Predictors of Time to Recovery from a Surgical Repair of Obstetric Fistula at Mekelle Hamlin Fistula Center, Tigray, Ethiopia
Received: 24-Dec-2017 / Accepted Date: 22-Jan-2017 / Published Date: 29-Jan-2018 DOI: 10.4172/2376-127X.1000364
Abstract
Background: Ethiopia is one of the high fistula burdened countries in the world with an annual occurrence of 3,500 new and existence of 37,500 untreated obstetric fistula cases. Studies conducted in this area focus on determinants of obstetric fistula before surgical repair and researches addressing the associated factors are limited.
Objective: To estimate time to recovery from a surgical repair of obstetric fistula and its associated factors among patients treated at Mekelle Hamlin Fistula Center.
Methods: The data represent random samples of 306 fistula patients treated at Mekelle Hamlin Fistula Center from February 2006 to December 2014. Patients’ background characteristics, obstetric and perioperative information was collected. Comparison of survival time and selection of candidates among categorical variables were done using Kaplan-Meier curve and log rank test. Variables with p-value ≤ 0.25 in bivariate analysis were included in multivariable analysis. Cox proportional hazard assumption, Confounding, Interaction, Multicollinearity and Model fitness were tested: Tables, figures, hazard ratios and 95% confidence intervals were used to present results.
Results: The patients were followed for 6657 person days at risk, the median recovery time was 20 days. The overall recovery rate was 2.5 cases per 100 person days. Multivariable Cox proportional hazard model result showed labor duration of two or more days (AHR=0.73, 95% CI=0.53, 0.99) and post-operative bladder catheterization longer than 14 or more days (AHR=0.45, 95% CI=0.32, 0.62) were factors negatively associated with recovery time from obstetric fistula surgery.
Conclusion and recommendations: women who experienced labor of two or more days and post-operative bladder drainage for more than two or more weeks took longer time to recover after the repair. Therefore, Decision makers, Health care professionals, Stakeholders and Researchers should give emphasis on activities that reduce delays’ in decision making, delays’ in giving urgent intervention and delays’ in reaching health institutions that contributes in reducing complications of prolonged labor ultimately obstetric fistula.
Keywords: Obstetric fistula; Recovery
Abbreviations
AAFH: Addis Ababa Hamlin Fistula Hospital; ARR: Adjusted Risk Ratio; CI: Confidence Interval; cm: centimeter; EDHS: Ethiopian Demographic Health Survey; HR: Hazard Ratio; IQR: Interquartile Range; Kg: Kilogram; MDGs: Millennium Development Goals; MHFC: Mekelle Hamlin Fistula Center; NGOs: Non- Governmental Organizations; RVF: Recto Vaginal Fistula; USAID: United States Agency for International Development; USD: United States Dollars; VVF: Vesico Vaginal Fistula; WHO: World Health Organization; YHFH: Yirgalem Hamlin Fistula Hospital
Introduction
Background
Obstetric fistula is an injury that occurs during prolonged or obstructed labor causing tissue damage to organs inside the pelvis and resulting in incontinence of urine, feces or both. The dead tissues due to prolonged pressure fall away and a hole will be formed between the vagina and bladder called Vesico-vaginal Fistula (VVF) or between the vagina and rectum called Recto Vaginal Fistula (RVF) [1-3].
Obstetric fistula is the worst child birth related complication that contributes for 2.5% of the Global daily death of mothers associated with child birth related complications [4].The main causes of obstetric fistula in the developed world are radiation therapy and surgery whereas in developing countries, “the three delays” are responsible, the delay in seeking skilled emergency obstetric care, the delay in reaching health facility and the delay in receiving a timely intervention after reaching health facility [5]. These predispose laboring mothers to suffer unrelieved obstructed labor and end up with obstetric fistula [1,6-8].
Harmful traditional practices such as early marriage and home delivery are other potential factors for the development of obstetric fistula [8-10]. Globally, nine to 84% of obstetric fistula patients gave birth at home and more than 2 million women are currently living with this problem. Additional 50,000 to 100,000 new cases are estimated to occur each year and majority of which are from Africa and Asia [9-13].
Incidence rates of obstetric fistula in countries with high maternal mortality is as high as two to three cases per 1000 women [14]. Estimated incidence and prevalence of untreated obstetric fistula in Ethiopia during the year 2010 was 3,500 and 37,500, respectively [9,15].
The 2010 Mekelle Hamlin Fistula Center’s (MHFC) report showed that 1000 patients were admitted for treatment of Fistula and 88 patients were referred to Addis Ababa Fistula Hospital (AAFH) in the period between 2006 and 2010 [16].
Consequences of obstetric fistula can be physical, social and psychological traumas. The physical suffering may be damage of skin adjacent to genital areas, cessation of menstruation, vaginal scaring, failure to conceive, bladder stone formation, infections and foot drop associated with neurological injury. Among social and psychological consequences feelings of shame, social isolation, divorce, depression and lack of social support are the major ones [1,2,17,18].
Problem statement
Ethiopia is one of the high-burden countries that constitute the Fistula belt in the world [10]. The estimated coverage of institutional and home deliveries in Ethiopia are 15% and 85%, respectively [19]. Obstetric Fistula results in several consequences to the patient, the family, the community and the country. Isolation of Fistula patients either by themselves or by society inhibits patient’s ability to work and interact with communities. As a result, patients and their entire family driven into poverty through reduction of productivity [2,20,21].
The approximate average cost per Fistula patient in developing countries to cover expense of surgery, postoperative care and physical rehabilitation is $450 United States Dollars (USD) for two to three weeks of hospital stay. That may not be adequate for complicated surgeries such as treating dual vaginal and rectal Fistulas which requires more training than some other corrective surgeries [20].
