Research Article Open Access
Postural Balance Control of the Leprosy Patient with Plantar Sensibility Impairment
Thania Loiola Cordeiro1*, Marco Andrey Cipriani Frade1-3, Ana Regina SB Barros4 and Norma Toraboschi Foss2,41 Programa de Pós-Graduação em Clínica Médica, FMRP – USP, Brazil
2 Divisão de Dermatologia, Departamento de Clínica Médica, FMRP-USP, Brazil
3 Centro de Referencia Nacional em Dermatologia Sanitária HCFMRP-USP, Ribeirão Preto-SP, Brazil
4 Centro de Reabilitação Lucy Montoro HCFMRP-USP, Brazil
- *Corresponding Author:
- Thania Loiola Cordeiro
Departamento de Clínica Médica – HCFMRP. Av. Bandeirantes
3900 - Monte Alegre - CEP: 14049-900 Ribeirão Preto/SP, Brazil
Tel: 551636022447
E-mail: thania.cordeiro@gmail.com
Received date: April 15, 2014; Accepted date: May 12, 2014,; Published date: May 19, 2014
Citation: Cordeiro TL, Cipriani Frade MA, Ana Regina SB Barros and Toraboschi Foss N (2014) Postural Balance Control of the Leprosy Patient with Plantar Sensibility Impairment. Occup Med Health Aff 2:158. doi: 10.4172/2329-6879.1000158
Copyright: © 2014 Cordeiro TL, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Occupational Medicine & Health Affairs
Abstract
Leprosy is a granulomatous disease that affects the peripheral nervous system, leading to loss of thermal, tactile and pain sensibility. Changes in plantar sensibility and proprioception caused by leprosy might affect postural balance control. The Body Center of Pressure (COP) constitutes the neuromuscular response to changes or accelerations of the body’s Center of Gravity and can be affected by orthopedic, neurological or rheumatic injuries. Fifteen multibacillary (MB) and 6 paucibacilary (PB) leprosy subjects were randomly selected, as well as 11 subjects without leprosy for the control group (GC). The MB and PB had their plantar sensibility checked by the Semmens- Weinstein test; all groups had their COP evaluated (stabilometry) using a baropodometer, during standing position with eyes opened and barefooted. The balance variations were measured by the displacement of the COP, as in COP ML (medial-lateral direction) and COP AP (anterior-posterior direction) for right and left feet and total body projection. The stabilometric analysis regarding COP AP revealed no statistically significant difference between groups MB, PB and GC, despite the presence of impaired sensibility in all leprosy patients. The same occurred with the COP ML. The comparison between right and left feet of MB, PB and GC did not show statistically significant differences, although the MB group present the highest variation between the COP projection over right and left feet There were found no consistent evidence suggesting in this study that patients with abnormal plantar sensibility might show disparities when compared to the GC for postural balance control. This is probably due to compensatory adjustments by the vision or ankle joint proprioception. Therefore, it was showed that the reduction on plantar sensibility alone might not be decisive to affect the postural body balance control on leprosy patients, and further investigation is needed.
Keywords
Stabilometry; Leprosy; Sensitivity impairment
Abbreviations
MB: Multibacilary Leprosy Subjects; PB: Paucibacilary Leprosy Subjects; MDT: Multi Drug Therapy; SWtest: Semmens-Weinstein sensibility test; CG: Center of Gravity; COP: Body Center of Pressure; COP ML: Medial to Lateral displacement of the Body Center of Pressure; COP AP: Anterior to Posterior displacement of the Body Center of Pressure; EMG: Electromyography; HCFMRP: Scholl Hospital of Ribeirao Preto; GC: Control Group
Introduction
Leprosy is a granulomatous disease of chronic evolution caused by the bacillus Mycobacterium leprae [1] that leads to specific inflammation with slow evolution, affecting the peripheral nervous system, mainly sensory fibers [2]. The World Health Organization (WHO) estimates that there are 1 million leprosy carriers and currently about 2-3 million people present physical disabilities due to leprosy. According to WHO, the ideal prevalence for leprosy should be of less than 1 case per 10,000 inhabitants. Brazil is among the countries that have not achieved this goal, with current prevalence of 1,24 and second only to India in total number of cases registered. Despite the administration of medication, various degrees of physical disability due to nerve injury and motor sensitive changes can interfere with the social and economic life of the patients, resulting in stigma and discrimination against them [3].
