Prevalence of Significant Pulmonary Diseases in Chinese Adult Patients Presenting with Persistent Cough in Primary Care in Hong Kong-A Pilot Study
Received: 13-Oct-2022 / Manuscript No. JRM-22-77198 / Editor assigned: 17-Oct-2022 / PreQC No. JRM-22-77198 (PQ) / Reviewed: 31-Oct-2022 / QC No. JRM-22-77198 / Revised: 17-Mar-2023 / Manuscript No. JRM-22-77198 (R) / Published Date: 24-Mar-2023
Abstract
Objectives: To evaluate the prevalence of significant pulmonary diseases among Chinese adult patients presenting with persistent cough lasting for 3 weeks or more in primary care in Hong Kong.
Methods: Based on the data generated from the hospital authority clinical data analysis and reporting system, 880 Chinese adult patients who presented with cough as the predominant symptom lasting for 3 weeks or more in two general out-patient clinics in Hong Kong from 1st January 2017 to 31st December 2017 were included in this study. We have evaluated the prevalence of significant pulmonary diseases including lung cancer, non-tuberculosis pneumonia, pulmonary tuberculosis, asthma, bronchiectasis, chronic obstructive pulmonary disease and interstitial lung diseases among the subjects. The proportions of positive pulmonary investigation findings arranged in the study sites and the associated factors for significant pulmonary diseases were also analysed.
Results: The prevalence of significant pulmonary diseases among the studied subjects was 19.2% (169/880). The proportions of positive investigation findings among those with investigations done were 32.0%, 24.7%, 6.2% and 36.7% for chest radiograph, sputum for bacterial culture, sputum for acid-fast bacilli culture and spirometry respectively. The presence of red flag symptoms (OR 3.01, p<0.001), history of other chronic lung diseases (OR 6.82, p<0.001) and older age (OR 1.02, p=0.010) had strong associations with significant pulmonary diseases.
Conclusion: One fifth of the studied subjects had significant pulmonary diseases. Comprehensive clinical evaluation was warranted in these patients for timely detection and intervention of underlying significant pulmonary diseases.
Keywords: Pulmonary diseases; Subacute cough; Chronic cough; Primary care; Asthma; Chronic obstructive pulmonary disease; Bronchiectasis, Pneumonia; Pulmonary tuberculosis; Lung cancer
Introduction
Cough is one of the commonest complaints encountered by primary care physicians. As reported by the Hong Kong primary care morbidity survey 2007-2008, cough related complaints ranked the first among all the physical episodic complaints in general practice [1]. Chronic cough is one of the most common indications for referral and accounts for 10% of respiratory referrals to secondary care [2]. It had a high global prevalence of 9.6% in general adult populations according to a study in 2015 [3].
Current clinical guidelines define subacute cough as having a cough lasting 3 to 8 weeks while chronic cough using cut off duration of 8 weeks [4-6]. Both pulmonary and non-pulmonary disorders can cause persistent cough. Common pulmonary conditions include asthma, post infectious cough, Chronic Obstructive Pulmonary Disease (COPD) and eosinophilic bronchitis [7-10]. Common non pulmonary causes include upper airway cough syndrome (chronic rhinitis, chronic sinusitis and rhinosinusitis), Gastro Esophageal Reflux Disease (GERD) and cough following use of Angiotensin Converting Enzyme Inhibitors (ACEI). 40% of patients being seen in secondary care were diagnosed to have unexplained chronic cough [11].
Significant pulmonary diseases are pulmonary conditions that are not self-limiting and cause substantial morbidity or even mortality. These include lung cancer; communicable pulmonary conditions namely lower respiratory tract infection and pulmonary tuberculosis, chronic lung diseases including asthma, bronchiectasis, COPD and Interstitial Lung Diseases (ILD) [12].
The prevalence of these conditions in patients presented with subacute or chronic cough is highly variable among different regions. The prevalence of COPD, asthma, bronchiectasis and ILD among adults with chronic cough was 6.5%-26.4%, 12.0%-36.0%, 0.2%-8.0% and 8.0% respectively according to various international studies [13-15]. Lung cancer was shown to be the cause in less than 2% of patients who presented with chronic cough [16]. A Korean survey showed that the prevalence of pulmonary tuberculosis among patients with sub-acute and chronic cough was 4.8% and 8.8% respectively [17]. Studies which evaluated the prevalence of chest infections caused by other microorganisms among patients with chronic cough were lacking.