Obstetric fistula can be avoided and managed if quality emergency obstetric care is available on time for laboring mothers [1,7]. Delaying the age of first pregnancy and stopping harmful traditional practices such as female genital mutilation(FGM) will also reduce the problem [22]. Factors associated with obstetric fistula are similar with that of maternal morbidity and mortality, actions taken to control maternal morbidity and mortality have an impact to address obstetric fistula [23].
Fistula treatment through surgery was successful over 90% of cases at Addis Ababa Fistula Hospital and 88% at Mekelle Hamlin Fistula Center (MHFC), respectively, whereas the proportion of physical closure at Yirgalem Hamlin Fistula Hospital (YHFH) was 81.7% [24- 26]. The operative procedures of repairing Fistula injuries are overt, but the approaches for effective prevention are not well understood. That is mainly because, in countries where Fistulas are highly common there is a complicated relationship between medical, social, economic and environmental factors associated with Fistula [5].
While Ethiopia being one of the major fistulas affected countries, there are scanty of information regarding the fistulacase, its predictors and consequences. More precisely, there are very few data about predictor’s of obstetric fistula analyzed by taking the duration of treatment. Such information is vital for treatment success. Whereas cross-sectional studies conducted in African countries like Congo and Kenya, the contribution of censored subjects were not considered for identifying predictors of obstetric fistula surgical outcome in the analysis.
Previous study conducted in Ethiopia at YHFC on determinants of time to recovery from obstetric fistula surgery by taking one year’s data didn’t address all the peri-operative care related factors associated with Fistula recovery and further it was done in a setting with different socio demographic characteristic [26-28]. Therefore, it is necessary to conduct a research to estimate the time to recovery from obstetric fistula repair and associated factors that affect recovery.
Significance of the study
Obstetric fistula is one of the severe forms of maternal morbidity experienced by women with child birth related complications in Ethiopia. Further, there is a shortage of reliable data around social, demographic and clinical factors associated with time to recovery from obstetric Fistula surgical repair that will be valuable for managing health care institution through planning, monitoring and evaluation of quality of care as well as use of human and material resources [29-35].
Hence, findings of this research will be used to develop and implement health care plan that can be is used for the prevention and management of obstetric fistula at national or subnational level. It can also facilitates evidence based decision making and take appropriate action regarding quality of obstetric services. Moreover, it can be used as base line information for researchers and stakeholders working on reproductive health programs on the same problem.
Objectives
General objective
To estimate time to recovery from surgical repair of obstetric fistula and identify its associated factors at Mekelle Hamlin Fistula Center, Tigray Region, Ethiopia from 2006 to 2014.
Specific objectives
1. To estimate time to recovery from surgical repair of obstetric fistula.
2. To identify factors associated with time to recovery from obstetric fistula repair.
Materials and Methods
Study area and period
This study was conducted from November 27 to December 27/2014 on a dataset of patients who were treated from 2006 to 2014 at MHFC found in Mekelle city that is the capital city of Tigray Regional State. Mekelle is found 783 km far north of Addis Ababa, the capital city of Ethiopia [36-38]. Based on the 2011 EDHS estimate, the total population of the city is 261, 168 of which 126,917 (48.6%) are males and 134,251 (51.4%) are females. Of the total population 51.75% attended primary and above level of education. The health system in Mekelle is consisting of both public and private that encompass not-for-profit clinics which are run by non-governmental organizations (NGOs) such as MHFC [39] .
MHFC is established in February 2006 at Mekelle city and is located proximal to Mekelle regional hospital. It is one of the five mini Fistula hospitals constructed to provide preventive, curative and rehabilitative services to clients coming from urban and rural areas of Tigray and surrounding regions. This institution has been working with the regional health bureau as well as, local and international NGOs to reduce maternal morbidity and mortality.
Study design
A facility based retrospective cohort study design with record review was used to estimate time to recovery from surgical repair of obstetric fistula and identify its associated factors among obstetric fistula patients at MHFC.
Source and Study population
Source population: Medical records of all Fistula patients who undergone obstetric fistula surgery at MHFC from 2006 to 2014.
Study population: All medical records of obstetric fistula patients, who were diagnosed, admitted and operated at MHFC from 2006 to 2014.
Sample population: The sample population for this study was 306 patient medical records who were selected randomly from 1665 medical records of obstetric fistula patients diagnosed, admitted and operated at MHFC from 2006 to 2014.
Inclusion criteria: All patients who were diagnosed admitted and operated for obstetric fistula at MHFC in the period from February 2006 to December 2014.
Exclusion criteria: Patients with incomplete information of the base line and follow up data at least for the main exposure and outcome variable, all cases of Fistula with history of previous repair other than MHFC and patients who came with successfully closed Fistula at the time of diagnosis were excluded from this study.
Sample size determination
STATA analytical software version 12 was used to calculate the sample size for proportional hazard regression model by taking 80% power, 5% level of significance and standard deviation of 0.5. From previous study proportion of subjects withdrawn from the study (18.3%), the over all probability of the Fistula closure (81.7%) and hazard ratio among patients who delivered at home and at health institution (1.481) were considered to calculate the sample size [26]. Finally a total of 306 samples were obtained.
Sampling procedures
Medical records of 1,665 patients who had undergone obstetric fistula surgery at MHFC in the period between February 2006 and December 2014 were selected according to eligibility criteria. Of these records of obstetric fistula patients, 306 study subjects were selected by simple random sampling using random number generated by Microsoft Excel application.
Data collection tools and procedures
The data were extracted from patient’s card, registers and operative notes using a data extraction tool adopted from standard study report forms developed and utilized by all Fistula centers in Ethiopia. The data extraction tool included information regarding patients’ Sociodemographic, Economic and obstetric characteristics as well as anatomical and clinical characteristics of Fistula, preoperative, intra operative and post-operative procedures. The data collection was done by three healthcare professionals who have Bachelor of Science (B.Sc.) degree and experience in data collection. That were recruited and trained by the investigator. Finally, the data was collected from November 27 to December 27, 2014 under supervision of the principal investigator.
