Pediatric Gastro-Intestinal Endoscopy in Nigeria: A Budding Practice
Received: 03-Mar-2019 / Accepted Date: 15-Apr-2019 / Published Date: 25-Apr-2019 DOI: 10.4172/2161-069X.1000595
Abstract
Background: The application of rigid and flexible telescopes in the diagnosis and treatment of pathologies related to gastrointestinal tract of pediatric patients has achieved global acceptance and is widely performed.
Aims: To highlight the usefulness of diagnostic and therapeutic pediatric Gastro-Intestinal (GI) endoscopy in a developing country setting.
Patients and methods: A cross-sectional study of pediatric cases undergoing diagnostic and therapeutic gastrointestinal endoscopy in two health facilities in Port Harcourt metropolis, Nigeria from February 2012 to February 2018. The variables studied were demographics, indications, type of procedure, outcome and challenges. Statistical analysis of data was done using IBM SPSS Statistics for Windows, version 20 Armonk, NY.
Results: A total of 20 GI endoscopies were performed in pediatric patients. The age range of these cases was from 15 months to 18 years; mean age of 10.1 ± 5.7 years. There were 10 males and 10 females. Thirteen diagnostic GI endoscopies were done, and the therapeutic GI procedures were: 4 foreign body retrieval; 1 percutaneous endoscopic gastrostomy PEG; and 2 injection sclerotherapies for GI bleeding. General anesthesia was used in all patients below 12 years of age.
Conclusion: The technology-based practice of endoscopic intervention in pediatric patients is useful, safe and feasible.
Keywords: Endoscopy; Gastro-intestinal tract; Pediatric
Introduction
Surgical subspecialties are continually witnessing novel therapies in both minimally invasive and open surgical techniques. They are often heralded with skepticism or great enthusiasm, but overtime find their appropriate level of acceptance in the surgical armamentarium. The important considerations in local acceptance are related to cost, feasibility and safety. The application of rigid and flexible telescopes in the diagnosis and treatment of pathologies related to gastrointestinal tract in pediatric patients has achieved global acceptance [1].
Globally, the pediatric surgery workforce varies in distribution with a shortage reported [2,3]. In low- and middle-income countries where 50% of the populations are children a major limitation to endoscopic surgery is the short fall in pediatric surgical workforce including pediatric endoscopic surgeons, anesthesiologists and nurses [4]. To date, gastro-intestinal endoscopy in the pediatric population has generally been performed by both non-pediatric endoscopists and pediatric endoscopists [5]. The practice is longstanding in adult population with skilled endoscopists compared to pediatric age group thus they often fill the gap in pediatric gastrointestinal endoscopy service as a pragmatic step [6].
This study highlights an adult endoscopist’s experience in bridging the gap of pediatric gastrointestinal endoscopy service in a developing country, Nigeria.
Patients and Methods
This was a cross-sectional observational study of patients referred with specific indications for gastro-intestinal endoscopy at 2 private health facilities in Port Harcourt metropolis in Niger delta region of Nigeria. The patients’ data were prospectively collected using Microsoft Excel software. The inclusion criteria included cases undergoing GI endoscopy aged 18 years and below. The exclusion criteria included: non-GI pediatric endoscopic interventions; pediatric cases of laparoscopy in the GI tract; all adult cases. The data collated were demographics, indications, type of procedure, outcome and challenges.
Equipment
The equipment used were Karl Storz flexible video gastroscopes 13821/13801 PKS, video-colonoscopes 13925 PKS, Telecam DXII camera control unit, Xenon 100 W light source and Insufflator device, HD Monitor and AIDA data capture device.
Patient preparation
All cases were evaluated during a pre-endoscopy clinic visit or just prior to procedure for emergency cases. An informed consent was obtained from parent/guardian. A fasting recommendation was restricted to clear fluids from not later than 2-4 hours before procedure for upper GI endoscopy. Prior to colonoscopy, there was dietary restriction and bowel cleansing using sodium picosulphate citrate (Picolax) in split dose at 0.25 sachet/ dose for 2 to 6-year old patients, 0.5 sachet /dose for 6-12 years and 1 sachet/dose for >12 year-old patients. This was started a day prior to colonoscopy.