For the evaluation of patients with subacute cough, the American College of Chest Physicians (ACCP) guidelines recommend to first determine whether it is a post infectious cough (e.g. pneumonia, acute bronchitis or tuberculosis), a new onset or exacerbation of pre-existing conditions (e.g. asthma, chronic bronchitis, upper airway cough syndrome and GERD) or a non-infectious cough. According to the American thoracic society and the Infectious Diseases Society of America (IDSA) guidelines, chest radiography is required as a routine evaluation for the diagnosis of community acquired pneumonia [18]. Although sputum for bacterial culture is optional for patients who are being managed as outpatients, obtaining sputum for culture can optimize the selection of an appropriate antibiotic [19]. For patients presented with chronic cough, both the British Thoracic Society (BTS) and ACCP guidelines suggest chest radiography and spirometry as initial investigations. Sputum smears and cultures for Acid Fast Bacilli (AFB) should be obtained for patients who live in areas with a high prevalence of pulmonary tuberculosis. If the initial investigations are normal, referral to a specialist centre for further evaluations such as bronchoscopy and high resolution computed tomography of the thorax is indicated.
Studies have consistently shown that smoking is the most important risk factor for significant respiratory tract disorders including lung cancer, COPD, pulmonary tuberculosis, pneumonia, ILD and other chronic lung diseases [20-23]. Alcoholism increases the risk of community acquired pneumonia and pulmonary tuberculosis but whether alcohol consumption increases the risk of lung cancer remains controversial [24]. Older age was shown to be a risk factor of significant pulmonary diseases in patients with chronic cough, in particular pneumonia, pulmonary tuberculosis and ILD [25]. Female has increased risk for asthma whereas male gender has increased risk for pulmonary tuberculosis and ILD [26]. Socioeconomic status is inversely related to the risks of developing COPD and pulmonary tuberculosis [27]. Patients with neurological disorders (i.e. stroke, dementia, Parkinson's disease and epilepsy) and chronic lung diseases have increased risk of pneumonia. Other comorbid conditions that weaken the immune system such as diabetes mellitus, chronic kidney and liver diseases and cancer are associated with increased risk of chest infection and pulmonary tuberculosis [28]. A personal history of cancer also raises the possibility of metastatic cancer involving the lung causing persistent cough.
Several red flag respiratory symptoms are well known to have associations with underlying significant pulmonary diseases. Haemoptysis, shortness of breath and weight loss were present in 3%, 15%-17% and 6%-10% of primary care patients diagnosed with lung cancer respectively [29]. Pneumonia caused 10% of hemoptysis while pulmonary tuberculosis accounted for 8% [30]. Shortness of breath was reported in approximately 90% of patients with ILD, 70% with COPD and 31% with asthma [31-33]. Fever, shortness of breath, weight loss and hemoptysis were the presenting complaints of 80.2%, 41.0%, 37.2% and 28.8% of patients who were diagnosed with pulmonary tuberculosis [34].
Sub-acute and chronic cough are largely benign conditions but may also be caused by significant respiratory tract pathologies that must not be missed. To our knowledge, there was no published data regarding the prevalence of significant pulmonary diseases among Chinese adult patients presenting with persistent cough in primary care in our locality.
This study aimed to identify the prevalence of significant pulmonary diseases namely lung cancer, non-tuberculosis pneumonia, pulmonary tuberculosis, asthma, bronchiectasis, COPD and ILD among Chinese adult patients presenting with persistent cough lasting for 3 weeks or more in primary care. The proportions of positive pulmonary investigation findings, including chest radiograph, sputum culture and spirometry arranged in the study sites and the associated risk factors of significant pulmonary diseases would also be analysed. As there were variations among the existing international guidelines while local guidelines for persistent cough were lacking, the results from our study would be useful for revising the evaluation algorithm, optimizing management and quality of care for patients suffering from persistent cough in primary care in Hong Kong.
