Patterns and Severity of COVID-19 among Sudanese Patients Using High Resolution Computed Tomography at Jabra Isolation Center
Received: 25-May-2022 / Manuscript No. roa-22-64845 / Editor assigned: 27-May-2022 / PreQC No. roa-22-64845 (PQ) / Reviewed: 19-Jul-2022 / QC No. roa-22-64845 / Revised: 24-Jul-2022 / Manuscript No. roa-22-64845 (R) / Published Date: 31-Jul-2022 DOI: 10.4172/2167-7964.1000391
Abstract
Background: After the spread of COVID-19, chest CT examination became used as a complement to RT-PCR for diagnose and follow up as a rapid tool when RTPCR results are unavailable.
Objective: aimed to characterize the patterns and severity of COVID-19 using high resolution computed tomography among Sudanese patients in Jabra Isolation Center, Khartoum State.
Materials and Methods: A total of 50 patients with COVID-19 confirmed by a positive from RT-PCR who underwent chest CT were enrolled in the study. Clinical and laboratory data were collected by reviewing the hard medical records. Radiology abnormalities were categorized based upon the patterns and distribution within the lungs. The CT-SS was defined by summing up individual scores from 6 lung regions; rated by Likert scale as 0 (0%), 1 (1-25%), 2 (26-50%), 3 (51-75%), or 4 (76-100%). The total severity score was reached by summing the sex lobe scores into mild and severe cases.
Results: (33 were men and 17 were women, 26 patients have more than 60 years, they were the majority age group, 28 cases with mild and 22 cases with severe disease). Study found that (COVID-19) was distributed as Multi-lesions in 46 cases (92%), bilaterally, and diffused within the lung fields in (39.77%, 41.81% respectively). Peripheral ground glass opacities patterns (GGOs) were the most common feature. There was a significant difference in distribution of disease between right and left lungs (p<0.05). Where the right lung was the most infected in both mild and severe cases. The lower lobes of both lungs were the most involved sites by COVID-19 in compare with the upper and middle lobes in both lungs.
Conclusions: Thin-section high-resolution chest CT is an essential modality for detection of lung abnormalities in COVID-19. The semi-quantitative CT scoring system for COVID-19 can be used to evaluate the severity of pulmonary involvement quickly and objectively.
Keywords: COVID-19; Computed tomography; RNA virus; Corona Virus
Introduction
Corona Virus Disease 2019 (COVID-19) is a fast infectious spreading viral disease caused by Severe Acute Respiratory Syndrome Corona Virus (SARS- CoV-2) an RNA virus with a crown like appearance. It transmits from one to another primarily via respiratory droplets [1]. On 31th December, 2019, the World Health Organization (WHO) reported several cases of viral pneumonia with unknown etiology in Wuhan, Hubei Province, China. Globally, There have been 470 839 745 confirmed cases and 6092 933 confirmed deaths from this disease as of March 22, 2022 [2]. COVID-19 has infected millions of people around the world and continues to threaten many more [3] has reached Sudan on mid of March 2020, and by the end of March 2022 there are 61,842 confirmed cases and 4,897 total deaths [4]. The major symptoms of COVID-19 such as cough, fever, fatigue, and dyspnea can help in early disease detection and preventing it from spreading to others Clinical, laboratory, and radiologic parameters are used to classify COVID-19 severity [5,6]. Due to its advantages as a specific and easy qualitative test, real time reverse transcriptase-PCR (RT-PCR) is of significant interest nowadays for the detection of SARS-CoV-2 [7]. Chest CT scan have an important role in the diagnosing and follow-up of patients with COVID-19. Variant studies have stated the radiographic abnormalities changes in the acute course of COVID-19 , which range from mild to severe cases [8,9]. So, the combination of real-time RTPCR and clinical features, especially CT imaging, can make disease management easier [10].
In interstitial lung disease and pneumonia, a high-resolution CT severity score system was widely employed for medical decisionmaking and prognosis [11,12]. As well as the chest CT findings of COVID-19 are reported in a variety of literatures as multiple ground glass opacity, consolidation and interlobular septal thickening in both lungs which are predominantly dispersed beneath the pleura [13].