Sensibility loss and its consequences for the leprosy patient
The involvement of autonomic fibers causes alteration of glandular functions, leading to dry skin and mucous membranes as well, and is responsible for the loss of thermal, tactile and pain sensibility. The damaged peripheral motor fibers are responsible for the reduction or abolition of muscular response, paralysis or muscle atrophy [4]. The preserved protective sensory surface (pain, heat, cold) contributes to the regulation of mechanisms that generate vasomotor reflexes and neuromuscular adaptive accommodation for the mechanical protection of the feet. Consequently, the detection of protective sensory losses becomes important to identify peripheral neuropathy, and to avoid plantar ulcer development and eventual amputation of lower limbs [5]. The injury of the sensory fibers is not unique to leprosy. Other diseases such as diabetes, vascular disorders and different neuropathies ou trauma can also generate plantar sensory loss. However, one may find an asymmetric and punctual pattern of insensibility, which is characteristic of leprosy.
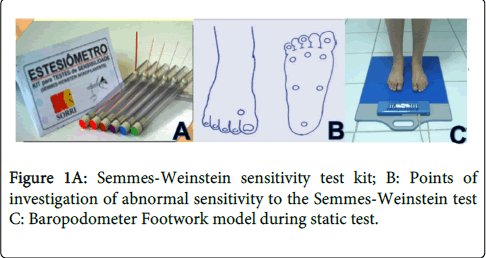
The Semmes-Weinstein test is widely used (SWtest) to evaluate plantar sensibility. It consists of nylon wires of the same size and of different diameters, with a variation of strength of 0.05g to 300g and associated colors in this order: green 0.05 g, 0.2 g blue to violet to 2.0g, 4.0g dark red to orange to 10g, magenta and red to 300g. The loss of protective sensation in the hands and feet is basically indicated by the lack of response to the stimulus of the violet, blue and green filaments [6].
Body balance and plantar sensibility impairment
The body balance maintenance is achieved by the postural control system, and action of the sensory and motor nerves that play this role. These are required to ensure the vertical projection of the body’s center of gravity (CG), which is supposed to be maintained within the base of support (polygon delimited by the lateral edges of the feet) giving stability to the body and allowing the execution of various transactions with its upper segments [7]. The Body Center of Pressure (COP) constitutes the neuromuscular response to changes or accelerations of the CG [8,9] and can be measured by Stabilometry given by a pressure plate. This device quantifies postural oscillations by the projection of the COP for the whole body as well as for each foot, by generating a dithered image of the oscillations, showing an extent area occupied by them. Several pathologies alter the behavior of these postural oscillations, with specific patterns of amplitude and/or frequency. Thus, the stabilometric measure could be used as a reference for monitoring the progress of patients during their treatment [10]. The statocinesiogram is the map of the COP in the anterior-posterior direction (COP AP) versus COP in the mediallateral direction (COP ML) expressed in cm2 and cm (when considering only isolated data for ML and AP), while the stabilogram is the temporal series of COP in each direction: anterior-posterior and medial-lateral expressed in cm/sec [11].
There are several studies on visual or cerebellar influences in stabilometry [12]. However, studies that relate changes in plantar sensibility and stabilometry are scarce. Since postural balance control is dependent on plantar sensibility and on somatossensorial information described by the ankle joint proximal position (through applied pressure and stretching of the tendon and/or muscle), The loss of cutaneous sensibility could be directly related to poor performance for postural control in patients with leprosy, not only by protective and proprioceptive impairment, but also because the disease may affect only one side of the body [13]. The Ministry of Health of Brazil initially adopted a model of classification for leprosy, designating as paucibacillary (PB) or multibacillary (MB) patients with negative and positive bacillus smear, respectively. This classification facilitates the prescription of a suitable multidrug therapy (MDT) [14]. Currently, this classification has been based only upon the number of lesions [15].
Study regarding differences between leprosy patients analyzed the electromyography (EMG) of MB and PB leprosy patients and found that 20% of MB patients had unilateral neural involvement, against 48% of PB patients [16]. Taking these facts into consideration, the aim of this study was to observe the stabilometry patters for individuals with MB and PB leprosy, comparing these results with stabilometry patters of individuals without leprosy.