Materials and Methods
Study design
This was a pilot cross sectional study carried out in two General Out-Patient Clinics (GOPCs) in Hong Kong under hospital authority’s management. The hospital authority is a statutory body that provides public healthcare services to Hong Kong citizens through hospitals, special clinics, general out-patient clinics and community out-reach services. These two GOPCs provided primary care with about 140,000 doctor consultation attendances for a wide spectrum of episodic and chronic diseases annually. All patients attending the GOPCs presented with cough as the sole or predominant symptom lasting for 3 weeks or more attending the study sites from 1st January 2017 to 31st December 2017 would be included. The inclusion and exclusion criteria were summarized as below:
Inclusion criteria
• Patients presented with cough as the sole or predominant symptom lasting for 3 weeks or more attending the study sites from 1 January 2017 to 31 December 2017.
Exclusion criteria
• Patients aged below 18 years old.
• Non-Chinese patients.
• Patients with cough duration less than 3 weeks or not specified.
The International Classification of Primary Care (ICPC), a coding method for primary care encounters, allows for the coding of patient’s reason for encounter, the problems or diagnoses managed and primary care interventions. A list of patients with ICPC code R05 (Cough) fulfilling the inclusion criteria was generated from the hospital authority clinical data analysis and reporting system. Medical records of the consultations related to the cough episode in the study sites and secondary care (if patient had been referred) were reviewed for analysis.
Procedure
Collected variables included age, gender, duration of cough upon first consultation, current smoking and drinking status, socioeconomic status, presence of red flag symptoms including hemoptysis, shortness of breath, fever and weight loss, co-morbidities including history of chronic lung, kidney and liver diseases, diabetes, malignancy and neurological diseases including stroke, dementia, Parkinson's disease and epilepsy. Collected investigation results arranged in the study sites included chest radiograph, sputum culture for bacteria and AFB and spirometry. The identified diagnoses for the cough were classified into non-tuberculosis pneumonia, pulmonary tuberculosis, COPD, asthma, bronchiectasis, ILD, lung cancer, other pulmonary diseases and non-respiratory causes with the diagnoses documented. The identified significant pulmonary diseases would be further categorized into newly diagnosed or exacerbation of underlying chronic lung diseases. For patients with no diagnosis established, their outcomes would also be recorded.
The findings of investigations arranged in both primary and secondary care would be reviewed for the establishment of diagnosis. Non-tuberculosis pneumonia was diagnosed when the clinical or investigations findings were suggestive of chest infection. Patients with chest radiographs showing infective changes along with positive sputum culture for non-tuberculous mycobacteria were also classified as non-tuberculosis pneumonia. Patients with positive sputum culture for mycobacterium tuberculosis were diagnosed with pulmonary tuberculosis. The diagnoses of COPD needed to be confirmed by spirometry whereas bronchiectasis and ILD by computed tomography of the thorax [35,36]. Asthma was diagnosed when patients exhibit respiratory symptoms consistent with asthma combined with confirmative spirometry findings [37]. The diagnosis of lung cancer was established by histopathology or imaging studies in patients who refused invasive investigations.
Positive chest radiography findings were defined as chest radiographs suggestive of any of the following conditions: Active pulmonary tuberculosis, pneumonia, emphysema, bronchiectasis, lung cancer or other new onset lung diseases as reported by the radiologists. Positive sputum culture results were defined as a positive growth of bacteria. Positive spirometry results were those demonstrating an obstructive pattern, defined as post bronchodilator Forced Expiratory Volume in one second (FEV1)/Forced Vital Capacity (FVC) ratio smaller than 0.70 with or without bronchodilator reversibility or a restrictive pattern, defined as FEV1/FVC ratio equals to or greater than 0.70 and FVC less than 80% predicted.
Outcomes
Primary outcome was the prevalence of significant pulmonary diseases including lung cancer, non-tuberculosis pneumonia, pulmonary tuberculosis, asthma, bronchiectasis, chronic obstructive pulmonary disease and interstitial lung diseases among Chinese adult patients presenting with persistent cough lasting 3 weeks or more in the two GOPCs. Secondary outcomes were the proportions of patients with positive pulmonary investigation findings, namely chest radiograph, sputum for bacterial and AFB culture and spirometry arranged in the study sites and the associated factors for significant pulmonary diseases.