However, because there have been few published investigations in this area in Sudan, this work might be the first to use high-resolution computed tomography to assess COVID-19 patterns and severity. As a result, we believe that our findings would be useful in establishing a local standard for COVID-19 patterns and severity among Sudanese patients in Jabra Isolation Center, Khartoum State.
Material and Methods
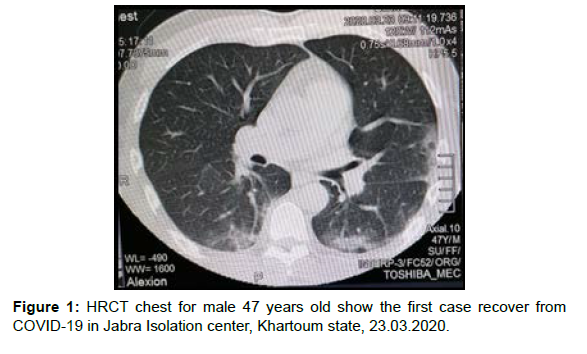
The study was approved by the Diagnostic radiology department, college of medical radiological science, Sudan University of science and technology and Khartoum state ministry of health under number (WKH/WS/1ATAA/44/A). This was conducted at a single-center, retrospective, observational study between September 21, 2021 and February 13, 2022 at Jabra Isolation center. This hospital was chosen because it is Sudan’s first and largest COVID-19 isolation center, as well as an international center accredited by the Federal Ministry of Health and the World Health Organization. This study included 50 adult patients who tested positive for COVID-19 infection by realtime reverse transcriptase polymerase chain reaction (rRT-PCR) and performed a chest HRCT scan, excluding those with lung cancer, a history of lobectomy, tuberculosis, or atelectasis. Patients’ medical record names were hidden from data handlers while demographic data, clinical presentations, and medical histories were collected. Two radiologists with more than three years of experience independently assessed HRCT radiographic images while being blinded to the patients’ clinical data (Figure 1).
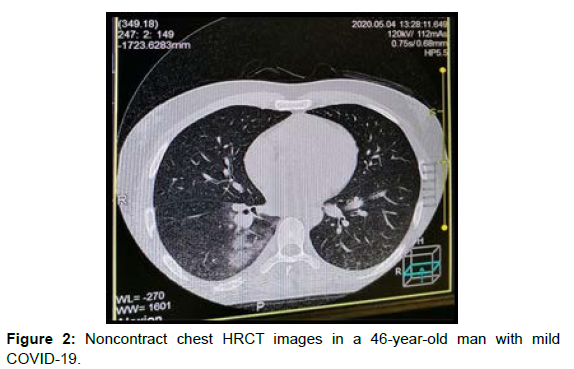
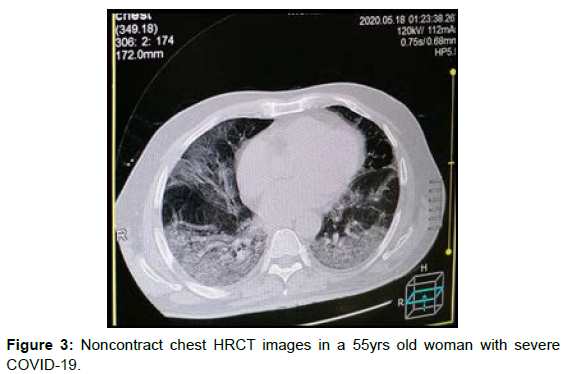
The cross sectional radiographic HRCT images were independently assessed, and the final decisions were made by consensus. The abnormal features of chest HRCT imaging were quantitatively evaluated. Two radiologists evaluated the abnormal imaging findings (Single, Multiple, Unilateral, Bilateral, Localized, Diffused, Patchy, Nodular, Peripheral Ground Glass Opacities (GGOs), Consolidation, interlobular septal thickening and Sub-plural band). COVID-19- related lymphadenopathy, pulmonary fibrosis, pleural effusion, and emphysema pula were all ruled out. The radiologists calculated the lesion areas on each lung lobe as a percent of the overall lung lobe area. The lung was divided into six zones by the level of tracheal carina and the level of inferior pulmonary vein bilaterally on CT images, and the percentages in each lung lobe were scored using a semi- quantitative visual scoring system (CT-SS) to identify the severity of COVID-19 disease. GGOs (ground-glass opacities) were assessed on a 0-4 Likert scale. (0=absent; 1=1-25%; 2= 26-50%; 3= 51-75%; 4=76-100%). The cumulative score of six zones has been used to compute the global severity score for each targeted pattern [14]. Mild cases are those with 1 to 12 total scores, while severe cases are those with 13 to 24 total scores (Figures 2 and 3).
