Percutaneous Repair of Achilles Tendon Rupture
DOI: 10.4172/2329-910X.1000314
Introduction
The treatment modalities for Achilles tendon rupture vary from conservative to different surgical treatment options. The main concerns of conservative treatment are the complications of long term immobilization and re-rupture rate, which could be minimized by advances in postoperative rehabilitation programs and functional bracing. On the contrary, the main concern of open repair is wound complications, which could be minimized by recent advances in minimally invasive techniques. Percutaneous repair of acute tendoachilles rupture avoids possible complications of open repair as well as conservative treatment [1]. This paper presents a series of patients with acute tendon rupture treated with percutaneous repair carried. The purpose of this study is to evaluate the clinical and functional results of percutaneous repair of acute Achilles tendon ruptures and efficacy of this technique in sural nerve protection.
Patients and Methods
The study was approved by the ethical committee of Dpu University, Pune. A total of 22 patients with complete rupture of the Achilles tendon were treated in Dr. D. Y. Patil hospital and medical college pune, using the presented technique. All patients signed an informative consent form. There were 16 men and 6 women, with a mean age of 34.7 years (25 years-48 years). The causes of injury were sports activity (12 patients) twist injury (six), falling downstairs (two) and during daily activity (two).
Diagnosis
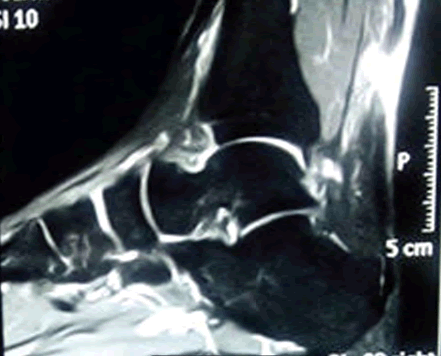
The rupture was diagnosed at the site of rupture a palpable tendon gap, positive Thompson test, positive matles test and loss of plantar flexion in the affected ankle and unable to walk on toes on the affected side (Figure 1). The diagnosis was confirmed by radiological evaluation (MRI/USG) for all patients (Figure 2). All patients had a complete rupture of the Achilles tendon with a gap less than 3 cm located 3 cm-6 cm proximal to the calcaneal insertion[2]. The inclusion criteria were complete rupture if Achilles tendon of not more than 1 month duration with intact skin and intact sensation of the affected limb. Exclusion criteria were as follows (a) incomplete rupture of Achilles tendon, (b) chronic rupture exceeding 1 month duration, (c) sensory impairment of the affected limb, (d) bony avulsion of calcaneal tuberosity, (e) history of recent local corticosteroid injection and (f) re-rupture of the Achilles’ tendon. The percutaneous tendon repair was done with in a mean of 8.5 days (2 days-28 days) of injury. The mean follow up was 26 months (18 months-40 months).
Operative technique
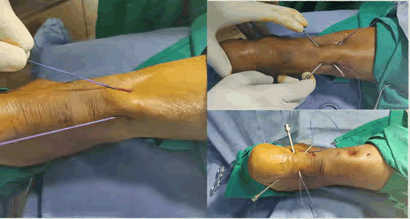
All patients underwent surgery under spinal anesthesia without tourniquet. Patients were placed in prone position with free ankle and foot for easily mobilization [3]. After detecting the site of rupture, skin incision markings were marked along the posterior aspect of the Achilles’ tendon. Leg and foot were prepared and draped.
Materials required
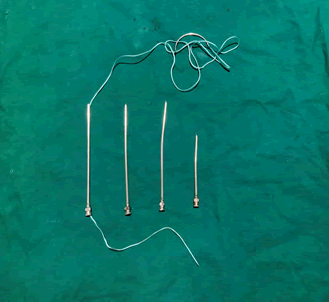
a. Needles 16G ss needless short and long b. Sutures ethibond (5-0), ethilon (3-0) (Figure 3)
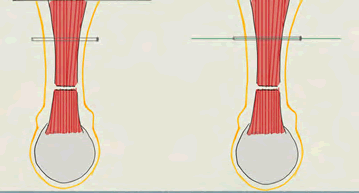
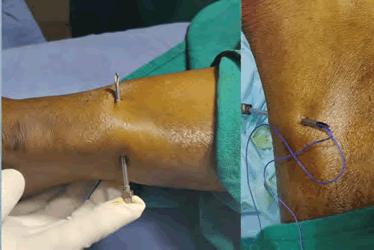
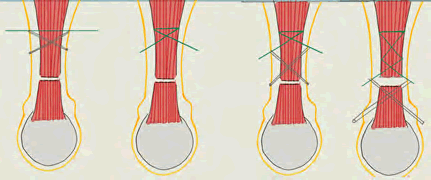
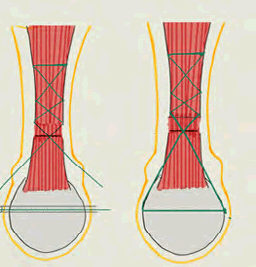
Over the posterior aspect of tendon, 4 cm-5 cm above the proximal ruptured end of tendon, a 16G needle is passed from medial to lateral through the tendon and ethibond is passed through the 16G needle. Then two 16G needles are passed obliquely inferior to superior through the tendon and ethibond is passed through the needles (Figures 4-6).
