59 | 27.3 | |
| Lack of supervision | 21 | 9.7 | |
| Time consuming to use | 29 | 13.4 | |
| Work load | 75 | 34.7 | |
| Lack of knowledge | 32 | 14.8 | |
From the total participants 135 (62.5%) (95%CI: 56%, 69%) of them utilized partograph to monitor women’s in labor (Figure 1). Among total study respondents more than half 119 (55.1%) of them used partograph routinely to monitor labor progress for. Regarding reason stated by obstetric care providers about 75 (34.7%) of them replied that workload was the major challenge which create difficulty for not using partograph among skill birth attendants (Figure 2).
Factors associated with partograph utilization among obstetric care providers
In bi variable analysis, variables with p-value less than 0.25 were considered as a candidate variable for multi variable analysis and run in multi variable analysis. Educational status, profession, health facility, service year, service training, knowledge, attitude, partograph availability, partograph in obstetric review, managerial policy and reason for not using partograph were identified as a candidate variable for multi variable analysis by yielding P value < 0.25. After multi variable analysis was preformed four variables (Educational status, profession, service training and attitude) showed significance association with partograph utilization with a p value of < 0.05 [7].
In multi variable analysis educational status were found to be statistically associated with partograph utilization of obstetric care providers (p < 0.05). Obstetric care providers with educational status of degree had 62% less likely of partograph utilization as compared to those with educational status of M.Sc and above [AOR 0.038; 95% CI: 0.003-0.506; p- value =0.013].
On the other hand respondent’s profession displayed significant association with partograph utilization (p<0.05). The odds of partograph utilization among study subjects whose profession was B.Sc Midwives were 9.9 times higher than that of study subjects whose profession was Obstetrician and Gynecologist [AOR 9.9; 95% CI: 1.06- 92.65; p-value=0.44] [8].
Similarly obstetric training was significantly associated with partograph utilization. The chance of partograph utilization was about 2.28 times higher for those care providers who had obstetric training than those care providers who had no any obstetric training [AOR 2.28; 95% CI: 1.1-4.7; p value = 0.029].
Additionally attitude towards partograph utilization showed strong statistical association with partograph utilization (p<0.01). Relative to obstetric care providers with unfavorable attitude towards partograph utilization obstetric care providers with favorable attitude had 3.7 times more likely to utilize partograph for monitoring labor [AOR = 3.7; 95% CI: 1.76-7.83 ; p value =0.001] (Table 5).
| Variables | Partograph utilization | 95% CI | ||
|---|---|---|---|---|
| Utilized | Not utilized | COR(95% CI) | AOR(95% CI) | |
| Educational status | ||||
| Diploma | 33(76.7) | 10(23.3) | 0.419(0.193-0.908)* | 0.14(0.008-2.6) |
| Degree | 94(58) | 68(42) | 0.808(0.18-3.635) | 0.04(0.003-0.51)* |
| M.Sc and above | 8(72.7) | 3(27.3) | 1 | 1 |
| Profession | ||||
| Obstetrician/gynaecologist | 3(42.9) | 4(57.1) | 1 | 1 |
| General practitioner | 7(50) | 7(50) | 1.33(0.214-8.28) | 5.99(0.55-64.9) |
| Health officer | 4(57.1) | 3(42.9) | 1.77(0.214-14.7) | 2(0.14-31.56) |
| BSc Nurse | 10(66.7) | 5(33.3) | 2.66(0.42-16.8) | 17.5(1.37-224.67)* |
| Diploma Nurse | 10(62.5) | 6(37.5) | 2.2(0.36-13.5) | 2.72(0.22-33.43) |
| BSc Midwives | 76(61.8) | 47(38.2) | 2.15(0.462-10.06) | 9.9(1-92.6)* |
| Diploma Midwives | 22(73.3) | 8(26.7) | 3.66(0.67-20) | 6.8(0.57-81.34) |
| IESO | 3(75) | 1(25) | 4(0.26-60.3) | 0.6(0.2-15.4) |
| Health facility | ||||
| Hospital | 99(58.9) | 69(41.1) | 1 | 1 |
| Health centre | 36(75) | 12(25) | 2.091(1.016-4.304)* | 1.8(0.74-4.38) |
| Service year | ||||
| < 2 | 28(54.9) | 23(45.1) | 1 | 1 |
| 2-5 | 35(66) | 18(34) | 1.597(0.723-3.527) | 1.24(0.44-3.5) |
| > 6 | 72(64.3) | 40(35.7) | 1.479(0.754-2.9) | 1.25(0.48-3.23) |
| Service training | ||||
| Yes | 84(66.1) | 43(33.9) | 1.456(0.833-2.543) | 2.28(1.09-4.76)* |
| No | 51(57.3) | 38(42.7) | 1 | 1 |
| Knowledge | ||||
| Good knowledge | 99(60) | 66(40) | 0.625(0.357-1.231) | 0.54(0.23-1.24) |
| Poor knowledge | 36(70.6) | 15(29.4) | 1 | 1 |
| Attitude | ||||
| Favourable | 99(67.8) | 47(32.2) | 1.989(1.11-3.565)* | 3.7(1.76-7.8)** |
| Un favourable | 36(51.4) | 34(48.6) | 1 | 1 |
| Partograph availability | ||||
| Yes | 125(65.1) | 67(34.9) | 2.612(1.1-6.12)* | 2.8(0.96-8.12) |
| No | 10(41.7) | 14(58.3) | 1 | 1 |
| Partograph in obstetric review | ||||
| Yes | 126(61.2) | 80(38.8) | 0.175(0.022-1.408) | 0.11(0.01-1.08) |
| No | 9(90) | 1(10) | 1 | 1 |
| Managerial policy | ||||