Material and Methods
Sample
There were randomly selected 21 patients with leprosy all between 18 and 60 years, 15 MB and 6 PB already in multidrug therapy (MDT) treatment at the Schooll Hospital of Ribeirao Preto (HCFMRP), with independent ambulation of orthoses or protheses, and without mechanical impairment associated with neurological disorders, rheumatic, vascular and orthopedic diseases. This sample coincides with another study regarding the variation in percentage of PB group compared to MB in leprosy population [17], whereas MB is more common than PB. There were randomly selected 11 volunteers between 18 and 60 years for the control group (GC) without leprosy, diabetes, or any disease that could compromise plantar sensibility or general joint mobility.
Plantar Sensibility analysis
The plantar sensibility of MB and PB groups was measured using the SWtest (Kit prepared by SORRI, Bauru), along with the plantar mapping points provided by the Ministry of Health of Brasil [18] (Figures 1A and 1B). The patients selected presented 3 or more points of sensory loss (lack of response to the stimulus of the violet, blue and green filaments) altogether for both feet.
Stabilometric evaluation The apparatus used for stabilometry evaluation in groups MB, PB and GC was a pressure plate (Footwork, AM3⌧ - Quart St. Anne 84220 Goult, France) with an active surface plate of 40x40x0,5 cm, and polycarbonate coated capacitors containing 2704 calibrated pressure sensors which detect pressure expressed in Kpa and calculate the projection of the COP and its displacement during static analysis thus generating the stabilometry (Figure 1C). Each subject stood barefoot on the pressure plate for 30 seconds, motionless, with arms along the body and looking to the horizon for the analysis of static posture. The feet were positioned freely, according to their postural habit. The change in balance was measured by the displacement area of the COP, COP ML and AP COP for total body projection, and also the projection on right and left feet.
Data analysis
The Mann-Whitney and Krukall-Wallis tests were used for the statistical analysis.
Results
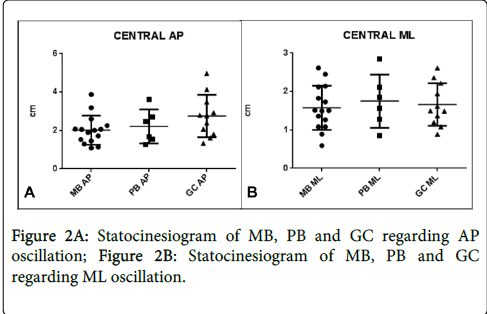
The stabilometric analysis regarding AP oscillation revealed no statistically significant difference (p=0,15) between groups MB, PB and GC, despite the presence of impaired plantar sensibility on all leprosy patients selected (Figure 2A). The same occurred with oscillations at the ML direction (p=0,86) as shown in Figure 2B.
It is worth noting that the GC presented the lowest average (0,92 cm and sd=0,56 ) of sway at ML direction compared to MB (1,58 cm and sd=0,58) and PB (1,75 cm and sd=0,69), but for the AP oscillation the relationship between groups was reversed, and the GC had the highest average of oscillation (2,89 cm and sd=1,10) while MB showed the lowest average (2,02 cm and sd=0,76). PB presented an oscillation average of 2,22 cm and sd=0,88.
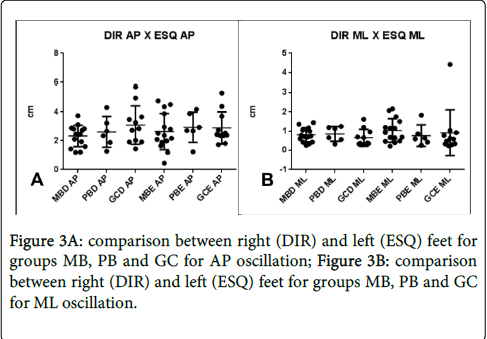
The stabilometric analysis regarding laterality also showed no statistically significant differences. The comparison between movements at AP directions between right and left feet for all groups resulted in p=0,72 (Figure 3A). The same comparison for the oscillations at ML directions resulted in p=0,40 (Figure 3B).