Study variables
Dependent variable: Recovery from Fistula Surgery: Status of recovery from Fistula surgery (primary repair) is defined using two indicators, status of Fistula closure and patient’s post-repair stress incontinence by using Andrew Browning’s method [40-42].
The surgical outcome of obstetric fistula was considered as recovered if a woman operated for VVF is cured (Fistula closed and patient is dry) or cured but wet (Fistula closed and patient has mild stress incontinence) or if a woman operated for RVF is cured (anal sphincter intact and patient is continent) or (anal sphincter intact but leaks flatus and her Fistula wound is closed) or if a woman operated for combined VVF and RVF fulfills the criteria of recovery for both VVF and RVF within 21 days following surgery.
Whereas the surgical outcome of VVF was considered as not recovered, if a woman operated for Fistula had moderate to severe urinary incontinence, or stress incontinence of Andrew Browning’s grade (b) and beyond or confirmed that the Fistula wound is not closed (break operations) and/or if a woman operated for RVF has non-intact anal sphincter and has leakage of stool or confirmed that her Fistula wound is not closed within 21days following surgery.
The dependent variable in this study is “recovery status” from a surgical repair of obstetric fistula.
A. Recovery status=Event (yes) if the patient was recovered from a surgical repair of obstetric fistula within 21 days following surgery.
Recovery status=Censored (no) if the patient was not recovered from a surgical repair of obstetric fistula within 21 days following surgery and if a patient was died following operation. The recovery status was coded as 1 for event and 0 for censored.
B. Time-The difference between date of surgery and date of event or censorship.
Three groups of independent variables are included in this study. Based on literature review and available data on standard report forms of MHFC, the independent variables are summarized below.
Socio-demographic and economic factors: Patient’s date of hospital visit, age, marital status, educational status, time taken for travel, source of help and religion were included.
Patients’ obstetric history: Information regarding history of pregnancy, anti-natal care and number of children the patient had, details of conditions related to causative delivery and delivery outcome were included.
Perioperative factors: Fistula characteristics, presence of scarring, involvement of adjacent organs, pre-operative, intra-operative and post-operative cares about surgical procedure performed, antibiotics administered, type of anesthesia used, type of surgical route and repair, type and duration of catheterization, previous repair attempt and presence of post-operative complications were also described.
Data processing and management
After the data is extracted, data entry, coding, categorizing and labeling were done by using STATA analytical software version 12 accordingly to make the data ready for analysis.
Data quality assurance
Data cleaning was done to ensure completeness, consistency and extreme values. In order to improve the quality of the data, data collectors were given two days of training which focus on the objective of the study, use of facility’s report forms and the importance of filling out data extraction tool completely and accurately. Before data collection the data extraction tool was pretested on 5% of the sampled patient records found at Mekelle Hamlin Fistula Center to check for easy transformation of information from the facility formats into the data extraction tool and to minimize missing of information.
During the data collection and at the end of each day, checking of each completed data extraction tool was done by the investigator against the medical records from which the data was extracted.
Data analysis
After completing data cleaning and normality checkups of continuous variables, the data was analyzed using STATA analytical software version 12. Median with inter quartile range for continues nonparametric variables was used as reported measures of central tendency and variation respectively. Likewise, frequency and percentage were used for description of categorical predictors of the study population.
To compare time to recovery among the categories and to select a predictor to the full model, all the categorical predictors were tested using Kaplan-Meier curve and log rank test, whereas continuous variables were tested using univariate cox proportional hazard regression model. Variables with a cutoff point of p-value ≤ 0.25 were taken to multivariable analysis by using purposive candidate selection criteria [43].
Multivariable Cox proportional hazard regression model was used to assess the independent factors associated with time to recovery. Stepwise backward elimination model building procedure was used, along with comparing each model by using likely hood ratio test. Interaction and cofounding were checked using a cutoff point of change in beta greater than 20% [43].
The final model was checked for satisfying the assumption of proportionality by using global test based on Schoenfeld residual. Whereas the existence of Multicollinearity was checked using a cutoff point of mean variance inflation factor (VIF)>10): Cox and Snell’s residual analysis (Nelson Aalen cumulative hazard function against Cox and Snell’s residual) was used for checking model fitness [43,44]. The association between predictors and time to recovery was interpreted using hazard ratios and all statistical significances were conducted at 95% confidence interval.
Ethical clearance
Ethical clearance was obtained from the ethical review board of Mekelle University, College of Health Sciences and department of Public Health. Permission was obtained from Hamlin Fistula International Ethiopia. The confidentiality of information regarding patients involved in this study was maintained to the maximum extent possible along with keeping all patient records within the study site and avoidance of identifying study participants by name on any documentation, report or publication resulting from data collected in this study.
Results
Descriptive statistics
Patient’s socio demographic and economic factors: A total of 306 patients who have undergone obstetric fistula surgery were included in the study, of which 165 (53.92%) had recovered after surgery while 141 (46.08%) were censored. Among 300 participants 152 (50.66%) of the patients were dependent on their family for care and support, 226 (74.34%) were illiterate. Among 295 patients whose body weight was measured, 197 (66.78%) had weight less than 50 Kg. Height was measured on 296 patients and 75% of these were taller than 150 cm.