| Yes | 95(59) | 66(41) | 0.54(0.276-1.056) | 0.55(0.23-1.27) |
| No | 40(72.7) | 15(27.3) | 1 | 1 |
| Reason for not utilizing partograph | ||||
| Non availability of partograph | 40(67.8) | 19(32.2) | 1 | 1 |
| Lack of supervision | 11(52.4) | 10(47.6) | 0.522(0.189-1.443) | 0.47(0.14-1.58) |
| Time consuming | 21(72.4) | 8(27.6) | 1.247(0.468-3.324) | 0.8(0.26-2.53) |
| Workload | 38(50.7) | 37(49.3) | 0.488(0.24-0.992)* | 0.45(0.2-1) |
| Lack of knowledge | 25(78.1) | 7(21.9) | 1.7(0.624-4.613) | 1.57(0.5-4.9) |
| *=p<0.05 statistically significant, **=p<0.01 Statistical association, ***=p<0.001 Strong statistical association; COR=Crude Odds Ratio, AOR=Adjusted Odds Ratio, =Confidence Interval, 1=Reference category | ||||
Discussion
This study attempted to identify utilization of partograph and associated factor among obstetric care providers in public health facilities of Hawassa city administration.
In this study 62.5% of the study participants utilized partograph for monitoring progress of labor. Educational status of respondents, profession, service training and attitude towards partograph utilization were significant factors associated with partograph utilization.
It is known that partograph utilization is so important for early identification of problems, complications and early referral; in turn it is essential for good maternal and fetal outcomes. In our study about 62.5% (95%CI: 56%, 69%) of the study participants utilized partograph in order to follow labor which is consistent with the result from Addis Ababa (57.3%) and comparable with that of East Gojjam (53.85%).
The result of the present study also showed that level of partograph utilization greater than from the study conducted in North Shoa and South West Nigeria (40.2%,32.3%) respectively. and less than from that of Eastern zone of Tigray (83%). The difference between these studies may emanate from difference in sample size and time variation between the studies; since obstetric training and supportive supervisions increased through time which in turn promote knowledge of obstetric care providers to actively utilize partograph. In the other side this difference may arise from variation in knowledge level of the study participants and also from their profession since in our study majority (76.4%) of the respondents had good level of knowledge and greater than half (56.9%) of the respondents were Midwives indicating the chance for utilization of partograph.
The finding of our study indicated that 76.4% of obstetric care providers had good level of knowledge implying that this finding is consistent with the finding from North Shoa (70.5%). This finding is also comparable with result from Central Zone of Tigray (68.2%) [18] but higher than from that of Eastern Gojam (56.04%) and Cameroon (29.6%) respectively. The possible reason for this variation may be difference in the study area, time gap between the studies and data collection procedures.
Concerning attitude towards partograph utilization about 67.6% of the study participants had favorable attitude on partograph utilization during monitoring labor. This result is in agreement with the study finding from Central Zone of Tigray (67.7%). However the finding of our study is lower than from that of North Shoa Zone (83.6%) and higher than from that of Wolaita Zone (42.1%) respectively [9].
The finding of our study identified that educational status have significant association with partograph utilization during monitoring labor in which obstetric care providers with educational status of degree had 62% less likely to utilize partograph as compared to those with educational status of MSc and above. Similar finding was observed in a study done in East Gojam Zone, Eastern Zone of Tigray and Wolaita Zone. The possible explanation will be most of the obstetric care providers who holds a degree were Midwives who got obstetric training and routinely work in obstetric wards; this experience leads them to properly utilize partograph during monitoring labor. However studies from Central Zone of Tigray contradicts with this finding indicating that educational status of study participants had no significance influence on partograph utilization.
Our study also identified that respondent’s profession had statistical association with partograph utilization. Respondents who are B.Sc Midwives were 10 times more likely to utilize partograph compared to Obstetricians/Gynecologists. This finding is similar with result from a study in North Shoa Zone and Eastern Zone of Tigray. This might be due to the fact that Midwife obstetric care providers had more of chance of being assigned in delivery wards and consequently received training on partograph utilization which might in turn have improved their knowledge and skills to utilize partograph than others.
