Research Article Open Access
Perinatal Outcome in Patients with Isolated Oligohydramnios at Term: A Prospective Study
Enas Mushtaq*, Shameema Parveen, Feroze Shaheen, Sami Jan, Asif Abdullah and Yasir Ahmad LoneDepartment of Obstetrics and Gynaecology, SKIMS, Srinagar
- Corresponding Author:
- Enas Mushtaq
Department of Obstetrics and Gynaecology
SKIMS, India
Tel: 9419409779
E-mail: enasmushtaq123@gmail.com
Received date: May 15, 2017; Accepted date: May 31, 2017; Published date: June 04, 2017
Citation: Mushtaq E, Parveen S, Shaheen F, Jan S, Abdullah A, et al. (2017) Perinatal Outcome in Patients with Isolated Oligohydramnios at Term: A Prospective Study. J Preg Child Health 4:332. doi:10.4172/2376-127X.1000332
Copyright: © 2017 Mushtaq E, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Pregnancy and Child Health
Abstract
Objective: To evaluate the perinatal outcome in patients with isolated oligohydramnios. Design: A prospective study. Sample: 146 patients had isolated oligohydramnios. These were compared with those having AFI>5 cm (n=500). Methods: A prospective study was conducted from November 2012 to November 2014. Patients were divided into two groups (AFI>50 mm and ≤ 50 mm). The study inclusion criteria were women with singleton pregnancy at 36-42 weeks gestational age (GA) and women sure of the gestational age. Main outcome measures: Abnormal non-stress test, obstetric intervention for fetal distress, Apgar score, meconium stained liquor and NICU admission. Results: The two groups were similar with regard to maternal age, parity and mean gestational age. Isolated oligohydramnios was associated with higher rate of induction of labour (68.49% vs. 21.8%, p<0.001), nonreassuring fetal heart rate (45.20% vs. 13.2%, p<0.001), cesarean section for fetal distress (51.61% vs. 28.47%, p<0.001), meconium stained amniotic fluid (32.2% vs. 21.6%, p=0.008). However, there was no statistically significant difference between the two groups in terms of Apgar score at 1 min, NICU admissions and stillbirths. Conclusion: Isolated oligohydramnios is associated with increased risk of obstetric interventions particularly due to fetal distress. Nonetheless, fetal distress due to oligohydramnios did not lead to increased risk for low Apgar, NICU admissions, stillbirths. This may be reflective of aggressive intrapartum management that these patients received.
Keywords
Oligohydramnios; Amniotic fluid index (AFI); Perinatal
Introduction
Amniotic fluid (AF) is a marvellously complex and dynamic milieu that changes as pregnancy progresses [1].
The AFV can be measured by dye dilution techniques at the time of amniocentesis [2,3] or can be directly measured at caesarean delivery [4]. The dye-dilution test is the gold standard for the assessment of amniotic fluid volume [2,4]. Since this modality is invasive and associated with higher complications, especially in the presence of decreased amniotic fluid volumes, it is more feasible to estimate AFV by sonography in routine clinical practice.
There are 3 reported sonographic techniques used to estimate the AFV:
1) Maximal vertical pocket: Chamberlain defined the normal amount of amniotic fluid as the largest/deepest vertical fluid pocket measuring between 2 and 8 cm [5].
2) Amniotic fluid index (AFI): Phelan proposed amniotic fluid index (AFI) as a more objective and reproducible method as it estimates the amniotic fluid in four quadrants, and defined oligohydramnios as AFI less than 5 cm, with the normal range for AFI being 12.9 ± 4.6 cm (5-18 cm) [6,7].
3) Two diameter pocket: Manning defined oligohydramnios when the largest pocket on ultrasound in both vertical and horizontal planes measure less than 2 cm [8]. Any change above or below the normal values for amniotic fluid volume has been associated with adverse perinatal morbidity and mortality. The exact definition of oligohydramnios varies according to the technique used for measuring amniotic fluid volume. Depending on the sonographic technique used to assess amniotic fluid volume, certain cut-off values for oligohdramnios have been defined as below:
1. Single vertical pocket: definitions range between <1.0 cm 5, <2 cm [9] and <3 cm [10].
2. Two-diameter pocket: vertical × horizontal <15 cm2
3. AFI (Amniotic Fluid Index) technique: definitions of oligohydramnios include <5 cm (which represents <1st centile) 6, <5th centile for gestational age (which translates into an AFI value of between 7.1 and 9.7cm) [11] and <8 cm [12].