Pertaining to the patients current age, among 277 respondents 167 (60.28%) were in the age group of 20-34years category. When we see the patients age at causative delivery, of 306 patients 191 (62.42%) were in the same age group of 20-34 years. Regarding to the patients age at marriage, from 286 observed patients 193 (67.48%) were in the age group of 15-20 years. regarding patients marital status, of 301 patients 209 (69.43%) were married (Table 1).
| Variable |
N |
Category | Frequency | Percent (%) |
|---|---|---|---|---|
| Marital status |
301 |
Married | 209 | 69.43 |
| Others | 93 | 30.56 | ||
| Educational status |
304 |
Illiterate | 226 | 74.34 |
| Primary | 58 | 19.07 | ||
| Secondary and above | 20 | 7.59 | ||
| Source of help or support |
300 |
Dependent on husband | 102 | 34.00 |
| Dependent Family/donor dependent | 152 | 50.66 | ||
| Independent | 46 | 15.33 | ||
| Current age |
277 |
<20 | 41 | 14.81 |
| 20-34 | 167 | 60.28 | ||
| >34 | 69 | 24.91 | ||
| Age at causative delivery |
306 |
< 20 | 69 | 22.55 |
| 20-34 | 191 | 62.42 | ||
| >34 | 46 | 15.03 | ||
| Age at marriage |
286 |
<15 | 50 | 17.48 |
| 15-20 | 193 | 67.48 | ||
| >=20 | 43 | 15.03 | ||
| Patients’ weight |
295 |
< 50kg | 197 | 66.78 |
| >=50kg | 98 | 33.22 | ||
| Patients’ height |
296 |
< 150cm | 74 | 25.00 |
| > =150cm | 222 | 75.00 | ||
| Type of transport |
305 |
Foot ,stretcher, foot and stretcher | 8 | 2.62 |
| By bus/taxi/trucks | 21 | 6.89 | ||
| Foot and bus/taxi/trucks | 276 | 90.49 | ||
| Time take to reach HI by car |
294 |
1/2 to 1 day | 228 | 77.55 |
| 1- 2 day | 51 | 17.35 | ||
| >= 2 days | 15 | 5.10 | ||
| Time take to reach HI on foot |
262 |
<1 day | 189 | 72.14 |
| 1to2 days | 55 | 20.99 | ||
| >=2 | 18 | 6.87 |
Table 1: Background characteristics of patients treated at MHFC from 2006 to 2014.
Obstetric characteristics: From the study participants 113 (37.05%) were pregnant for two to four times, 193 (65.87%) had at least one ANC follow-up for their causative delivery and 177 (58.80%) had two and more days of labor. From the participants 201 (66.12%) had spontaneous or assisted vaginal causative delivery. Nearly 270 (90%) of the patients’ causative delivery was end up with still birth and 201 (65.69%) of the patients had more than one child. Regarding place of causative delivery, 211 (68.95%) of the patients gave birth at health institution (Table 2).
| Variable | N | Category | N (%) | Percent (%) |
|---|---|---|---|---|
| Gravida | 305 | 1 pregnancy | 104 | 34.10 |
| 1-4 pregnancy | 113 | 37.05 | ||
| >=5 pregnancy | 88 | 28.85 | ||
| Antenatal care follow-up | 293 | No | 100 | 34.13 |
| Yes | 193 | 65.87 | ||
| Duration of causative labor | 301 | < 2 days | 124 | 41.20 |
| >= 2 days | 177 | 58.80 | ||
| Mode of delivery | 304 | Abdominal | 103 | 33.88 |
| SVD/AVD** | 201 | 66.12 | ||
| Number of delivery | 306 | One child | 105 | 34.31 |
| More than one child | 201 | 65.69 | ||
| Causative delivery outcome | 304 | live birth | 34 | 11.18 |
| Still birth | 270 | 88.82 | ||
| Number of children alive | 306 | No children | 110 | 35.95 |
| One to four | 151 | 49.35 | ||
| More than four | 45 | 14.71 | ||
| Place of delivery | 306 | Home | 95 | 31.05 |
| Health institution | 211 | 68.95 |
Table 2: Obstetrics characteristics of fistula patients treated at MHFC, 2006-2014.
Peri-operative conditions: From the total patients, 165 (53.92%) were recovered with-in recommended 21 days. Among 302 patients 174 (57.62%) were suffering from incontinence for 3 to7 months. Considering to post operative catheterization, more than half of the patients 178 (58.17%) were catheterized for less than 14 days. Concerning to circumcision, from 289 patients 239 (82.70%) were not circumcised.
254 (84.39%) of the patients were operated for the first time at MHFC. Among 284 patients observed, 147 (51.76%) had mild virginal scar. Pertaining to bladder size of patient, 129 (47.60%) had fair bladder size and 177 (67.82%) had intact bladder neck. Post operative antibiotics administration for prophylaxis or treatment was reported for 255 patients, among these 182 (71.37%) had received Post operative antibiotics (Table 3).
| Variable | N | Category | Frequency | Percent (%) |
|---|---|---|---|---|
| Recovery status | 306 | Recovered | 165 | 53.92 |
| Not recovered | 141 | 46.08 | ||
| Duration of incontinence in months | 302 | <3 | 17 | 5.63 |
| 3-7 | 174 | 57.62 | ||
| >=7 | 111 | 36.75 | ||
| Circumcision | 289 | Circumcised | 50 | 17.30 |
| Not circumcised | 239 | 82.70 | ||
| History of previous repair | 301 | No | 254 | 84.39 |
| Yes | 47 | 15.61 | ||
| Vaginal scar | 284 | No scar | 87 | 30.63 |
| Mild | 147 | 51.76 | ||
| Moderate to severe | 50 | 17.61 | ||
| Bladder size | 271 | None or small | 49 | 18.08 |
| Fair | 129 | 47.60 | ||
| Good | 93 | 34.32 | ||
| Status of bladder neck | 261 | Partial damage | 40 | 15.33 |
| complete damage | 44 | 16.86 | ||
| Intact | 177 | 67.82 | ||
| Duration of bladder catheter | 306 | <14days | 178 | 58.17 |
| >=14days | 128 | 41.83 | ||
| Post-operative-antibiotics | 255 | No | 73 | 27.75 |
| Yes | 182 | 71.37 |
Table 3: Peri-operative conditions of patients treated at MHFC, from 2006 to 2014.