Anesthesia
For patients below the age of 12 years, intravenous propofol or ketamine was administered by an attending anesthesiologist. Intravenous antibiotic was administered prior to interventional procedures like injection sclerotherapy and Percutaneous Endoscopic Gastrostomy (PEG). There was endotracheal intubation with deflation of cuff in upper GI endoscopy while intubating the upper oesophageal sphincter or during foreign body retrieval at the stage of withdrawal through this region. A peri-procedural monitoring of oxygen saturation and vital signs of patients was done. For patients above 12 years of age and cooperative, there was an intravenous administration of a sedative (diazepam 0.1 ml/kg) by assistant physician with the assistance of trained endoscopy nurses. Also, a local anesthetic was sprayed on the pharyngeal mucosa for upper GI endoscopy and an opioid analgesic additionally administered for lower GI endoscopy. In all cases below 12 years or case of a non-cooperative child over 12 years of age, general anesthesia was the choice modality. Patients were monitored to full recovery and discharged home, same day, with instructions on subsequent visit to clinic or referred back to managing physician.
Statistical analysis
The statistical analysis of data was done using IBM SPSS Statistics for Windows, version 20 Armonk, NY. The mean and standard deviation of age was calculated, and categorical data described in simple percentages.
Results
A total of 20 GI endoscopy cases were performed on pediatric patients by same surgeon endoscopist during the study period. The age range was from 15 months to 18 years; mean age of 10.1 ± 5.7 years. There were 10 males and 10 females. The age and sex distribution are as shown in Table 1. Adolescents formed more than half of study population with no neonate recorded.
| Age | Male (%) | Female (%) | Total (%) |
|---|---|---|---|
| <2 years | 1 (5%) | 1 (5%) | 2 (10%) |
| 2-5 years | 3 (15%) | 1 (5%) | 4 (20%) |
| 6-12 years | 2 (10%) | 1 ( (5%) | 3 (15%) |
| 13-18 years | 4 (20%) | 7 (35%) | 11 (55%) |
| Total | 10 (50%) | 10 (50%) | 20 (100%) |
Table 1: Age and sex distribution of pediatric cases.
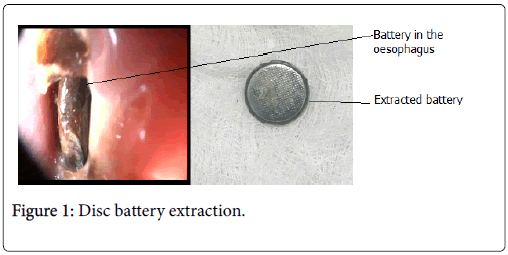
Upper gastrointestinal endoscopy
Seventeen cases of upper GI endoscopy were performed. The indications were: GI bleeding 5 (29.4%), upper abdominal pain 5 (29.4%), foreign body ingestion 4 (23.5%), dysphagia 1 (5-9%), vomiting of hair 1 (5.9%) and neurologic impairment 1 (5.9%). The therapeutic interventions recorded were: 4 foreign body retrieval (2- disc batteries, 1 British coin and 1 toothbrush); 1 percutaneous endoscopic gastrostomy for nutritional challenges in neurologic impairment (cerebral palsy); and 1 injection sclerotherapy for oesophageal varices. An Alligator grasping forceps was successfully used to endoscopically extract the coin and a disc battery (Figure 1) while a snare was used for the tooth brush retrieval. The sedation/ analgesia protocol for the procedures is as shown in Table 2.
| Procedures/indications | Conscious sedation | General anesthesia | Total Frequency |
|---|---|---|---|
| Upper GI Endoscopy | |||
| • Diagnostic | 7* | 5 | 12 |
| • Therapeutic | 0 | 5 | 5 |
| Lower GI Endoscopy | |||
| • Diagnostic | 2 | 0 | 2 |
| • Therapeutic | 1 | 0 | 1 |
| Total | 10 | 10 | 20 |
*Including local pharyngeal spray with 10% xylocaine spray
Table 2: Pediatric gastrointestinal endoscopies, indications and sedation/analgesia used.