All CT scans were performed with all patients in the supine position and holding their breath at the end of inhalation. The scan parameters are: Tube voltage 120 kV, tube current 110 mA, pitch 1.0, rotation time 0.5 s to 0.75 s, slice thickness 5 mm, slice thickness 1 mm or 1.5 mm for axial reconstruction, coronal sagittal reconstruction with 64 slices of spiral computed tomography scanner (TOSHIBA Aquilion CT unit) installed in 2012.
Statistical Analysis
All statistical analyzes were performed by Statistical Products and Services software (SPSS Statistics, version 26.0, Chicago, IL, USA). 0.05 was considered to demonstrate statistical significance. Categorical variables are expressed as frequencies and percentages using cross tabulation statistic. Fisher’s exact test was used to compare scores of each lung lobe between the light and severe groups, where the weighted kappa coefficient was used to compare the consistency of two observers in each lung lobe compare the left and right lung scores, upper lobe scores, middle lobe scores and lower lobe scores using the mean and student’s t-test to identify significant differences.
Results
There were 33 (66%) men and 17 (34%) women. Ages were categorized into three groups, the majority of patients over 60 years of age 26 (52%) and 20 (40%) between 40 and 59 years of age. Depending on signs and symptoms, patients with cough, fever, hypoxemia and SOB were the common clinical presentations (29; 58%, 28; 56%, 14; 28% and 13; 26%, respectively). The prevalence of hypertension and diabetes was (18; 36% and 18; 36%). COVID19 was distributed as multiple lesions in 46 (92%) cases, bilateral and diffuse in (39; 77%, 41; 81%, respectively) in the lung field, having patchy pattern in 42 (84%) cases. ground glass opacity (GGO) was found in 46 (92%) cases. Consolidations are found in 20 (40%) cases. The sample was divided into two groups; Mild cases were 28 (56%) and severe cases were 22 (44%). There was a significant difference between the lung opacity scores of the mild group and the severe group in each lung lobe (P < 0.05). In which the right lung was infected the most in the mild and severe group with the mean value (4.46; 8.68) compared with the left lung (2.96; 8.00, respectively) with the significant difference in the two comparisons (P= 0.00) (Tables 1-4).
| Variables | CT-SS | ||
|---|---|---|---|
| Gender | Total (n = 50) (%) | Mild(n=28) (N; %) |
Severe(n=22) (N; %) |
| Male | 33 (66%) | (17; 60.71%) | (16; 72.72%) |
| Female | 17 (34%) | (11; 39.28%) | (6; 27.27%) |
| Age | |||
| 20-39 years | 4 (8%) | (3; 10.71%) | (1; 4.45%) |
| 40-59 years | 20 (40%) | (10; 35.71%) | (10; 45.45%) |
| More than 60 years | 26 (52%) | (15; 53.57%) | (11; 50.00%) |
| Clinical Presentations | |||
| SOB | 13 (26%) | (20; 71.42%) | (17; 77.27%) |
| Chest pain | 3 (6%) | (2; 7.14%) | (1; 4.45%) |
| Fever | 28 (56%) | (14; 50.00%) | (14; 63.63%) |
| Cough | 29 (58%) | (16; 57.14%) | (13; 59.09%) |
| Headache | 6 (12%) | (1; 3.57%) | (5; 22.72%) |
| Fatigue | 13 (26%) | (6; 21.42%) | (7; 31.81%) |
| Hypoxia | 14 (28%) | (10; 35.71%) | (4; 18.18%) |
| Medical History | |||
| Hypertension | 18 (36%) | (10; 35.71%) | (8; 36.36%) |
| DM | 18 (36%) | (11; 39.28%) | (7; 31.81%) |
| No Dis | 9 (18%) | (3; 10.71%) | (1; 4.45%) |
| CHD | 5 (10%) | (0; 00.00%) | (1; 4.45%) |
Table 1: Demographic and Clinical Data of 50 Patients with COVID-19.