Survival analysis
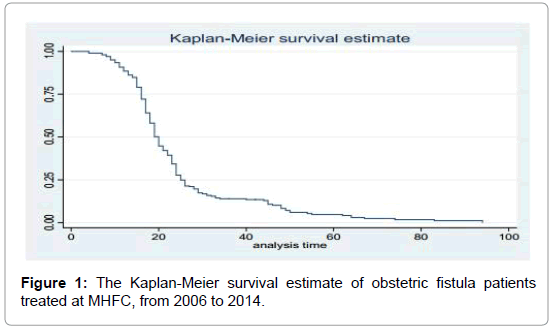
The median time of a patient stay in the hospital to treated and physically cured is 19 days. The median recovery time for patients who delivered at health institution was a year lower than (19 days) who delivered at home (20 days). The patients were followed for a total of 6657 person days at risk. The overall median recovery time among fistula patients who operated in MHFC was 20 days. The rate of recovery for patients whose causative delivery being at home and health institution was 2.5 cases per 100 person days, 95% CI=(1.9, 3.3) and 2.4 cases per 100 person days, 95% CI=(2.0, 2.9), respectively.
The Kaplan-Meier curve displayed below shows the overall survival status of patients was decreasing through the study time (Figure 1).
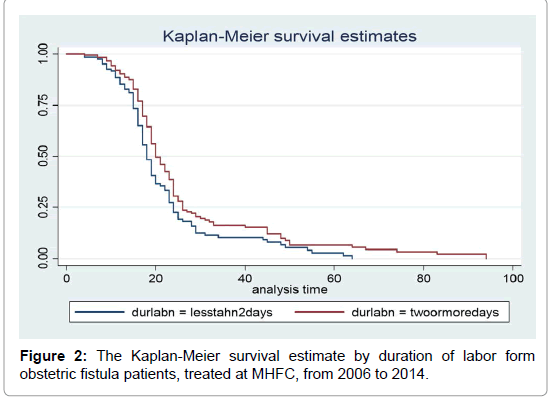
The Kaplan-Meier curve and log rank test result displayed below shows, the estimated difference in survival status of patients based on duration of labor less than 2 days and duration of labor of 2 or more days (P=0.0105), i.e., the recovery time is longer for those patients who were in labor for two or more days than patients in labor for less than 2 days (Figure 2).
One patient who delivered at home and five patients who delivered at health institution recovered in the first week following obstetric fistula surgery respectively. Higher recovery rate was seen in the 2 to 3 weeks following obstetric fistula surgical repair among patients who delivered at home and who delivered at health institution, respectively (Table 4).
| pdnew | person-time | failures | rate | [95% conf. Interval] | |
|---|---|---|---|---|---|
| Home and ~S | |||||
| (0-7) | 662.00 | 1 | 0.15 | 0.02 | 1.07 |
| (7-14) | 633.00 | 7 | 1.11 | 0.53 | 2.32 |
| (14-21) | 414.00 | 45 | 10.87 | 8.12 | 14.56 |
| >21 | 374.00 | 0 | 0.00 | . | . |
| HI | |||||
| (0-7) | 1471.00 | 5 | 0.34 | 0.14 | 0.82 |
| (7-14) | 1334.00 | 33 | 2.47 | 1.76 | 3.48 |
| (14-21) | 852.00 | 74 | 8.69 | 6.92 | 10.91 |
| >21 | 917.00 | 0 | 0.00 | . | . |
| total | 6657.00 | 165 | 2.48 | 2.13 | 2.89 |
Table 4: Comparison of recovery rates per 100-person days at risk by place of delivery after Obstetric fistula surgery among patients treated at MHFC from 2006 to 2014.
Bivariate analysis
In bivariate analysis, current age, age at causative delivery, age at marriage, weight, height, Source of help, gravidity, ANC, labor duration, number of delivery, number of children, duration of bladder catheter, bladder neck status, bladder size, circumcision type, previous fistula repair history, incontinence duration and post operative antibiotic use had p-value<0.25 and are a potential candidate for multivariable Cox regression analysis (Table 5).
| Variable | log rankest | Df | p-value | AHR (95%CI) |
|---|---|---|---|---|
| Socio demographic and economic factors | ||||
| Patients current age | 3.74 | 2 | 0.1542 | |
| Age at causative delivery | 2.9 | 2 | 0.2351 | |
| Age at marriage | 3.34 | 2 | 0.1881 | |
| Patients weight | 1.34 | 2 | 0.2473 | |
| Patients height | 2.45 | 1 | 0.1174 | |
| Patients educational status | 1.43 | 2 | 0.4893 | |
| Type of transport | 1.92 | 2 | 0.3837 | |
| Time taken to reach HI by car | 1.87 | 2 | 0.3928 | |
| Time taken to reach HI on foot & others | 0.93 | 2 | 0.6283 | |
| Patients source of help | 5.14 | 2 | 0.0767 | |
| Patients marital status | 0.02 | 1 | 0.8921 | |
| Obstetrics factors | ||||
| Number of pregnancy | 3.01 | 2 | 0.2216 | |
| ANC follow up | 5.22 | 1 | 0.0223 | |
| Place of delivery | 0.07 | 1 | 0.7899 | |
| Duration of labor | 6.54 | 1 | 0.0105 | 0.73 (0.53, 0.99) |
| Number of delivery | 2.58 | 1 | 0.1085 | |
| Number of children alive | 6.89 | 2 | 0.0318 | |
| Mode of delivery | 0 | 1 | 0.9558 | |
| Causative delivery outcome | 0.03 | 1 | 0.852 | |
| Peri-operative factors | ||||
| Duration of bladder catheter | 17.96 | 1 | 0 | 0.45(0.32, 0.62) |
| Status of bladder neck | 3.94 | 2 | 0.1391 | |
| Primary repair history | 2.38 | 1 | 0.1229 | |
| Bladder size | 14.35 | 2 | 0.0008 | |
| Post-operative antibiotics | 1.43 | 1 | 0.2323 | |
| vaginal scar | 1.55 | 2 | 0.46 | |
| Circumcision | 3.3 | 1 | 0.0693 | |
| Duration of incontinence | 4.79 | 2 | 0.0911 | |
*DF-degrees of freedom
Table 5: Log rank test and adjusted analysis for patients treated at MHFC from 2006 to 2014.