Lower gastrointestinal endoscopy
An indication of bleeding per rectum was recorded in the three cases. Two colonoscopies were performed with no abnormality detected. There was a case of proctoscopy and a therapeutic injection sclerotherapy, using 50% dextrose as a sclerosant, was performed in this case of first degree hemorrhoids.
Outcome and Challenges
All cases were successfully completed endoscopically but for first case of disc battery due to non-availability of appropriate endoscopy accessories. There was no anesthetic complication recorded; however, dissociative side effects were observed with ketamine.
Transient sore throat and abdominal discomfort were the minor complications recorded in the upper and lower GI procedures respectively. There was no perforation or mortality recorded. All cases except PEG tube insertion were managed on out-patient basis. The cost of pediatric GI service in children below 12 years was higher than routine GI endoscopy in adult patients.
Discussion
There has been an evolution of pediatric gastrointestinal endoscopy in the last three decades with an increasing number of diagnostic and therapeutic applications [5]. In this study there was a 3.3:1 ratio of diagnostic to therapeutic pediatric cases performed with pediatric GI endoscopy representing 2.2% of entire GI endoscopies performed by endoscopist. This low rate of pediatric endoscopy is like a report from South-west Nigeria-1.9% [7]. There is paucity of literature on this service in Nigeria. This underscores the budding nature of this service hence a need for increased awareness and appropriate referral by pediatric care givers. Gastro-intestinal bleeding was the most common indication for both upper and lower GI endoscopy recorded with 7 (35.0%) cases and a sole case of normal study at colonoscopy. This is like another African study from Sudan; however, with a higher rate (49%) of normal study [8]. Abdominal pain and foreign body ingestion were the other leading indications.
The role of therapeutic intervention in the pediatric upper gastrointestinal tract can be divided broadly into diagnostic or therapeutic. This can be performed in an elective or emergency setting. Foreign body ingestion and GI bleeding were the emergency scenarios recorded which is in line with global trend of pediatric GI endoscopy [9]. The most frequently ingested foreign body recorded was disc battery (Figure 1). These small batteries have the risk of conducting electricity as both poles are in direct contact with the mucosa and leakage of caustic material. These can cause significant necrosis and potential perforation however none of these complications was recorded due to timely intervention. The types of foreign objects ingested by children vary with geography. In the western world, coins are the most frequently encountered foreign body, while in the eastern world, fish bones account for a greater percentage [10,11]. Other objects ingested such as magnets, toy parts or safety pins can add a degree of complexity and risk to foreign body retrieval. A case of impacted tooth brush, accidentally slipped down the hyperextended neck while brushing the teeth, was successfully retrieved by applying a snare to the handle in the distal esophagus and carefully extracted.
GI bleeding is a major indication for emergency pediatric endoscopy. A sole case of varices in the distal esophagus presenting as upper GI bleeding had first session of sclerotherapy and was subsequently lost to follow-up. The use of injection sclerotherapy is effective in treatment of esophageal and gastric varices [12,13]. Although band ligation is more efficacious in the adult population, the benefit of sclerosing agents in children is that they can be used in scenarios where band ligators are too large to pass through the oropharynx of a young child [9]. Injection sclerotherapy using 50% dextrose was successful in a case of first degree hemorrhoids as is reported in literature [14]. In all, surgical intervention is needed in failed endoscopic intervention for profuse bleeding as interventional radiology is another service not readily available. A case of profuse duodenal bleeding required an open surgery which revealed an ulcerated choledochocele. A duodenotomy with marsupialization of cyst was performed during the operation.
A major challenge to pediatric GI endoscopy is anesthesia with the attendant risk and additional cost implication. In contrast to adult GI endoscopy generally performed under conscious sedation, the same in children is mostly performed under deep sedation or general anesthesia. This is to reduce emotional stress of separation from parents and preparation for the procedure. A pre-procedural assessment including a systematic review and physical examination with a special focus on the airway with a documentation of loose teeth and oral piercings is important [14]. Ketamine and propofol were the anesthetic agents used in this study. The use of the former drug elicited dissociative effect; beyond this no untoward effect was recorded.