The data analysis for right and left feet separately, comparing the MB and PB groups with the control group showed that the biggest difference can be found within the projection of COP over the left feet, ven though the results were not statistically significant. Of those the greatest variation occurred in the MB group (Table 1). The same table shows the comparison within each group, whereas the MB presented again the greatest variation.
| Groups | P value |
| MBD - MBE | 0,50** |
| MBD – GCD | 0,86 |
| MBE – GCE | 0,23* |
| PBD - PBE | 0,79 |
| PBD – GCD | 0,73 |
| PBE - GCE | 0,52* |
| GCD – GCE | 0,69 |
Table 1: Comparison between leprosy right (MBD and PBD) and left (MBE and PBE) feet with GC right and left feet (GCD and GCE).
Discussion
Plantar peak pressures are a result of displacements of the body center of gravity over the feet due to the adjustment of the diaphragm moving the body to maintain balance by few millimeters on the static position [19].
The importance of the foot to postural control is given by the weight distribution and its corresponding floor reaction response, through the muscular adjustments made mainly by the ankles [20]. The ankle joint usually performs the AP adjustments, while trunk muscles, hip adductors and abductors make the necessary adjustments for ML oscillations [21]. The displacements of COP ML and COP AP describe the adjustments for the postural control.
The equilibrium on static position begins with the sensory system through recognition of space and plantar support areas and continues through transmission of information to the vestibular, motor and central systems for postural adjustments [9]. Any failure in one of these systems may lead to imbalance. Studies showed that by removing one of the regulatory mechanisms of equilibrium from the control group, the results obtained in stabilometry matched those of the patients group with cervical injury and proprioception impairment [21].
On this research we found no statistical evidence that patients with abnormal plantar Sensitivity presented postural balance control disparities compared to GC. Looking back to other studies alike, it can be found that similarly, the assessment of proprioception and anticipatory reaction to postural response in leprosy patients have no statistically significant difference when compared to control group [13]. However, when visual adjustments were suppressed major shifts at the stabilometry of leprosy patients are reveled, even though this commented study does not take into account unilateral or bilateral Sensitivity impairment, or MB/PB classification.
Study with force plates in leprosy patients shows irregularities at the distribution of plantar pressure for MB individuals with altered Sensitivity, which can disrupt the equilibrium [16]. In the same study, the author shows that MB patients have bilateral plantar Sensitivity loss, whereas the PB sensory changes occur mostly unilaterally, and without changes with respect to plantar peak pressure.
The present study revealed no statistically significant differences between the stabilometry for right and left feet, both between groups and inside each group. It was observed that the MB group showed the greatest variation regarding the average values for the projection of the COP over the left foot oscillation when compared to the GC, and with the projection over the right foot for the same group, contradicting the literature researched, which demonstrates that PB are more susceptible to variations between right and left. On the other hand, the previous studies on this matter only took into account the distribution of plantar peak pressures, not the COP oscillation.
Conclusion
This study showed that the impairment of plantar Sensitivity alone might not be decisive to affect the postural body balance control on leprosy patients. It is important to note that this study was conducted as a pilot, and so the small sample collected could be an important limitation. We believed that further research is needed with a larger number of subjects to ensure a more reliable sample regarding unilateral nerve damage on leprosy patients. Also, further investigation about other mechanisms of postural control such as vision and mobility of the subtalar joint (directly related to proprioception) is required for MB and PB patients in order to elucidate the real intervention of lepromatous neuropathy on the body balance.
Acknowledgments
We would like to thank the Doctors, Nurses, Physical Therapists and staff members of the HCFMRP who collaborated for this study, as well as the patients and volunteers who kindly participated.
References
- Aquino DM, Caldas Ade J, da Silva AA, Costa JM (2003) [Profile of leprosy patients in a hiperendemic area of Amazonian Maranhão, Brazil]. Rev Soc Bras Med Trop 36: 57-64.
- Maffei WE (1974) Fisiopatologia e anatomia patológica das infecções, em Fundamentos da Medicina, 229, Fundo Editorial Kyk-Procinex. São Paulo.
- World Healh Organization (2010). Weekly epidemiological record
- Chauhan VS, Pandey SS, Shukla VK (2003) Management of plantar ulcers in Hansen's disease. Int J Low Extrem Wounds 2: 164-167.