Multivariable analysis
Among the eighteen variables that had satisfied the purposeful selection criteria of p-value<=0.25 to be a potential candidate for multivariable analysis, two predictors (duration of labor for causative delivery and duration of post operative catheterization) had statistically significant association with time to recovery.
Factors influencing time to recovery from obstetric fistula surgery
By controlling the effect of duration of bladder catheterization, the recovery time was slower by 27% for patients whose duration of labor for their causative delivery was two or more days (AHR=0.73, 95% CI=0.53, 0.99). After adjusting for the effect of duration of labor for the causative delivery, the rate of recovery from obstetric fistula surgical repair among patients whose bladder was catheterized for fourteen and more days was 55% reduced to recover than patients whose bladder was catheterized for less than fourteen days (AHR=0.45, 95% CI=0.32, 0.62) (Table 4).
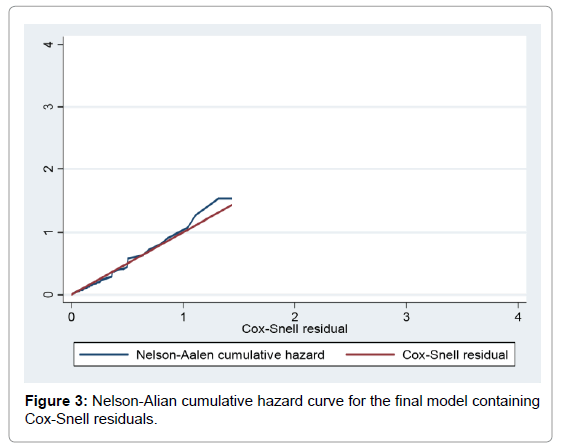
Goodness of fit of the final model
The fit of the model was evaluated by using the Cox-Snell residuals with fitting the model using the stcox command. Finally, the Nelson- Aalen cumulative hazard function plot was seen to compare the hazard function to the diagonal line. Since the hazard function follows the 45 degree line, the model best fits the data (Figure 3).
Discussion
This study was conducted to estimate the time to recovery and to identify predictors of recovery from a surgical repair of obstetric fistula among patients treated at MHFC in the period 2006 to 2014. A total of 306 patients who have undergone obstetric fistula surgery were included in the study of these 165 (53.92%) had recovered in the recommended time. The median time of a patient stay in the hospital to be recovered was 19 days (2.71) weeks which is not consistent with the study finding at YHFC, Ethiopia which is 4.1 weeks [26].
Possible reasons for this inconsistency might be variation on quality of care provided for patients at different levels. the study also found out that, the overall rate of recovery from a surgical repair of obstetric fistula was 2.5 per 100 person days at risk, which was not very much different for those who delivered at home and at health institution whose recovery rate was 2.54 and 2.44 per 100 person days at risk, respectively.
The median recovery time for patients who delivered at health institution was lower (19 days) than who delivered at home (20 days). This means those patients whose place of causative delivery was at health institution recover one day earlier than whose place of causative delivery was at home. The patients were followed for a total of 6657 person days at risk and over all recovery rate=2.5 cases per 100 person days at risk, 95% CI=(2.1, 2.9). The overall median recovery time among fistula patients who operated in MHFC was 20 days. The rate of recovery for patients whose causative delivery being at home and health institution was 2.5 cases per 100 person days at risk, 95% CI=(1.9, 3.3) and 2.4 cases per 100-person days at risk, 95% CI=(2.0, 2.9), respectively.
From the results of multivariable Cox’s proportional hazard regression model, it was found that, duration of labor and duration of bladder catheterization were independent predictors of time to recovery from a surgical repair of obstetric fistula. In the current study, sustained labor for two or more days was identified as independent predictor of time to recovery from obstetric fistula surgical repair. The rate of recovery was reduced by 27% for patients who were in labor for two or more days. This implies that patients whose causative delivery took more than two days of labor took longer time to recover after surgery than their counter parts. This finding is comparable with the study done in Yirgalem, Ethiopia [26]. Which implies, there could be a delay in decision making to visit health institution during the onset of labor or a delay while transportation or a delay in making intervention after reaching health institution. Eventually, the unrelieved prolonged labor badly damages soft tissues of the pelvic organs and results in complex Fistula that make patients incontinent even after surgical therapy [45].
Urinary bladder catheterization was also a prognostic factor that significantly predicts time to recovery from a surgical repair of obstetric fistula. The current study showed the rate of recovery decreased by 55% among patients whose bladder was catheterized for fourteen days and more, than patients whose bladder was catheterized for less than 14 days. This implies patients whose bladder was catheterized for fourteen days and more, recover later than those who were in labor for less than two weeks.
That is consistent with the fact that continuous bladder drainage of high volume urine for not more than 14 days is the base of success in Fistula repair. Moreover, continuous bladder drainage through folly catheter helps the bladder repair to heal without distension and reduces the risk of infection, breakdown of repair and patient’s hospital stay. Since recovery after surgery generally takes two weeks, patient’s bladder needs drainage through a catheter traditionally for two weeks [32,46,47].
This is also in agreement with the findings of a multi country study that has involved patients from 11 study sites in Uganda, Guinea, Niger, Nigeria and Bangladesh which dictate’s duration of catheterization for 14 days and more was associated with failure to close the Fistula compared to women catheterized for less than 14 days [32,48]. There is no statistically significant deference on multi variable analysis among patients who delivered at home and at health institution. It is not consistent with the study finding at Yirgalem, Ethiopia [26]. Possible reasons for this inconsistency might be in the current study participant came long time after onset of labor, delay on reaching health facility.