Sample size calculation
The prevalence of significant pulmonary diseases among Chinese adult patients with persistent cough in primary care was lacking both locally and internationally. Hence, we opted to employ the data from a multicenter survey published in China in 2013 where the population was ethnically similar to our population though the study was carried out in secondary care. The prevalence of the commonest significant pulmonary disease among patients with chronic cough i.e. asthma with a prevalence of 32.6% was chosen to produce the most conservative sample size. By using a computerized sample size calculator with the assumptions of 5% precision, 32.6% prevalence and infinite population size, the estimated sample size was at least 338 in order to achieve 95% confidence interval. In this study, all eligible patients were included to increase the precision of the estimates and to maximize the chance of detecting statistically significant findings.
Statistical analysis
SPSS (version 21) was used for statistical analysis. Continuous variables would be presented as means ± Standard Deviation (SD) and compared with student’s t-test. Skewed data would be presented in median and compared with Mann-Whitney test. Categorical variables would be presented as percentages and compared with Chi-square test or Fisher’s exact test. Age, gender, smoking, alcoholism, socioeconomic status, history of chronic lung, kidney, liver, neurological diseases, diabetes, malignancy and the presence of red flag symptoms were known associated factors of significant pulmonary diseases according to the literature. These factors were included as independent variables in the logistic regression model for control of confounding effects. A p-value of less than 0.05 would be considered statistically significant.
Results
Study population
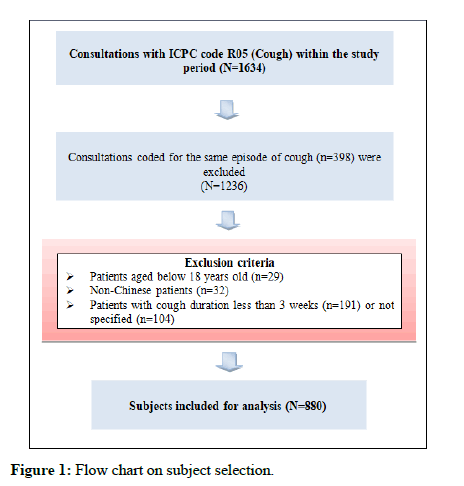
There were 1634 consultations coded with ICPC code R05 (Cough) within the study period. 398 consultations were excluded as they were coded for the same episode of cough. 356 patients were excluded according to the exclusion criteria as shown in Figure 1. A total of 880 patients were included in the final analysis.
The demographic and clinical characteristics of the subjects were shown in Table 1. The mean age of our patients was 61.1 years in which 517 (58.8%) were female. The median duration of cough was 4 weeks. 10.5% and 2.6% of patients were current smokers and chronic drinkers respectively. 14.2% of our patients were receiving comprehensive social security allowance. More than one fifth (22.8%) of patients had red flag symptoms. 9.7% of patients had history of chronic lung diseases in which near half of the patients had asthma (4.5%).
