Pathological Fracture as a Complication of Cystic Degeneration of Parathyroid Adenoma
Received: 06-Aug-2020 / Accepted Date: 24-Aug-2020 / Published Date: 31-Aug-2020 DOI: 10.4172/2167-7964.1000330
Abstract
Parathyroid cystic adenomas are often misdiagnosed as thyroid cysts. We report a case of haemorrhagic cystic parathyroid adenoma, which presented a diagnostic challenge that led to life-threatening complications. A 46-yearold man who was mis-diagnosed as having a thyroid follicular cyst 4 months ago, presented with pathological fracture right neck femur. Laboratory investigations revealed increased serum calcium, parathyroid hormone, and impaired renal function. Ultrasound examination of the neck showed complex cystic lesion related to the left thyroid lobe. He had medical treatment of hypercalcaemia followed by surgical excision of a 5.5 cm cystic neck mass. He stayed in hospital for 6 months during which the calcium and parathormone returned to normal, his fracture healed, and the bone texture had improved.
Keywords: Case report; Cyst; Adenoma; Hyperparathyroidism; Ultrasound
Introduction
Primary hyperparathyroidism (PHPT) is usually diagnosed as an incidental finding of raised serum calcium or due to symptoms secondary to hypercalcemia [1]. The occurrence of bone lesions such as pathologic fractures in PHPT is now rare since methods to measure serum calcium became available routinely [2]. Cystic degeneration of parathyroid adenoma is seen in 1-2% of patients with primary hyperparathyroidism [3,4]. The clinical manifestations of functional cystic parathyroid adenoma are usually similar to those of nondegenerated adenomas and include a biochemical profile consistent with that of primary hyperparathyroidism and a broad array of symptoms, including fatigue, depression, nephrolithiasis, osteoporosis, and abdominal pain. As have their solid counterparts, cystic adenomas have been reported to occur in hypercalcaemic crisis as the result of acute necrosis or haemorrhage of a parathyroid adenoma [5]. The clinical presentation of parathyroid cyst frequently resembles thyroid nodules leading the clinician to mistakenly believe that thyroid disease is involved [6]. Although imaging is a useful part of the preoperative assessment of such lesions, there are no specific radiological methods for differentiating parathyroid cysts from other cystic neck lesions. Ultrasonography may reveal a non-specific cystic structure. Computerised tomography (CT) and MRI may demonstrate the cystic component of these lesions and help to visualise the relationship with adjacent tissues which are particularly useful in the presence of substernal extension or compressive symptoms, they may also be employed when a diagnosis cannot be reached using ultrasound guided FNA, if malignancy is suspected, or for preoperative planning [7].
Case Report
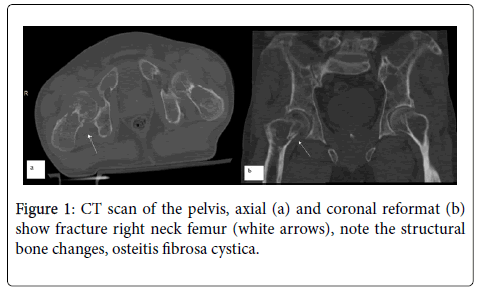
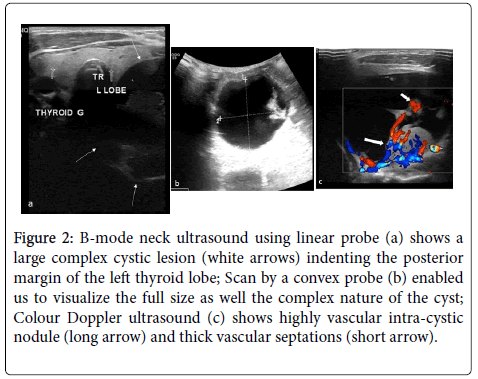
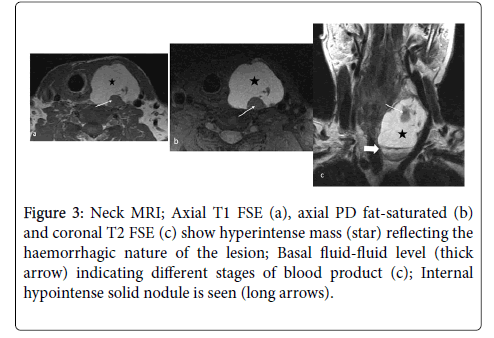
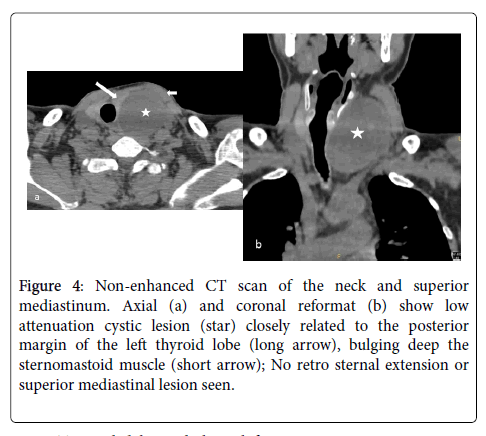
A 46-year-old man had a history of rapidly growing neck swelling four months ago, but he was not properly worked up. An ultrasound guided FNA cytology was done, diagnosed as thyroid follicular cyst, his thyroid function was normal, and no further treatment was recommended. He presented to our emergency department with fracture right neck femur, CT scan of pelvis and proximal femur (Figure 1) confirmed the fracture and showed diffuse structural bony changes. His laboratory results disclosed the following values: Ca 3.9 mmol/L (2.15-2.55), calculated Ca2+ 4.1mmol/L, phosphorous 1.58 mmol/L (0.78-1.53), parathormone 337.80 pmol/L (1.30-6.80), Alkaline phosphatase 1408 IU/L. Serum