| Variables | Disease severity, n (%) | P value | ||
|---|---|---|---|---|
| Mild (n=28) |
Severe (n=22) |
|||
| Lesion Number | Single | (4; 14.28%) | (0; 00.00%) | 0.065 |
| Multi | (24;85.71) | (22; 100%) | ||
| Uni-lateral | (9; 32.14%) | (0; 00.00%) | 0.003 | |
| Bi-lateral | (17; 60.71%) | (22; 100%) | 0.001 | |
| Localized | (8; 28.57%) | (0; 00.00%) | 0.006 | |
| Diffused | 19; 67.85%) | (22; 100%) | 0.003 | |
| Nodular | (6; 21.42%) | (3; 13.63%) | 0.477 | |
| Patchy | (22; 78.57%) | (20; 90.90%) | 0.238 | |
| Peripheral GGOs | (25; 89.82%) | (21; 95.45%) | 0.425 | |
| Sub-plural band | (3; 10.71%) | (0; 00.00%) | 0.113 | |
| Consolidation | (7; 25.00) | (13; 59.09%) | 0.015 | |
| Inter-lobular septal Thickness | (4; 14.28%) | (0; 00.00%) | 0.065 | |
| Using cross tabulation, Chi square | ||||
Table 2: Final radiographic images diagnoses of HRCT.
| Lung Lobe | Frequency (n=50) | Mild (n=28) | Severe (n=22) | P Value | Kappa |
|---|---|---|---|---|---|
| Left Upper Lobe (LUL) | |||||
| 0 | 17 | 15 (53.57%) | 1 (4.54%) | ||
| 1 | 22 | 12 (42.58%) | 10 (45.45%) | ||
| 2 | 7 | 0 (0.00%) | 7 (31.81%) | 0.000 | 0.86 |
| 3 | 3 | 0 (0.00%) | 3 (13.63%) | ||
| 4 | 1 | 0 (0.00%) | 1 (4.54%) | ||
| Left Middle Lobe (LML) | |||||
| 0 | 6 | 5 (17.85%) | 0 (0.00%) | ||
| 1 | 15 | 15 (53.57%) | 0 (0.00%) | ||
| 2 | 13 | 7 (25.00%) | 6 (27.27%) | 0.000 | 0.73 |
| 3 | 11 | 0 (0.00%) | 11 (50.00%) | ||
| 4 | 5 | 0 (0.00%) | 5 (22.72%) | ||
| Left Lower Lobe (LLL) | |||||
| 0 | 6 | 5 (17.85%) | |||
| 1 | 9 | 8 (32.00%) | 1 (4.54%) | 0.000 | 0.8 |
| 2 | 9 | 9 (32.14%) | 0 (0.00%) | ||
| 3 | 15 | 4 (14.28%) | 11 (50.00%) | ||
| 4 | 11 | 1 (3.57%) | 10 (45.45%) | ||
| Right Upper Lobe (RUL) | |||||
| 0 | 7 | 5 (17.85%) | 2 (9.09%) | ||
| 1 | 20 | 14 (50.00%) | 5 (22.72%) | ||
| 2 | 13 | 7 (25.00%) | 6 (27.27%) | 0.017 | 0.66 |
| 3 | 3 | 0 (0.00%) | 3 (13.63%) | ||
| 4 | 7 | 1 (3.57%) | 6 (27.27%) | ||
| Right Middle Lobe (RML) | |||||
| 0 | 4 | 3 (10.71%) | 0 (0.00%) | ||
| 1 | 11 | 10 (53.71%) | 1 (4.54%) | ||
| 2 | 18 | 12 (42.85%) | 6 (27.27%) | 0.000 | 0.79 |
| 3 | 7 | 1 (3.57%) | 6 (27.27%) | ||
| 4 | 10 | 1 (3.57%) | 9 (40.90%) | ||
| Right Lower Lobe (RLL) | |||||
| 0 | 2 | 1 (3.57%) | 0 (0.00%) | ||
| 1 | 8 | 7 (25.00%) | 1 (4.54%) | ||
| 2 | 12 | 11 (39.28%) | 1 (4.54%) | 0.000 | 0.9 |
| 3 | 14 | 5 (17.85%) | 9 (40.90%) | ||
| 4 | 14 | 3 (10.71%) | 11 (50.00%) | ||
Table 3: Comparison of scores of each lung lobes between the two severity groups.