| Mean 61.1 (SD 13.5) | Number (%) | |
|---|---|---|
| Age (years) | ||
| <30 | 26 (2.9) | |
| 30-39 | 37 (4.2) | |
| 40-49 | 82 (9.3) | |
| 50-59 | 227 (25.8) | |
| 60-69 | 297 (33.8) | |
| 70-79 | 139 (15.8) | |
| ≥ 80 | 72 (8.2) | |
| Sex | ||
| Male | 363 (41.2) | |
| Female | 517 (58.8) | |
| Duration of cough (weeks) | Median 4 | |
| 3-7 (sub-acute) | 551 (62.6) | |
| ≥ 8 (chronic) | 329 (37.4) | |
| Smoking status | ||
| Non smoker | 679 (77.2) | |
| Ex-smoker | 106 (12) | |
| Current smoker | 92 (10.5) | |
| Unknown | 3 (0.3) | |
| Drinking status | ||
| Non-drinker | 737 (83.8) | |
| Ex-drinker | 6 (0.7) | |
| Social drinker | 82 (9.3) | |
| Chronic drinker | 23 (2.6) | |
| Unknown | 32 (3.6) | |
| Socioeconomic status | ||
| Not on CSSA | 752 (85.5) | |
| On CSSA | 125 (14.2) | |
| Unknown | 3 (0.3) | |
| Presence of red flag symptoms | ||
| Yes | 201 (22.8) | |
| Haemoptysis | 60 (6.8) | |
| Shortness of breath | 80 (9.1) | |
| Fever | 51 (5.8) | |
| Weight loss | 37 (4.2) | |
| No | 674 (76.6) | |
| Not documented | 5 (0.6) | |
| History of chronic lung disease | ||
| Yes | 85 (9.7) | |
| Asthma | 40 (4.6) | |
| Bronchiectasis | 13 (1.5) | |
| COPD | 8 (0.9) | |
| Lung cancer | 3 (0.3) | |
| ILD (Pneumoconiosis) | 1 (0.1) | |
| Pulmonary fibrosis | 2 (0.2) | |
| Pulmonary tuberculosis | 18 (2.1) | |
| No | 795 (0.3) | |
| History of chronic kidney disease | ||
| Yes | 51 (5.8) | |
| No | 829 (94.2) | |
| History of chronic liver disease | ||
| Yes | 48 (5.5) | |
| No | 832 (94.5) | |
| History of diabetes | ||
| Yes | 138 (15.7) | |
| No | 742 (84.3) | |
| History of malignancy | ||
| Yes | 60 (6.8) | |
| No | 820 (93.2) | |
| History of neurological disease | ||
| Yes | 39 (4.4) | |
| No | 841 (95.6) | |
| Note: CSSA: Comprehensive Social Security Allowance, COPD: Chronic Obstructive Pulmonary Disease, ILD: Interstitial Lung Diseases | ||
Table 1: Demographic data and clinical characteristics of patients (N=880).
Prevalence of significant pulmonary diseases and other conditions
169 (19.2%) patients with persistent cough lasting 3 weeks or more were found to have significant pulmonary diseases in which 16.1% were newly diagnosed. The majority of patients were diagnosed with non-tuberculosis pneumonia (10.8%). The prevalence of asthma, bronchiectasis, COPD and ILD (pneumoconiosis) was 3.3%, 2.2%, 1.9% and 0.1% respectively. 0.3% of our patients were confirmed to have pulmonary tuberculosis and 0.6% was diagnosed to have lung cancer (Table 2).
About one fourth (22.2%) of patients was clinically diagnosed to have other pulmonary diseases in which most of them were diagnosed with bronchitis (12.3%) followed by post viral cough (6.5%). 2.4% had abnormal chest radiograph undergoing work up in secondary care. Non respiratory causes were clinically diagnosed in 15.9% patients and most of them were diagnosed with allergic rhinitis with post nasal drip (9.8%). 42.7% (376) of patients had no diagnosis established in which majority (32.0%) had their cough subsided during the review period.
| Diagnosis | No. of patients (%) |
|---|---|
| Significant pulmonary diseases Newly diagnosed significant pulmonary diseases |
169 (19.2) 142 (16.1) |
| Non tuberculosis pneumonia | 95 (10.8) |
| COPD | 16 (1.8) |
| Bronchiectasis | 12 (1.4) |
| Asthma | 11 (1.2) |
| Lung cancer | 5 (0.6) |
| Pulmonary tuberculosis | 3 (0.3) |
| Exacerbation of underlying chronic lung diseases | 27 (3.1) |
| Asthma | 18 (2.1) |
| Bronchiectasis | 7 (0.8) |
| COPD | 1 (0.1) |
| ILD (Pneumoconiosis) | 1 (0.1) |
| Other pulmonary diseases | 195 (22.2) |
| Bronchitis | 108 (12.3) |
| Post viral cough | 57 (6.5) |
| Allergic airways | 4 (0.5) |
| Post pneumonia cough | 3 (0.3) |
| Smoker’s cough | 2 (0.2) |
| Lung opacity on chest radiograph# | 14 (1.6) |
| Lung nodule on chest radiograph# | 5 (0.6) |
| Pleural effusion# | 2 (0.2) |
| Non respiratory causes | 140 (15.9) |
| Allergic rhinitis with post-nasal drip | 86 (9.8) |
| ACEI induced cough | 37 (4.2) |
| Gastro esophageal reflux syndrome | 12 (1.3) |
| Congestive heart failure | 5 (0.6) |
| No cause established | 376 (42.7) |
| Patients with cough subsided | 282 (32.0) |
| Patients lost to follow up | 53 (6.0) |
| Patients with normal initial investigation and pending assessment by secondary care | 40 (4.6) |
| Patient with persistent cough but refused workup | 1 (0.1) |
| Note: #Abnormalities undergoing work up in secondary care, COPD: Chronic Obstructive Pulmonary Disease, ILD: Interstitial Lung Diseases, ACEI: Angiotensin Converting Enzyme Inhibitors | |
Table 2: Prevalence of significant pulmonary diseases and other conditions (N=880).