The causes of oligohydramnios can be divided into fetal, maternal, uteroplacental and idiopathic. The results of pregnancies with isolated oligohydramnios are controversial. Some authors [5,13,14] associate isolated oligohydramnios with an increased risk of adverse perinatal result. But others [15-17] have not shown any association of worse perinatal outcome with oligohydramnios. The objective of this study is to determine the association of isolated oligohydramnios at term with adverse perinatal outcome..
Methods
The study was conducted in the Department of Obstetrics and Gynaecology, Sher-i-Kashmir Institute of Medical Sciences (SKIMS), Srinagar. It was a prospective study conducted over a period of 2 years from November 2012 to November 2014. During this study, patients with singleton pregnancy were selected and Amniotic Fluid Index (AFI) was evaluated with the technique of Phelan. On the basis of AFI measurements, patients were divided in two groups. Those who had AFI>50 mm and ≤ 50 mm. The study inclusion criteria were as follows: Women with singleton pregnancy at 37-42 weeks gestational age (GA) and those sure of the gestational age.
The study exclusion criteria were as follows:
Patients with less than 37 weeks and unsure gestational age, those with multiple pregnancies, history of premature rupture of membranes, diabetes mellitus, hypertension, preeclampsia, those with fetal growth restriction and/or congenital fetal anomaly [18-20].
The variables selected to evaluate results included: spontaneous vaginal delivery, abnormal non-stress test, obstetric intervention for fetal distress, 1 min Apgar score <7, 5 min Apgar score <7, presence of meconium, birth weight, and neonatal intensive care unit (NICU) admission.
Statistical Methods
The perinatal outcome of the study group was compared with that of the control group. The results were collected, evaluated and statistically analysed. The continuous variables of the study have been shown in terms of mean ± S.D. The categorical variables of the study have been shown in terms of frequency and percentage. The two groups of interest have been compared statistically with the help of standard statistical tests like independent t-test, chi-square test and Fisher exact test. All the results so obtained have been discussed as 5% level of significance, i.e., P-value less than 0.05 considered as significant.
Results
During the study period, there were 146 patients who had isolated oligohydramnios (AFI ≤ 5 cm), which formed the study group. These were compared with those having AFI>5 cm and with no other associated complication. This group included 500 patients, which formed the control group.
The perinatal outcome of the study group was compared with that of the control group. The results were collected, evaluated and statistically analysed.
The mean age for the study group was 29.10 ± 3.081 years and for the control group was 29.34 ± 1.966 years. Maximum number of patients were in the age group of 26-30 years in both the study and control group. 58.2% of the patients in the study group and 60.4% of the patients in the control group were primigravida. The two groups were comparable (p=0.610). The mean gestational age in the study group was 39.02 ± 0.936 weeks and in the control group was 39.19 ± 1.100 weeks (p=0.069).
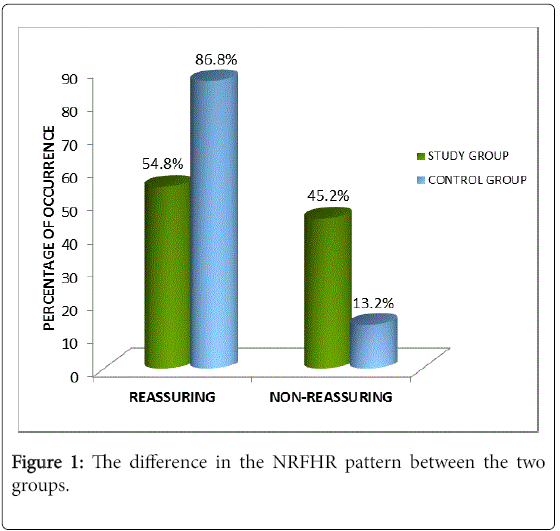
45.2% of the patients in the study group had NRFHR pattern as compared to 13.2% in the control group. The difference in the NRFHR pattern between the two groups was statistically significant (p<0.001). 68.49% of the patients in the study group were induced, while only 21.8% of the patients in the control group were induced (p<0.001) (Figure 1).