| Variables | Left lung | Right lung | P value | Upper Lobes | Middle Lobes | Lower Lobes | P value |
|---|---|---|---|---|---|---|---|
| Mild (n=28) | 2.96 | 4.64 | 0 | 1.61 | 2.5 | 3.5 | 0 |
| Severe (n=22) | 8 | 8.68 | 0 | 3.95 | 5.95 | 6.52 | 0 |
Table 4: Comparison of Left Lung Scores mean and Right Lung Scores mean, Upper Lobe Scores mean, Middle Lobes Scores mean and Lowe Lobe Scores mean (n=50).
Discussion
COVID-19 was declared as the sixth public health emergency pandemic requiring international concern by the World Health Organization on January 30, 2020 [1]. COVID-19 is a highly contagious viral disease that has spread around the world [2]. In addition, if there are no initial abnormalities on the chest x-ray, it can lead to a significant number of false negatives [3]. Thin-section chest CT is more sensitive than chest radiography at detecting pathological changes in the pulmonary parenchyma early in the disease process [4]. As a result, during in the COVID-19 outbreak in China, chest CT has become a major diagnostic tool [3]. This study was aimed to characterize the patterns and severity of COVID-19 using high resolution computed tomography scan. A total of 50 patients who had Chest (HRCT) and confirmed positively with COVID-19 using RT-PCR were included in this study.
According to the findings of this study, males are more likely than females to be infected with COVID-19, whether in mild or severe cases. These findings are in line with recent research, which suggests that higher levels of ACE2 and TMPRSS2 in males, hormonal influences on the immunological response, and gender variations in behavior may all have a role in the greater severity and fatality of COVID-19 seen in men [5]. Older adults and persons with underlying medical conditions are at higher risk for severe COVID-19. Study showed that patients, who have age over 60 years, were more likely to be infected with COVID-19 than those under the age of 39. As a result, Centers for Disease Control and Prevention (CDC) states that older people are more likely to get very sick from COVID-19. Being seriously ill means that elderly people with COVID19 may need hospitalization, intensive care or a ventilator to help them breathe, or they may even die. The risk increases for people in their 50s and increases in their 60s, 70s, and 80s. People 85 and older are more likely to become seriously ill.
We also observed that cough, fever, hypoxia, and SOB were the most common clinical manifestations associated with COVID-19 infection, as many literatures state that common clinical symptoms of COVID-19 patients include fever, cough, dyspnea, and fatigue, which are similar to those of severe acute respiratory syndrome coronavirus (SARS-CoV) and Middle East respiratory syndrome coronavirus (MERS-CoV) [6-8,14].
Our patient had a prevalence of hypertension and diabetes of cases (18; 36%).These results are consistent with previous studies, which suggested that these findings may be related to the advanced age of the patients. The relationship between cardiovascular comorbidities and clinical severity and prognosis in hospitalized patients needs further investigation, as it will have a significant impact on patient care [9].
Imaging features
Typical manifestations of early COVID19 are patchy, round, segmented or segmented ground glass opacities with or without consolidation [10]. Lesions are multiple and distributed asymmetrically and are more common in the peripheral regions [11-13]. In this study, the imaging features were consistent with the previous literature reports [15-18] of viral pneumonia; Study found that COVID-19 distributed as Multi-lesions in (92%) cases, bilaterally and diffused in (77%, 81% respectively) within the lung fields, having patchy pattern in (84%) cases. ground glass opacity (GGOs) were the most common feature in this descriptive cross sectional study which found in (92%) cases. Consolidation have found in 20 (40%) cases. These findings in the same line with previous study which state the predominant imaging pattern was of a peripheral ground- glass opacification with occasional consolidation in the peripheries [19-21].