creatinine 212 μmol/L (57-113), urea 12.7 mmol/L (2.9-7.1), M-TP 2.37 g/24.0 hrs urine (<0.15). WBC 19.2 109 /L (4.23-9.07), RBC 4.01 1012 /L (4.63-6.08), Hb 111g/L (137-175), Hct 0.332 L/L (0.4-0.51), Platelets 462 109 /L (140-400), ESR 85. An ultrasound examination of the neck revealed a large complex cystic lesion 6x4cm on the left side of the neck indenting the left thyroid lobe (Figure 2), colour Doppler showed highly vascular solid nodule and vascular thick septations. MRI of the neck revealed 7×5×4 cm cyst on the left side of the neck hyperintense on T1suggested acute haemorrhage (Figure 3), the lesion showed solid nodule adherent to its thin wall, it displaced and indented the left thyroid lobe with no line of cleavage in-between. CT scan of the neck and superior mediastinum (Figure 4) revealed left sided cystic neck lesion displacing the trachea, no retrosternal extension or superior mediastinal lesion. These findings led to a diagnosis of haemorrhagic functional parathyroid adenoma. Abdominal ultrasound showed bilateral renal calculi within echogenic kidneys. The patient was temporary referred to the ICU where he had medical support for hypercalcemia by IV fluid 125 ml/hr guided by fluid chart, encouraged oral fluid, Calcitonin injection 200 units SC/8 hrs, Zometa 4 mg in 250 ml (0.9% NaCl) over 4 hrs, NaHCO3 tab 1 gm and Aldomet tab 250 mg.
Figure 2: B-mode neck ultrasound using linear probe (a) shows a large complex cystic lesion (white arrows) indenting the posterior margin of the left thyroid lobe; Scan by a convex probe (b) enabled us to visualize the full size as well the complex nature of the cyst; Colour Doppler ultrasound (c) shows highly vascular intra-cystic nodule (long arrow) and thick vascular septations (short arrow).
Figure 3: Neck MRI; Axial T1 FSE (a), axial PD fat-saturated (b) and coronal T2 FSE (c) show hyperintense mass (star) reflecting the haemorrhagic nature of the lesion; Basal fluid-fluid level (thick arrow) indicating different stages of blood product (c); Internal hypointense solid nodule is seen (long arrows).
Figure 4: Non-enhanced CT scan of the neck and superior mediastinum. Axial (a) and coronal reformat (b) show low attenuation cystic lesion (star) closely related to the posterior margin of the left thyroid lobe (long arrow), bulging deep the sternomastoid muscle (short arrow); No retro sternal extension or superior mediastinal lesion seen.
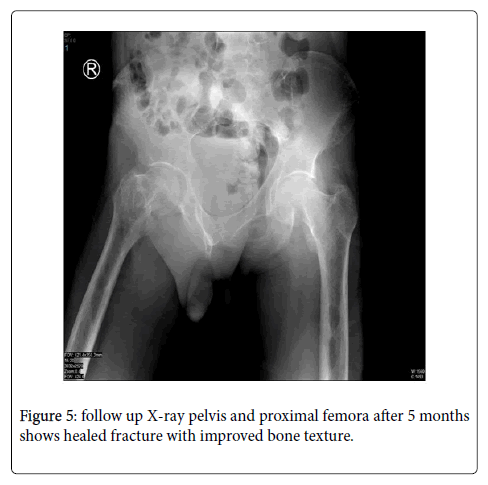
During the hospital stay, he had x-rays for skull, hands, chest, both knees and proximal tibia showed the osseous manifestations of PHPT, he also had 18F-NaF whole-body PET/CT which revealed metabolic super-scan. After about one month of medical support, surgical removal of the cystic neck lesion was done by ENT surgeon, a 5.5 cm cystic mass contain dark coloured fluid was removed. Histopathology showed parathyroid adenoma with cystic degeneration and no evidence of malignant cells. The clinical and biochemical profile of our patient normalized few days after surgery. The patient stayed in hospital for 6 months, during which the bone texture has improved (Figure 5) and the fracture healed but with residual degree of impaired renal function.
Discussion
Cystic parathyroid adenomas are reported to be rare and account for 1-2% of PHPT cases [8]. Previous reports have suggested that nonfunctional cysts tend to be unilocular and contain clear fluid, while functional cysts have more complex cystic features and often contain cloudy brown fluid, suggesting previous haemorrhage. This gross appearance supports the theory that most functional parathyroid cysts originate from haemorrhage and cystic degeneration of parathyroid adenomas [9,10].