Cesarean delivery was done in 93 (63.69%) patients in the study group, while as 144 (28.8%) patients in the control group underwent Cesarean section (p<0.001). Out of these, 51.61% of Cesarean section done in the study group was for fetal distress as compared to 28.47% in the control group (Tables 1 and 2). So, there were significantly more number of Cesarean section done for fetal distress in the study as compared to control group (p<0.001). 32.2% of patients in the study group and 21.6% in the control group had meconium stained amniotic fluid. 15.1% of the patients in the study group had thin meconium stained amniotic fluid in comparison with 8.4% in the control group.
| Indication | Study group | Control group | ||
|---|---|---|---|---|
| ( n = 93 ) | ( n = 144) | |||
| Number | Percentage | Number | Percentage | |
| Fetal distress | 48 | 51.61% | 41 | 28.47% |
| CPD | 15 | 16.12% | 27 | 18.75% |
| Failure of induction | 8 | 8.60% | 12 | 8.33% |
| Failure to progress | 9 | 9.67% | 22 | 15.27% |
| Previous 2 lscs | 6 | 6.45% | 19 | 13.19% |
| Malpresentation | 7 | 7.52% | 19 | 13.19% |
| Bad obstetric history | 0 | 0% | 4 | 2.77% |
Table 1: Caesarean delivery was done in 93 (63.69 %) patients in the study group.
| Indication | Study group | Control group | P-Value | Odds ratio |
|---|---|---|---|---|
| For lscs | (n=93) | (n=144) | ( 95 % C.I.) | |
| Fetal distress | 48 | 41 | < 0.001 | 2.67 |
| -51.61% | -28.47% | (1.49 âÂ?Â? 4.78 ) | ||
| Other reasons | 4500.00% | 103 | ||
| -48.38% | -71.52% |
Table 2: Caesarean section done in the study group.
Thick meconium stained amniotic fluid was present in 17.1% of the patients in the study group and in 13.2% in the control group (p=0.008). Maximum number of babies (107 out of 146, 73.28%) in the study group had birth weight between 2.5-3.5 kg while as in the control group maximum (382 out of 500, 76.4%) had birth weight between 3-4 kg. The mean birth weight in the study group was 3.0048 ± 0.456 kg and in the control group was 3.1800 ± 0.393 kg. There was a statistically significant difference between the two groups in terms of mean birth weight (p=0.000). 9.59% of the babies in the study group had Apgar score <7 at 1 min while as 8.4% of the babies in the control group had Apgar score <7 at 1 min. 3 babies (2.05%) and 5 babies (1%) had Apgar score <7 at 5 min after birth in the study and control group, respectively. Although more number of babies in the study group had Apgar score <7 at 1 min and 5 min as compared to the control group, the difference did not reach statistical significance (p=0.311). 7.6% of the babies in the study group required NICU admission as compared to 6% in the control group. The difference, again was not statistically significant (p=0.562). There was 1 still birth in the study group (0.68%). That baby had two tight turns of cord around neck and a true knot. On the contrary, there was no stillbirth in the control group. There was no early neonatal death in either the study or the control group.
Discussion
Oligohydramnios can be isolated or associated with maternal or fetal conditions such as hypertension, premature rupture of membranes, fetal growth restriction and congenital anomalies. While perinatal outcomes of associated oligohydramnios are related to the underlying condition, the natural history of isolated oligohydramnios is unclear.
Main findings
In the present study, it was seen that 45.20% of the patients in the study group had NRFHR pattern as compared to 13.2% in the control group. Thus, there was a higher incidence of NRFHR in the study as compared to the control group and the difference reached the statistical significance (p<0.001). All the patients with AFI ≤ 5 cm at term were admitted to the hospital. Out of 146 patients with oligohydramnios, in 100 patients (68.49%) labour was induced. This is in contrast to 109 patients (21.8%) that were induced in the control group. Significantly, more number of labour inductions were done in the study group as compared to the control group (p<0.001). 93 out of 146 patients (63.69%) in the study group underwent Cesarean section, while as in 144 out of 500 patients (28.8%) in the control group Cesarean section was done. The difference between the two groups in terms of cesarean delivery was statistically significant (p<0.001). Out of these, 48 patients had cesarean section done for fetal distress (51.61%) in the study group as compared to 41 patients (28.47 %) in the control group. In the present study, 32.2% had meconium stained amniotic fluid in the study group whileas 21.6% of patients in the control group had meconium stained amniotic fluid. The result was statistically significant in our study (p=0.008).