Similarly this study demonstrated that service training had showed significance association with partograph utilization implying that obstetric care providers who took service training had 2.3 times more chance of partograph utilization than their counter parts. This finding is supported by the study conducted in Central Zone of Tigray, Addis Ababa, North Shoa, East Gojam and Eastern Zone of Tigray. A study finding from Cameroon is in contrary with the current study implying that service training had no a determinable effect on partograph utilization. This discrepancy might be due to difference in the study setting, time and sample size.
Furthermore this study also showed that attitude had strongly statistically associated with partograph utilization during monitoring labor. Relative to obstetric care providers with unfavorable attitude obstetric care providers with favorable attitude had 3.7 times more likely to utilize partograph. Similar findings had been reported from a study in Addis Ababa and North Shoa. However this result is in contrast with the study from Central Zone of Tigray in which attitude of study participants had no any effect on partograph utilization [10].
Conclusion
Based on the result of this study about 62.5% of the study participants utilize partograph for monitoring labor whereas 37.5% of them had not utilized it.
This study also showed that educational status, profession, service training and attitude were significantly associated with partograph utilization during monitoring progress of labor. The concerned bodies should strengthen supportive supervision and provide training to obstetric care providers in order to promote partograph utilization for monitoring labor.
List of Abbreviations
BEmONC: Basic Emergency Obstetric and New born Care, EDHS: Ethiopian Demographic and Health Survey, FMOH: Federal Ministry of Health, HEWs: Health Extension Workers, MDGs: Millennium Development Goals, MNH: Maternal and Neonatal Health, MMR: Maternal Mortality Rate, NGO: Non-Governmental Organization,OCGs: Obstetric Care Giver, PHCU: Primary Health Care Unit, PI: Principal Investigator, UNICEF: United Nations Children’s Fund, WHO: World Health Organization.
Declaration
Ethical Consideration
Ethical clearance was obtained from Hawassa City Health Department. Permission letter from the health facilities were obtained to undertake the study. Informed consent was taken from each study participant before interview administration. Honesty and confidentiality were maintained with the right not to participate in the study.
Consent for Publication
Not applicable
Availability of Data and Materials
Data is not available for online access, however, readers who wish to gain access to the data can write to the corresponding author Molore Inaro Dola.
Competing Interests
The authors declare that they have no competing interests
Funding
The authors received no specific funding for this study
Authors’ Contributions
Both MED and HEZ participated in planning the study, writing proposal, monitoring data collection process and also in analyzing the data, writing the result and the manuscript. Both authors agreed to be accountable for all aspects of the work. Both authors read and approved the final manuscript.
Acknowledgement
We would like to thank data collectors, study participants, Hawassa city Health Department.
References
- Opoku BK, Nguah SB (2015) Utilization of the modifid WHO partograph in assessing the progress of labour in a metropolitan area in Ghana. Res J Womens Health 2.
- Berhan Y, Berhan A (2014) Causes of maternal mortality in Ethiopia: A significant decline in abortion related death. Ethiop J Health Sci 24: 15-28.
- Magon N (2011) Partograph Revisited Investig. Int J Clin Cases Investig 3: 1-6.
- Sena B, Kitila A, Ashagire M, Nemera G (2014) Utilization of Partograph during Labour and Birth Outcomes at Jimma University. J Preg Child Health 1: 1-6.
- Matewes M (2009) The partograph for the prevention of obstructed labour. Clinical Obstetric Gynecology 52: 256-269.
- Margaret M, Opiah A, Ekere JE, Emmanuel M (2012) Knowledge and Utilization of the Partograph among Midwives in the Niger Delta Region of Nigeria. Afr J Reprod Health 16: 126.
- Fantu AD, Worku A, Tadesse E (2013) Assessment of knowledge and utilization of the partograph among health professionals in Amhara region, Ethiopia. Sci J Clin Med 2: 26-42.
- Engida YB, Ayalew A, Nebreed F (2013) Knowledge and utilization of partograph among obstetric care givers in public health institutions of Addis Ababa, Ethiopia. Pregnancy and Childbirth 13: 1-9.
- Negash WA, Marta B, Gizachew AT (2015) Partograph utilization and associated factors among obstetric care providers in North Shoa Zone, Central Ethiopia: A cross sectional study. Afr Health Sci 15: 553-559.
- Fawole A, Hunyinbo K, Adekanle D (2008) Knowledge and utilization of the partograph among obstetric care givers in South West Nigeria. Afr J Reprod Health 12: 1-8.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Dola MI, Zewdie HE (2022) Partograph Utilization and Associated Factors among Obstetric Caregivers in Public Health Facilities of Hawassa City Administration, Sidama State, Ethiopia, 2021. J Preg Child Health 9: 540. DOI: 10.4172/2376-127X.1000540
Copyright: © 2022 Dola MI, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2159
- [From(publication date): 0-2022 - Dec 08, 2025]
- Breakdown by view type
- HTML page views: 1688
- PDF downloads: 471