In correlation between (CT-SS) and the radiographic patterns, there was a significant difference (P< 0.05) according to uni-lateral, bilateral, localized, diffused and consolidation lesion in both mild and severe groups (0.003, 0,001, 0,005. respectively).
Using a semi-quantitative scoring approach (CT Chest Scoring), the lung was divided into six zones (upper, middle, and lower on both sides) by the level of the tracheal carina and the level of the inferior pulmonary veins bilaterally on cross sectional CT images [20]. Using this Likert scale, the reviewers assessed the amount of the targeted patterns and the total affected lung parenchyma for each lobe. When comparing mild and severe cases, we discovered that the CT-SS was higher in severe cases. There were highly significant differences (p < 0.05) within lung lobes scores among the two severity groups (using Fisher exact test).
When we compared the right lung score mean to the left lung score mean with the two severity groups using student’ t-test, there was a significant difference (P< 0.05) also the right lung was the most infected in both the mild and severe groups, with mean (4.46 ; 8.68, respectively), where left scores mean were (2.96; 8.00). Most of the COVID-19 lesions involved both lower lobes more than two lobes [21,22]. In comparison to the upper and middle lobes in both lungs, COVID-19 was most commonly involved in the lower lobes of both lungs. These findings are in line with previous research [19] which devised a semi-quantitative scoring method to count the amount of lung opacification involving 20 lung regions as a surrogate for COVID-19 burden and discovered that the CT-SS was higher in severe cases when there was more lung opacification and not consistent with their result, where they found there is insignificant differences between left and right lung scores.
Limitations
This study had various limitations. First, the relatively small sample size was inadequate to disclose further potential mechanism or to include other predictive factors for prognosis. The study’s retrospective design may have resulted in selection bias. Another important problem was that lab testing and patient outcomes were not available in the majority of cases. In addition, characteristics such as cavitation and pleural effusion required further investigation. To validate the findings, bigger multi-center cohorts with follow-up and comprehensive data are required.
Recommendations
Future studies should use the RT-PCR results as the standard reference in conjunction with the final CT diagnose in order to determine the specificity and sensitivity (accuracy) as predictors for measuring disease severity. Since the clinical characteristics of COVID-19 change with the duration of the infection, we recommend future researchers to carefully consider the duration of disease as a fundamental factor in their studies.
Acknowledgment
Our deepest gratitude to our supervisor Dr. Saida Abdelkreem Omer Mohamed for her encouragement, guidance and to our cosupervisor Dr. Salma Ibnomer Dayelnaiem Mohamed for her great support helped us in this research.
Our warmth gratitude and thanks to Diagnostic Radiology- Department staff in Sudan University of Sciences and Technology, College of Medical Radiological Science and to Jabra Isolation Center who facilitated to getting the sample of this work. We wish to thank our radiologists Dr. Abdulrahman Hassan and Dr. Salah Alshoibi for analyzing the images and constructive criticisms.
References
- Zhu N, Zhang D, Wang W, Li X, Yang B, et al.(2020) A Novel Coronavirus from patients with pneumonia in China, 2019. N Engl J Med 382: 727-733.
- Li Q, Guan X, Wu P, Wang X, Zhou L, et al. (2020) Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N Engl J Med 382: 1199-1207.
- Chinese Society of Radiology (2020) Radiological Diagnosis of New Coronavirus Infected Pneumonitis: Expert Recommendation from the Chinese Society of Radiology (First edition). Chin J Radiol 54: E001-E001.
- Paul NS, Roberts H, Butany J, Chung T, Gold W, et al. (2004) Radiologic pattern of disease in patients with severe acute respiratory syndrome: the Toronto experience. Radiographics 24: 553-563.