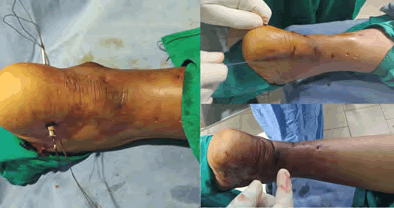
This similar technique is followed again till the proximal end of tendon is held firmly with ethibond. Then this similar technique is followed in the distal part of Ruptured tendon. Keep the ankle in plantar flexion till you get approximation of ruptured ends of tendon [4]. Keeping the ankle in plantar flexion, drill bit (2.7 mm) is passed through the calcaneum medial to lateral, and 16G needle is passed through the drill hole and lateral end of ethibond is passed through the needle (laterally to medially) so that both the free ends of ethibond are placed medially, free ends are tied and knot is buried underneath the skin, if necessary apply skin sutures. Hold the limb in plantar flexion and apply pop cast after aseptic dressing of wound, pop should be moulded along the course of tendoachilles (Figures 7-10).
Post-Operative care and follow up
Immobilization was done for two weeks in anterior below knee cast in plantar flexion for 6 weeks. After 6 weeks, gradual protected weight bearing, gradual increase in ankle range of motion, and calf strengthening and stretching exercise were initiated. Routine clinical follow up was performed at 2, 4 and 6 weeks. After 12 weeks patient is asked to resume full and normal daily activities. MRI was done at 3 months for all patients and the clinical follow up was completed at 6, 9, 12, 18 and 24 months.
Evaluation
American orthopedic foot and ankle society score (AOFAS) was used for functional evaluation (the ankle hind foot scale consists of nine items scored together for a total of 100 points, which are distributed over three categories: pain (40 points), functions (50 points) and alignment (10 points)). Thompson test, double heel rise test, and the single heel rise test were recorded. Patients return to work and complications were recorded.
Results
Across Average time of percutaneous repair of Achilles tendon rupture was 20 minutes (15-30 min). Period of hospitalization was 1-2 days. The mean follow up was 26 months (18-40) months. Functional outcomes were recorded at the 18 month post-operative visit for all 22 patients. The time interval from repair to return to work was 5-12 weeks, with a mean time of 7.54 weeks. The time interval from repair to return to sports was 16-28 weeks, with a mean time of 20 weeks.
Discussion
The variable anatomical course of sural nerve makes it vulnerable to injury during percutaneous suturing of recent Achilles tendon rupture [5,6]. The sural nerve during its course crosses the lateral Border of Achilles tendon at variable distances from tendon insertion. Distally the sural nerve passes lateral to Achilles’ tendon insertion. To overcome the possibility of sural nerve injury the lateral half of the Achilles tendon should be spared from percutaneous sutures. In our patients no tendon re-ruptures with adequate tendon healing at 3 months were observed. Deep venous thrombosis doesn’t occur in our series; this is due to early mobilization in anterior below knee slab and accelerated rehabilitation programs [7,8].
Conclusion
The presented percutaneous technique is easy and safe, with a low rate of complications. This technique preserves blood supply of the tendon (because Para tendon is not stripped), prevents infection and early healing of Achilles tendon. Thus this technique is very much helpful in diabetic patients. This technique avoids the possible complications of conservative and open management with neither re-rupture nor sural nerve injury, as the percutaneous sutures are avoided in this procedure.
References
- Ma GWC, Griffith TG (1977) Percutaneous repair of acute closed ruptured achilles tendon: A new technique. Clin Orthop 128: 247-255.Â
- Maes R, Copin G, Averous C (2006) Is percutaneous repair of the Achilles tendon a safe technique? A study of 124 cases. Acta Orthop Belg 72:179-183.              Â
- Ververidis AN, Kalifis KG, Touzopoulos P, Drosos GI, Tilkeridis KE, et al (2015) Percutaneous repair of the Achilles tendon rupture in athletic population. J Orthop 13:57-61.Â
- Soubeyrand M, Serra-Tosio G, Campagna R, Molina V, Sitbon P, et al (2010) Intraoperative ultrasonography during percutaneous achilles tendon repair. Foot Ankle Int 31:1069-1074.Â
- Fortis AP, Dimas A, Lamprakis AA (2008) Repair of achilles tendon rupture under endoscopic control. Arthroscopy 24:683-688. Â Â Â Â Â Â Â Â Â Â Â Â Â Â
- Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, et al (1994) Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int 15:349-353.Â
- Porter KJ, Robati S, Karia P, Portet M, Szarko M, et al (2014) An anatomical and cadaveric study examining the risk of sural nerve injury in percutaneous Achilles tendon repair using the Achillon device. Foot Ankle Surg 20:90-93.    Â
- Webb J, Moorjani N, Radford M (2000) Anatomy of the sural nerve and its relation to the Achilles tendon, Foot Ankle Int 21:475-477
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3608
- [From(publication date): 0-2021 - Dec 10, 2025]
- Breakdown by view type
- HTML page views: 2744
- PDF downloads: 864