The main implication of this study is to provide up-to-date information regarding factors associated with time to recovery from obstetrics fistula surgery. This study found out that prolonged labor and prolonged duration of urinary catheterization were statistically and significantly associated with time to recovery from obstetrics fistula surgery. Since fistula is one of the sever form of maternal morbidity it is necessary to prevent, identify and manage accordingly. These activities require the commitment of health policy makers. Therefore, it is better to monitor and evaluate the existing basic and comprehensive emergency obstetrics care and implementation of clinical guidelines regarding prevention, treatment and follow-up of patients with obstetrics fistula.
Conclusion
In conclusion, the overall median recovery time for patients who treated at MHFC was 20 days with overall recovery rate of 2.5 cases per 100 person day at risk. Duration of post-operative bladder catheterization and duration causative delivery were independent predictors of time to recovery from obstetric fistula surgical repair. Even though time to recovery was shorter by one day for those patients whose place of causative delivery at health institution, there is no statistically significant deference on multi variable analysis among patients based on their place of causative delivery.
Recovery from obstetric fistula repair was influenced by prolonged labor which in turn results in obstructed labor that may end up with one of the severe obstetric morbidity called obstetric fistula. Since duration of post-operative bladder catheterization and duration causative delivery were independent predictors of time to recovery from obstetric fistula surgical repair, health care providers and officials of health facility should give special emphasis in addition to routine care. Finally, prospective study is recommended to come up with the real-life determinants.
Recommendations
Treatment provision is not adequate in tackling problems associated with obstetric fistula: Therefore, it is important to identify factors that affect time to recovery from obstetric fistula surgery and intervene accordingly. Therefore, for the better treatment of obstetric fistula, the following recommendations are forwarded:
For ministry of health
Because availability of quality obstetric service has an impact for recovery from obstetric fistula surgery, Ministry of Health should address the issue of advanced training and distribution of adequate number of surgeons that can reduce the time spent for surgical repair and reduce post-operative bladder catheterization throughout treatment facilities. Furthermore recruitment, training and distribution of more midwives throughout health care facilities need to be emphasized to reduce the delay in giving early intervention for prolonged labor which can reduce the consequences of prolonged labor along with monitoring and evaluation of service quality. Ministry of Health should also give emphasis on activities including, increasing access to adequate obstetric care.
Stakeholders
Stakeholders such as Engender Health, UNPF (United Nations Population Fund) and AusAID (Australian agency for international development) should give more attention to work with teaching institutions for producing adequate number of qualified health care professionals. They should also engage in upgrading the existing health care facilities to provide obstetric fistula surgical repair where the service was unavailable: Both of which may reduce the delay in seeking treatment, the delay in getting early intervention and the delay in reaching health institutions due to lack of access.
Mekelle Hamlin Fistula Center
Since long duration of post-operative bladder catheterization has an impact on delay in recovery time, hence MHFC should work in such a way that reduces duration of post-operative catheterization by following up-to-date guideline and maintain standard of care.
Healthcare professionals
Health care professionals should give special emphasis in providing timely emergency obstetric care when laboring mothers arrive and they should use standardized preventive and curative guidelines that benefit laboring mothers.
Researchers
In this study much of the pre-operative and post-operative factors associated with Fistula patients were not addressed well due to unavailability of data. Hence further prospective studies need to be conducted to estimate the real median time to recovery and its associated factors and to address un-addressed predictors.
Acknowledgement
First, I would like to express my deepest gratitude to my advisors Dr. Araya Abrha Medhanyie (PhD) and Mr.Tesfay Hailu (MPH) for their excellent guidance, ongoing advice and provision of good atmosphere for doing this research paper. Secondly, my special thanks go to Mekelle University, College of Health Sciences Department of Public Health for offering opportunity of doing this research. Lastly, I forward my appreciation to Dr. Melaku Abrha (MD) and Dr. Fekade Ayenachew (MD) who were willing in providing the necessary support and information to accomplish this research.
References
- Wall L (2006) Obstetric vesicovaginal fistula as an international public-health problem. Lancet 368: 1201-1209.
- Hancock B (2009) Practical obstetric fistula surgery. Royal Society of Medicine Press Ltd, UK.
- Frajzyngier V, Ruminjo J, Barone MA (2012) Factors influencing urinary fistula repair outcomes in developing countries: A systematic review. Am J Obstet Gynecol 207: 248-258.
- (UNFPA) United Nations Population Fund (2012) When childbirth harms: Obstetric fistula.
- Wall L (2012) Preventing obstetric fistulas in low-resource countries: Insights from a Haddon matrix. Obstet Gynecol Surv 67: 111-121
- (2012) Assessing progress towards the Millennium Development Goals. Ethiopia MDGs Report.
- Wall LL (2012) A framework for analyzing the determinants of obstetric fistula formation. Stud Fam Plann 43: 255-272.
- Holme A, Breen M, MacArthur C (2007) Obstetric fistulae: A study of women managed at the Monze Mission Hospital, Zambia. BJOG 114: 1010-1017.
- Duby F, Hailey J (2013) Joint AusAID and USAID review of support to Hamlin fistula Ethiopia services order 230: In final report.
- Pierre MT, Fomulu JN, Khaddaj S, De-Bernis L, Delvaux T, et al. (2012) Risk factors for obstetric fistula: A clinical review. Int Urogynecol J 23: 387-394.
- Ortiz-Echevarria L (2013) An integrated approach to obstetric fistula prevention, care and treatment: URC combats a tragic, but preventable medical problem.
- UNFPA (2003) Second meeting of the working group for the prevention and treatment of obstetric fistula. Addis Ababa.
- Bacon C (2003) Obstetric fistula needs assessment report: Findings from nine African countries.
- Pathfinder International (2014) Strengthening the continuum of care for fistula prevention and repair in Ethiopia.
- (2012) Fistula treatment in Tigray region: The future of training in obstetrics and gynecology. In Proceedings of the 20th Annual Conference of the Ethiopian Society of Obstetricians and Gynecologists. ESOG: Mekelle.