Since parathyroid cysts are rare clinical entity in routine practice [11], our case was diagnosed as having thyroid cyst. Thyroid function test was done but neither parathyroid hormone assay nor the level of PTH in the cystic fluid was measured.
Ultrasound findings of our case showed that the cyst was inseparable from the thyroid which was atypical for a parathyroid cyst. In a study conducted by Nathan et al [12], it describes the sonographic appearance of 15 cases of cystic parathyroid adenoma: 14 of them appeared to originate from extra thyroid origin and one cyst deformed the posterior border of the overlying thyroid. On colour Doppler the solid nodule and the thick septations were highly vascular, typical of the appearance of the cystic adenoma documented in previous literature [13]. Sonography is crucial in these cases as a primary tool for diagnosis of any neck swelling. The sonographer may have to determine whether a cystic neck lesion is a parathyroid adenoma, cystic thyroid nodule, or other rare cystic neck lesion. The misdiagnosis of cystic parathyroid adenoma as a thyroid nodule or other cystic neck lesion can lead to more-invasive surgery (e.g., four gland parathyroid exploration versus minimally invasive parathyroidectomy) or delay in treatment if the parathyroid adenoma is dismissed as a thyroid cyst [12].
PHPT revealed by pathological fracture, as in our case, is very uncommon [13,14], he had fractured the right neck femur. CT scan (Figure 1) showed all the signs of PHPT, reduced bone density, osteitis fibrosa cystica, sub-ligamentous and subcortical erosions. Follow up XCitation rays after surgical removal of the lesion showed healing of the fracture and improvement in the bone texture (Figure 5).
MRI and CT on the neck were done as a preoperative plan. The localization of the mass, its accurate size and the haemorrhagic nature of the cyst, as well the relationship with surrounding structures are shown on MRI with high soft tissue resolution (Figure 3), CT was done to exclude any superior mediastinal lesion (Figure 4). We refrained from giving any contrast due to renal impairment. CT and MRI are particularly useful for preoperative planning to visualise the relationship with adjacent tissues or the presence of substernal extension [7]. In Conclusion, parathyroid cysts are uncommon, they have atypical sonographic appearance. Awareness of this entity with clinical and biochemical correlation and further ultrasound-guided aspiration of cyst fluid with PTH assay can lead to an accurate diagnosis of parathyroid disease sparing the patient from irreversible complications.
References
- Rachha R (2008) Pathological fractures as the presenting symptom of parathyroid adenoma: a report of three cases BJMP 1:26-29.
- Khaoula BA, Kaouther BA, Ines C (2011) An unusual presentation of primary
- Â hyperparathyroidism: pathological fracture. Case Reports in Orthopedics 1-3.
- McCoy KL, Yim JH, Zuckerbraun BS (2009) Cystic parathyroid lesions: functional and non-functional parathyroid cysts. Arch Surg 144:52-56.
- Calandra DB, Shah KH, Prinz RA (1983) Parathyroid cysts: a report of eleven cases including two associated with hyperparathyroid crisis. Surgery 94:887-892.
- Goomany A, Rafferty A, Smith I (2015) An Unusual Neck Mass: a Case of a Parathyroid Cyst and Review of the Literature Case Reports in Surgery 1-4.
- Ujiki M, Sturgeon C, Nayar R (2007) Parathyroid cyst: often mistaken for a thyroid cyst. World Journal of Surgery 31:60-64.
- Makino T, Sugimoto T, Kaji H (2003) Functional giant parathyroid cyst with high concentration of CA19-9 in cystic fluid. Endocrine Journal 50:215-219.
- Ippolito G, Palazzo FF, Sebag F (2006) A single-institution 25-year review of true parathyroid cysts. Langenbecks Arch Surg 391:13-18.
- Pacini F, Antonelli A, Lari R (1985) Unsuspected parathyroid cysts diagnosed by measurement of thyroglobulin and parathyroid hormone concentrations in fluid aspirates. Ann Intern Med 102:793-794.
- Cappelli C, Rotondi M, Pirolaetal I (2009) Prevalence of parathyroid cysts by neck ultrasound scan in unselected patients. J Endocrinol Invest 32:357-359.
- Johnson NA, Yip L, Tublin ME (2010) Cystic Parathyroid Adenoma: sonographic Features and Correlation With 99mTc-Sestamibi SPECT Findings. AJR 195:1385-1390.
- Morgan G, Ganapathi M, Afzal S (2002) Pathological fractures in primary hyperparathyroidism: a case report highlighting diagnostic difficulties. Injury 33:288-291.
Citation: Amr HA, Eldesouky IM (2020) Pathological Fracture as a Complication of Cystic Degeneration of Parathyroid Adenoma. OMICS J Radiol 9: 1000330 DOI: 10.4172/2167-7964.1000330
Copyright: © 2020 Hanan Abdulaziz Amr, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 3778
- [From(publication date): 0-2020 - Dec 16, 2025]
- Breakdown by view type
- HTML page views: 2868
- PDF downloads: 910