A need for special equipment is yet another challenge in paediatric GI endoscopy. Endoscopes for paediatric cases are chosen based on age and weight of the patient. For children weighing between 2.5-10 kg, gastroscope of diameter ≤ 6 mm is preferred [13]. There was however no child recorded in this age group. The standard gastroscopy with 9 mm diameter is considered, particularly if therapeutic intervention is needed because of the large channel size to admit endoscopy accessories- as was used in this study. Lastly, there was the challenge of non-ready, local availability of endoscopy accessories leading to a failed attempt at foreign body retrieval. This hurdle was overcome by out-sourcing and stocking of relevant endoscopy consumables. Despite these challenges, patients were managed primarily on ambulatory care (out-patient) basis with timely intervention and a reduction in duration of anxiety to parents and early return to school.
Conclusion
There are peculiar surmountable challenges to the budding practice of pediatric GI endoscopy in Nigeria. The technology-based practice of endoscopic intervention in pediatric patients is useful, safe and feasible.
Conflicts of Interest
Conflict of interest disclosed was none.
References
- Wilson CB (2006) Adoption of new surgical technology. BMJ 332: 112-114.
- Ameh EA, Adejuyigbe O, Nmadu PT (2006) Paediatric Surgery in Nigeria. J Paediatr Surg 41: 542-546.
- Nakayama DK, Burd RS, Newman KD (2009) Paediatric surgery workforce: Supply and demand. J Paediatr Surg 44: 1677-1682.
- Krishnaswami S, Nwomeh B, Ameh E (2016) The paediatric surgery workforce in low-middle income countries: problems and priorities. Semin Paediatr Surg 25: 32-42.
- Thomson M, Tringali A, Dumonceau JM, Tavares M, Tabbers MM, et al. (2017) Paediatric gastrointestinal endoscopy: European society for paediatric gastroenterology hepatology and nutrition and European society of gastrointestinal endoscopy guidelines. J Pediatr Gastroenterol Nutr 64: 133-153.
- Rawashdeh MD, Abu-Farsakh N, al-Jaberi TM (1996) Paediatric upper gastrointestinal endoscopy in developing countries. Ann Trop Paediatr 16: 341-346.
- Alatise OI, Anyabolu HC, Sowande O, Akinola D (2015) Paediatric endoscopy by adult gastroenterologists in Ile-Ife Nigeria. A viable option to increase the access to paediatric endoscopy in low resource countries. Afr J Paediatr Surg 12: 261-265.
- Mudawi HMY, El Tahir MA, Suleiman HS, Eltaybe NH, Gamer NM, et al. (2009) Paediatric gastrointestinal endoscopy: experience in a Sudanese University Hospital. East Mediterr Health J 15: 1027-1031.
- Rahman I, Patel P, Boger P, Rasheed S, Thomson M, et al. (2015) Therapeutic upper gastrointestinal tract endoscopy in Paediatric Gastroenterology. World J Gastrointest Endosc 7: 169-182.
- Cheng W, Tam PK (1999) Foreign-body ingestion in children: experience with 1,265 cases. J Pediatr Surg 34: 1472-1476.
- Kay M, Wyllie R (2005) Pediatric foreign bodies and their management. Curr Gastroenterol Rep. 7: 212-218.
- Hill ID, Bowie MD (1991) Endoscopic sclerotherapy for control of bleeding varices in children. Am J Gastroenterol 86: 472-476.
- Ray-Offor E, Amadi S (2019) Haemorrhoidal disease: predilection sites, pattern of presentation, and treatment. Ann Afr Med 18: 12-16.
- Friedt M, Welch S (2013) An update on pediatric endoscopy. Eur J Med Res 18: 24.
Citation: Ray-Offor E, Gbobo I (2019) Pediatric Gastro-Intestinal Endoscopy in Nigeria: A Budding Practice. J Gastrointest Dig Syst 9: 596. DOI: 10.4172/2161-069X.1000595
Copyright: © 2019 Ray-Offor E, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4063
- [From(publication date): 0-2019 - Dec 06, 2025]
- Breakdown by view type
- HTML page views: 3160
- PDF downloads: 903