- Carvalho VF, Ferreira MC, Vieira SA, Ueda T (2009) [Cutaneous sensibility threshold in the feet of diabetic patients with pressure specified sensory device: an assessment of the neuropathy]. Rev Assoc Med Bras 55: 29-34.
- Marciano LHSC, Garbino JA (1994) Comparação de Técnicas de Monitoramento da Neuropatia Hanseniana: Teste de Sensibilidade e Estudo de Condução Nervosa. Hansen Int 19:5-10.
- Zatsiorsky VM (1997) Kinematics of human motion. Champaign, IL: Human Kinetics.
- Lafond D, Duarte M, Prince F (2004) Comparisson Of Three Methods To Estimate The Center Of Mass During Balance Assessment. J Biomec 37: 1421-1426
- Rubira APFA, Martins MFE, Dente CBS, Gerling NG, Tomas C, et al., (2010) Eficiência da Estabilometria e Baropodometria Estática na Avaliação do Equilíbrio em Pacientes Vestibulopatas. Neurobiologia 73:2.
- Mochizuki L, Amadio AC (2003) Aspectos biomecânicos da postura ereta: a relação entre o centro de massa e o centro de pressão. Revista Portuguesa de Ciências do Desporto 3: 77-83.
- Duarte M, Zatsiorsky VM (2002) Effects of body lean and visual information on the equilibrium maintenance during stance. Exp Brain Res 146: 60-69.
- Oliveira L (1993) Estudo de revisão sobre a utilização da estabilometria como método de diagnóstico clínico. RBE 9:37-53
- Mercadante FA (2010) Avaliação do Controle Postural em Portadores de Hanseníase. São Paulo. Dissertação. Instituto de Psicologia – USP
- Andrade VLG (1996) Paucibacilar ou Multibacilar? Uma contribuição para os serviços de saúde. Hansen. int., 21:6-13.
- Brasil, Ministry of Health (2010) Anexo I – Diretrizes para vigilância, atenção e controle da Hanseníase.
- Cordeiro TL (2011) Baropodometria na Hanseníase e sua Relação com a Alteração de Sensibilidade. São Carlos 79p. Dissertação. Interunidades em Bioengenharia EESC/EQSC/FMRP – USP.
- Mackert CCO (2008) Estudo de base populacional de fatores epidemiológicos de risco em hanseníase. Dissertação (Mestrado) – Pontifícia Universidade Católica do Paraná; Curitiba.
- Brasil(2002) Ministério da Saúde. Secretaria de Políticas de Saúde. Departamento de Atenção Básica (2002) Manual de adaptações de palmilhas e calçados. Brasília.
- Bricot B (2004) Posturologia 3. ed. São Paulo: Ícone, 270 p.
- Stefanello TD JR, Lodi RL (2006) Estudo comparativo de possíveis desequilibrios posturais em pacientes apresentando má oclusão de classe I, II e III de angle, através da plataforma de baropodometria. Arq Cienc Saúde Unipar. 10:139-143
- Madeleine P, Prietzel H, Svarrer H, Arendt-Nielsen L (2004) Quantitative posturography in altered sensory conditions: a way to assess balance instability in patients with chronic whiplash injury. Arch Phys Med Rehabil 85: 432-438.
Relevant Topics
- Child Health Education
- Construction Safety
- Dental Health Education
- Holistic Health Education
- Industrial Hygiene
- Nursing Health Education
- Occupational and Environmental Medicine
- Occupational Dermatitis
- Occupational Disorders
- Occupational Exposures
- Occupational Medicine
- Occupational Physical Therapy
- Occupational Rehabilitation
- Occupational Standards
- Occupational Therapist Practice
- Occupational Therapy
- Occupational Therapy Devices & Market Analysis
- Occupational Toxicology
- Oral Health Education
- Paediatric Occupational Therapy
- Perinatal Mental Health
- Pleural Mesothelioma
- Recreation Therapy
- Sensory Integration Therapy
- Workplace Safety & Stress
- Workplace Safety Culture
Recommended Journals
Article Tools
Article Usage
- Total views: 15517
- [From(publication date):
July-2014 - Aug 31, 2025] - Breakdown by view type
- HTML page views : 10884
- PDF downloads : 4633