14 babies out of 146 (9.59%) had Apgar score <7 at 1 min while as in the control group 42 babies out of 500 (8.4%) had Apgar score <7 at 1 min. Although the percentage of low Apgar score was higher in the study as compared to the controls, the result was not statistically significant (p=0.653). 3 babies (2.05%) in the study group and 5 babies (1%) in the control group had Apgar score <7 at 5 min. This result again was not statistically significant (p=0.311). 11 out of 146 (7.6%) babies in the study group were admitted in NICU in comparison with 30 out of 500 (6%) babies in the control group. The difference was not statistically significant (p=0.562). There was 1 (0.68%) still birth in the study group as compared to none in the control group. There was no early neonatal death in either group.
Interpretation
The results have been comparable with other studies. In the study done by Elsandabesee et al. [18] demonstrating the “Obstetricians’ attitudes towards ‘isolated’ oligohydramnios at term” , they found that in 45% of the patients with isolated oligohydramnios, induction of labour was done as compared to 25% in the normal liquor group. In the study done by Ashwal et al. [19], induction of labour was done in 27.7% in the study group and 3.7% in the control group (p<0.001). These studies show that oligohydramnios is an independent indication for induction of labour in most studies.
In the other studies also, caesarean section rate was higher in the oligohydramnios group as compared to the control group. In the meta analysis done by Rossi and Prefumo [20], it was found that obstetric interventions occurred more frequently in the isolated oligohydramnios (IO) than normal amniotic fluid (AF) group (IO: 89/679, 13% vs. normal AF: 166/3354, 5%; OR: 2.30; 95% CI: 1.00-5.29). Similarly, the rate of LSCS was noted to be significantly higher in the study compared to control group by Locatelli [21]. (p=0.045) and Ashwal [19] (p<0.001).
Controversies exist with regard to the relationship between oligohydramnios and meconium-stained amniotic fluid. In concordance to our findings, Rainford et al. [22] found higher rate of meconium stained amniotic fluid in oligohydramnios group as compared to control group (35% vs. 16%), (p=0.01). However, in the meta-analysis done by Rossi and Prefumo [20], meconium stained amniotic fluid was equally present in the study (86/657; 13.1%) and control groups (387/3216; 12.0%). Similarly, Ashwal et al. [19], Locatelli et al. [21] did not find significant difference between the two groups with regard to meconium stained amniotic fluid with p=0.67 and 0.98, respectively.
Similar results were found in the other related studies in terms of Apgar score at birth, NICU admissions, stillbirths and early neonatal deaths. In the study done by Ashwal et al. [19], Rossi and Prefumo [20] and Locatelli et al. [21] the difference in terms of Apgar score at birth did not reach statistical significance. Again, there was no statistically significant difference between the two groups in terms of NICU admission (Table 3) in the study done by Conway et al. [15], Rossi and Prefumo [20] and Ashwal et al. [19].
| Study | Afi = 5 cm | Â afi>5 cm | P-value |
|---|---|---|---|
| Conway et al [27] | 16.40% | 11.50% | Ns |
| Rossi et al [68] | 2.40% | 5.70% | Ns |
| Ashwal et al [73] | 4.60% | 3.60% | 11.00% |
| Present study | 7.60% | 6.00% | 56.20% |
Table 3: Significant difference between the two groups in terms of NICU admission.
Conclusion
This study shows that isolated oligohydramnios in uncomplicated term pregnancy is associated with significantly higher number of patients with non-reassuring fetal heart rate, induction of labour, caesarean delivery for fetal distress, meconium stained amniotic fluid.
Nonetheless, fetal distress due to oligohydramnios did not lead to increased risk for low Apgar score at birth, NICU admissions, still births, neonatal deaths.
It might be argued that the perinatal outcome was not significantly different between the two groups because all the patients with oligohydramnios were strictly monitored and interventions were undertaken at the earliest sign of possible fetal distress.
Ethical Considerations
Approved by the institutional ethics committee (Sher-I-Kashmir Institute of medical Sciences – SKIMS – institutional ethical committee- December 2012).
References
- Underwood MA, Gilbert WM, Sherman MP (2005) Amniotic fluid: Not just fetal urine anymore. J Perinatol 25: 341-348.
- Magann EF, Nolan TE, Hess LW, Martin RW, Whitworth NS, et al. (1992) Measurement of amniotic fluid volume: Accuracy of ultrasonography techniques. Am J Obstet Gynecol 167: 1533-1537.
- Dildy GA III, Lira N, Moise KJ, Riddle GD, Deter RL (1992) Amniotic fluid volume assessment: Comparison of ultrasonographic estimates versus direct measurements with a dye-dilution technique in human pregnancy. Am J Obstet Gynecol 167: 986-994.