- Alio AP, Merrell L, Roxburgh K, Clayton HB, Marty PJ, et al. (2011) The psychosocial impact of vesico-vaginal fistula in Niger. Arch Gynecol Obstet 284: 371-378.
- Ahmed S, Holtz SA (2007) Social and economic consequences of obstetric fistula: Life changed forever? Int J Gynecol Obstet 99: S10-S15.
- (2014) Ethiopia mini demographic and health survey. Central Statistical Agency, Ethiopia.
- Nicol M (2005) Conference of east, central and southern Africa obstetricians and gynecologists. Tanzania. Dares salaam: Women’s dignity project.
- Tamirat BT (2007) Situational analysis of obstetric fistula in the Gambia report 2007. UNFPA and WHO.
- WHO (2006) Integrated management of pregnancy and childbirth. In: Lewis G, Bernis Ld (Eds), Obstetric fistula: Guiding principles for clinical management and programme development.
- Mulu M (2012) The future of training in obstetrics and gynecology different strategic approach in obstetric care and trainings. In: Proceedings of the 20th Annual Conference of the Ethiopian Society of Obstetricians and Gynecologists. ESOG.
- Getachew T, Hewson P, Taye A (2014) Survival analysis of time to recovery from obstetric fistula: A case study at Yirgalem Hamlin Fistula Hospital, Ethiopia.
- Hawkins L, Spitzer RF, Christoffersen-Deb A, Leah J, Mabeya H, et al. (2013) Characteristics and surgical success of patients presenting for repair of obstetric fistula in western Kenya. Int J Gynecol Obstet 120: 178-182.
- Sjoveian S, Vangen, S, Mukwege D, Onsrud M (2011) Surgical outcome of obstetric fistula: A retrospective analysis of 595 patients. Acta Obstet Gynecol Scand 90: 753-760.
- Tafesse B, Muleta M, Michael AW, Aytenfesu H (2006) Obstetric fistula and its physical, social and psychological dimension: The Ethiopian scenario. Acta Urológica 23: 25-31.
- Krause HG, Natukunda H, Singasi I, Hicks SSW, Goh JTW (2014) Treatment-seeking behaviour and social status of women with pelvic organ prolapse, 4th degree obstetric tears and obstetric fistula in western Uganda. Int Urogynecol J 25: 1555-1559.
- Raassen TJ, Verdaasdonk EG, Vierhout ME (2008) Prospective results after first-time surgery for obstetric fistulas in East African women. Int Urogynecol J 19: 73-79.
- Tafesse B (2008) A new classification of female genital fistula. J Obstet Gynaecol Can 30: 394-395.
- Browning A (2006) Risk factors for developing residual urinary incontinence after obstetric fistula repair. BJOG 113: 482-485.
- Roy KK, Malhotra N, Kumar S, Seth A, Nayar B (2006) Genitourinary fistula: An experience from a tertiary care hospital. JK Sci 8: 144-147.
- Barone MA, Frajzyngier V, Ruminjo J, Asiimwe F, Barry TH, et al. (2012) Determinants of postoperative outcomes of female genital Fistula repair surgery. Obstet Gynecol 120: 524-531.
- Kayondo M, Wasswa S, Kabakyenga J, Mukiibi N, Senkungu J, et al. (2011) Predictors and outcome of surgical repair of obstetric fistula at a regional referral hospital, Mbarara, western Uganda. BMC Urol 11: 2-9.
- Goh JT, Browning A, Berhan B, Chang A (2008) Predicting the risk of failure of closure of obstetric fistula and residual urinary incontinence using a classification system. Int Urogynecol J 19: 1659-1662.
- Giorgi G, Krishnan K (2009) A water and sanitation needs assessment for Mekelle city, Ethiopia. In: MCI social sector working paper series.
- Dannecker C, Friese K, Stief C, Bauer R (2010) Urinary incontinence in women. Dtsch Arztebl Int 107: 420-426.
- Bishinga A, Zachariah R, Hinderaker S, Tayler-Smith K, Khogali M, et al. (2013) High loss to follow-up following obstetric fistula repair surgery in rural Burundi: Is there a way forward? PHA 3: 113-117.
- Waaldijk K (2004) The immediate management of fresh obstetric fistulas. Am J Obstet Gynecol 191: 795-799.
- Hosmer DW, Lemeshow S, May S (2008) Applied survival analysis: Regression modeling of time-to-event data. 2nd Edn, Wiley Series in Probability and Statistics
- Forthofer RN, Lee ES, Hernandez M (2007) Biostatistics: A guide to design, analysis and discovery. 2nd Edn.
- De-Ridder D, Badlani GH, Browning A, Singh P, Sombie I, et al. (2009) Fistulas in the developing world.
- Dangal G, Thapa K, Yangzom K, Karki A (2013) Obstetric fistula in the developing world: An agonising tragedy. NJOG 8: 5-15.
- Barone MA, Frajzyngier V, Arrowsmith S, Ruminjo J, Seuc A, et al. (2012) Non-inferiority of short-term urethral catheterization following fistula repair surgery: Study protocol for a randomized controlled trial. BMC Womens Health 12: 5.
- Frajzyngier VM (2011) Toward a better understanding of urinary fistula repair prognosis: Results from a multi-country prospective cohort study.
- Browning A (2006) A new technique for the surgical management of urinary incontinence after obstetric fistula repair. BJOG 113: 475-478.
Citation: Hailu S (2018) Predictors of Time to Recovery from a Surgical Repair of Obstetric Fistula at Mekelle Hamlin Fistula Center, Tigray, Ethiopia. J Preg Child Health 5: 364. DOI: 10.4172/2376-127X.1000364
Copyright: © 2018 Hailu S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 7109
- [From(publication date): 0-2018 - Dec 09, 2025]
- Breakdown by view type
- HTML page views: 5735
- PDF downloads: 1374