Proportion of patients with positive pulmonary investigation findings
Chest radiograph, sputum for bacterial culture, sputum for AFB culture and spirometry were arranged in the study sites and performed in 596 (67.7%), 377 (42.8%), 354 (40.2%) and 30 (3.4%) patients respectively. Among the patients with the respective investigations performed, 32.0% had positive findings of new onset lung diseases in chest radiograph, 24.7% and 6.2% had positive sputum bacterial and AFB culture and 36.7% had abnormal spirometry results (Table 3).
| Investigations | No. of patients (%) |
|---|---|
| Chest radiograph (N=596) | |
| Positive | 191 (32) |
| Infective changes | 84 (14.1) |
| Lung opacities | 37 (6.2) |
| Bronchitic changes | 34 (5.7) |
| Hyperinflated lungs | 14 (2.4) |
| Bronchiectatic changes | 8 (1.3) |
| Lung nodule(s) | 8 (1.3) |
| Lung mass | 3 (0.5) |
| Pleural effusion | 3 (0.5) |
| Negative | 405 (68) |
| Sputum bacterial culture (N=377) | |
| Positive (sub group with culture results)* | 93 (24.7) |
| Haemophilus influenzae | 47 (12.5) |
| Staphylococcus aureus | 17 (4.5) |
| Pseudomonas aeruginosa | 17 (4.5) |
| Moraxella catarrhalis | 13 (3.4) |
| Klebsiella pneumoniae | 8 (2.1) |
| Streptococcus pneumoniae | 7 (1.9) |
| Negative | 284 (75.3) |
| Sputum AFB culture (N=354) | |
| Positive | 22 (6.2) |
| Mycobacterium tuberculosis | 3 (0.8) |
| Non-tuberculous mycobacteria | 19 (5.4) |
| Negative | 332 (93.8) |
| Spirometry (N=30) | |
| Positive | 11 (36.7) |
| FEV1/FVC <0.70 without bronchodilator reversibility | 9 (30) |
| FEV1/FVC <0.70 with bronchodilator reversibility | 2 (6.7) |
| FEV1/FVC ≥ 0.70, FVC <80% predicted | 0 (0) |
| Negative (FEV1/FVC ≥ 0.70, FVC >80% predicted) | 19 (63.3) |
| Note: *16 patients had positive culture for 2 organisms, AFB: Acid Fast Bacilli, FEV1: Forced Expiratory Volume in One Second, FVC: Forced Vital Capacity | |
Table 3: Proportion of patients with positive pulmonary investigation findings.
Factors associated with significant pulmonary diseases
846 patients with no missing demographic or clinical data were included for analysis of factors associated with significant pulmonary diseases in the logistic regression.
The results revealed that the presence of red flag symptoms (OR 3.01, p<0.001), a history of other chronic lung diseases (OR 6.82, p<0.001) and older age (OR 1.02, p=0.010) had strong associations with significant pulmonary diseases (Table 4).