- Horsager R, Nathan L, Leveno KJ (1994) Correlation of measured amniotic fluid volume and sonographic predictions of oligohydramnios. Obstet Gynecol 83: 955-958.
- Chamberlain PF, Manning FA, Morrison I, Harman CR, Lange IR (1984) Ultrasound evaluation of amniotic fluid volume, I: the relationship of marginal and decreased amniotic fluid volumes to perinatal outcome. Am J Obstet Gynecol 150: 245-249.
- Phelan JP, Smith CV, Broussard P, Small M (1987) Amniotic fluid volume assessment with the four-quadrant technique at 36-42 weeks gestation. J Reprod Med 32: 540-542.
- Rutherford SE, Phelan JP, Smith CV, Jacobs N (1997) The four-quadrant assessment of amniotic fluid volume: An adjunct to antepartum fetal heart rate testing. Obstet Gynecol 70: 353-356.
- Chauhan SP, Magann EF, Perry KG, Morrison JC (1997) Intrapartum amniotic fluid index and two-diameter pocket are poor predictors of adverse neonatal outcome. J Perinatol 17: 221-224.
- Manning FA, Harman CR, Morrison I, Menticoglou SM, Lange IR, et al. (1990) Fetal assessment based on fetal biophysical profile scoring. IV. An analysis of perinatal morbidity and mortality. Am J Obstet Gynecol 162: 703-709.
- Halperin ME, Fong KW, Zalev AH, Goldsmith CH (1985) Reliability of amniotic fluid volume estimation from ultrasonograms: Intraobserver and interobserver variation before and after the establishment of criteria. Am J Obstet Gynecol 153: 264–7.
- Moore TR, Cayle JE (1990) The amniotic fluid index in normal human pregnancy. Am J Obstet Gynecol 162: 1168-1173.
- Jeng CJ, Lee JF, Wang KG, Yang YC, Lan CC (1992) Decreased amniotic fluid index in term pregnancy: Clinical significance. J Reprod Med 37: 789-792.
- Banks EH, Miller DA (1999) Perinatal risks associated with borderline amniotic fluid index. Am J Obstet Gynecol 180: 1461-1463.
- Casey BM, McIntire DD, Bloom SL, Lucas MJ, Santos R, et al. (2000) Pregnancy outcomes after antepartum diagnosis of oligohydramnios at or beyond 34 weeks' gestation. Am J Obstet Gynecol 182: 909-912.
- Conway DL, Adkins WB, Schroeder B, Langer O (1998) Isolated oligohydramnios in the term pregnancy: Is it a clinical entity? J Matern Fetal Med 7: 197-200.
- Rainford M, Adair R, Scialli AR, Ghidini A, Spong CY (2001) Amniotic fluid index in the uncomplicated term pregnancy, prediction of outcome. J Reprod Med 46: 589-592.
- Zhang J, Troendle J, Meikle S, Klebanoff MA, Rayburn W, et al. (2004) Isolated oligohydramnios is not associated with adverse perinatal outcomes. BJOG 111: 220-225.
- Elsandabesee D, Majumdar S, Sinha S (2007) Obstetricians' attitudes towards 'isolated' oligohydramnios at term. J Obstet Gynaecol 27: 574-576.
- Ashwal E, Hiersch L, Melamed N, Aviram A, Wiznitzer A, et al. (2014) The association between isolated oligohydramnios at term and pregnancy outcome. Arch Gynecol Obstet 290: 875-881.
- Rossi AC, Prefumo F (2013) Perinatal outcomes of isolated oligohydramnios at term and post-term pregnancy: A systematic review of literature with meta-analysis. Eur J Obstet Gynecol Reprod Biol 169: 149-154.
- Locatelli A, Vergani P, Toso L, Verderio M, Pezzullo JC, et al. (2004) Perinatal outcome associated with oligohydramnios in uncomplicated term pregnancies. Arch Gynecol Obstet 69: 130-133.
- Rainford M, Adair R, Scialli AR, Ghidini A, Spong CY (2001) Amniotic fluid index in the uncomplicated term pregnancy, prediction of outcome. J Reprod Med 46: 589-592.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 4911
- [From(publication date):
June-2017 - Aug 16, 2025] - Breakdown by view type
- HTML page views : 3607
- PDF downloads : 1304