- Mukherjee S, Pahan K (2021) Is COVID-19 gender-sensitive?. J Neuroimmune Pharmacol 16: 38-47.
- Assiri A, Al-Tawfi JA, Al-Rabeeah AA, Al-Rabiah, Al-Hajjar, et al. (2013) Epidemiological, demographic, and clinical characteristics of 47 cases of Middle East respiratory syndrome coronavirus disease from Saudi Arabia: a descriptive study. Lancet Infect Dis 13: 752-761.
- Lee N, Hui D, Wu A, Chan P, Cameron P, et al. (2003) A major outbreak of severe acute respiratory syndrome in Hong Kong. N Engl J Med 348: 1986-1994.
- Baj J, Karakuła-Juchnowicz H, Teresiński G, Buszewicz G, Ciesielka M, et al. (2020) COVID-19: Specific and Non-Specific Clinical Manifestations and Symptoms: The Current State of Knowledge. J Clin Med 9: 1753.
- Li S, Liu S, Wang B, Li Q, Zhang H, Zeng L, Ge H, Ma Q, Shen N. (2021) Predictive value of chest CT scoring in COVID-19 patients in Wuhan, China: a retrospective cohort study. Respir Med 176: 106271.
- Ng MY, Lee EYP, Yang J, Yang F, Li X, et al. (2020) Imaging profie of the COVID-19 infection: radiologic fidings and literature review. Radiol Cardiothorac Imaging 2: e200034.
- Lei J, Li J, Li X, Qi X (2020) CT Imaging of the 2019 Novel Coronavirus (2019- nCoV) Pneumonia. Radiology 295: 18.
- Liu P, Tan XZ (2019) Novel Coronavirus (2019-nCoV) Pneumonia. Radiology 295: 19.
- Chung M, Bernheim A, Mei X, Zhang N, Huang M, et al. (2020) CT imaging features of 2019 Novel Coronavirus (2019-nCoV). Radiology 295: 202-207.
- Saleemi S, Alhajji M, Almaghrabi R, Alrabiah F, Albaiz F, et al. (2020) Clinical characteristics of patients with COVID-19 in Saudi Arabia- A single center experience. Res Rev Infect Dis 3: 68-74.
- Ng MY, Lee EYP, Yang J, Yang F, Li X, et al. Imaging profile of the COVID-19 infection: radiologic findings and literature review. Radiol Cardiothoracic Imaging 2: e200034.
- Kim EA, Lee KS, Primack SL, Yoon HK, Byun HS, et al. (2002) Viral pneumonias in adults: radiologic and pathologic findings. Radiographics 22: S137-S149.
- Yang R, Li X, Liu H, Zhen Y, Zhang X, et al. (2020) Chest CT severity score: an imaging tool for assessing severe COVID-19. Radiol Cardiothorac Imaging 2: e200047.
- Li K, Fang Y, Li W, Pan C, Qin P, et al. (2020) CT image visual quantitative evaluation and clinical classification of coronavirus disease (COVID-19). Eur Radiol 30: 4407-4416.
- Haseli S, Khalili N, Bakhshayeshkaram M, Taheri MS, Moharramzad Y (2020) Lobar Distribution of COVID-19 Pneumonia Based on Chest Computed Tomography Findings; A Retrospective Study. Arch Acad Emerg Med 8: e55.
- Gold JAW, Wong KK, Szablewski CM, Patel PR, Rossow J, et al. (2020) Characteristics and clinical outcomes of adult patients hospitalized with COVID-19 Georgia, March 2020. MMWR Morb Mortal Wkly Rep 69: 545-550.
- https://www.cdc.gov/aging/covid19/
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Hussein AAA, Abdalkreem S, Adam A, Khalifa M, Abdallah A, et al. (2022) Patterns and Severity of COVID-19 among Sudanese Patients Using High Resolution Computed Tomography at Jabra Isolation Center. OMICS J Radiol 11: 391. DOI: 10.4172/2167-7964.1000391
Copyright: © 2022 Hussein AAA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 3917
- [From(publication date): 0-2022 - Dec 18, 2025]
- Breakdown by view type
- HTML page views: 3372
- PDF downloads: 545