| Associated factors | OR | 95% CI | P value |
|---|---|---|---|
| Age | 1.02 | 1.01-1.04 | 0.010* |
| Male | 0.85 | 0.55-1.32 | 0.477 |
| Duration of cough | 1.00 | 1.00-1.01 | 0.457 |
| Smoking status | |||
| Ex-smoker | 1.12 | 0.65-2.39 | 0.514 |
| Current smoker | 1.78 | 0.91-3.35 | 0.093 |
| Drinking status | |||
| Social drinker | 0.93 | 0.46-1.91 | 0.852 |
| Chronic drinker | 2.55 | 0.92-7.12 | 0.074 |
| Socioeconomic status | |||
| On CSSA | 1.56 | 0.93-2.60 | 0.092 |
| Presence of red flag symptoms | 3.01 | 2.01-4.50 | <0.001* |
| History of chronic lung disease | 6.82 | 4.02-11.58 | <0.001* |
| History of chronic kidney disease | 1.28 | 0.60-2.76 | 0.527 |
| History of chronic liver disease | 1.33 | 0.61-2.92 | 0.479 |
| History of diabetes | 0.99 | 0.59-1.67 | 0.980 |
| History of malignancy | 0.97 | 0.46-2.04 | 0.925 |
| History of neurological disease | 0.75 | 0.31-1.81 | 0.520 |
| Note: OR: Odd Ratio; CI: Confidence Interval; CSSA: Comprehensive Social Security Assistance | |||
Table 4: Factors associated with significant pulmonary diseases (N=846).
Discussion
In our study, almost one fifth (19.2%) of patients presented with persistent cough lasting for 3 weeks or more had significant pulmonary diseases. The high prevalence of chest infection (10.8%) among our patients demonstrated that it is an important diagnosis to be considered in evaluation of patients with persistent cough in primary care. Our results showed comparable prevalence of bronchiectasis (2.2% vs. 0.2%-8.0%) and lung cancer (0.6% vs. ≤ 2%) to the other studies conducted in China and the United States. However, when compared with other international studies, our study reported a much lower prevalence of COPD (1.9% vs. 6.5%-26.4%), asthma (3.3% vs. 12.0%-36.0%), pulmonary tuberculosis (0.3% vs. 6.8%) and ILD (0.1% vs. 8.0%). This could be explained by the difference in study population where the results from former studies were generated from data retrieved from secondary care. Besides, compared to the former studies which had higher prevalence of current smokers (23.9%-48.2%) and ex-smokers (15.1%-36.1%), our study population had a lower prevalence of current smokers (10.5%) and ex-smokers (12.0%). Furthermore, studies that reported high prevalence of asthma and COPD were carried out in countries, namely China, Sudan and Korea which might have higher air pollution levels caused by heavy industries compared to Hong Kong. These would also contribute to the difference in prevalence of the above mentioned significant pulmonary diseases between our study and former studies. 42.7% of our patients had no diagnosis established for the persistent cough lasting 3 weeks or more which was comparable to the previous findings of 40% of chronic cough patients with unexplained cause.
About one third of patients who had investigations performed had positive findings for chest radiography (32.0%) and spirometry (36.7%). This supported the recommendations by international guidelines that chest radiography and spirometry should be arranged as initial investigations for patients with sub-acute or chronic cough. It might be worthwhile to mention that the reason for the small proportion of our patients (3.4%) undergoing spirometry was that this investigation was ordered solely for patients with persistent shortness of breath after active infection was excluded and some patients with mild symptoms might not attend our clinic for follow up after the active infection was treated. Moreover, some patients who fit into these criteria were already known to have asthma or COPD; hence, spirometry was not rearranged. The proportion of patients with positive sputum bacterial and AFB culture was 24.7% and 6.2% respectively among patients with sputum saved. 10.6% (93/880) of all patients with persistent cough had positive sputum bacterial culture results. This implied that the test was warranted as a positive result together with the sensitivity test could guide physicians for appropriate antibiotic treatment. Although a relatively smaller proportion (2.5%) of all patients with persistent cough had positive AFB culture results, early diagnosis of Mycobacterium tuberculosis and non-tuberculous mycobacteria is crucial as they could both cause significant morbidity and mortality with the former being highly contagious. This supported the need of performing the test for patients with persistent cough in our locality. 6.0% and 0.1% of all patients were lost to follow up and refused workup respectively; this might result in an underestimationn of the proportion of positive investigation results and prevalence of significant pulmonary diseases.
In keeping with the findings of various studies, older age, a history of chronic lung diseases and the presence of red flag symptoms were significantly associated with significant pulmonary diseases. Thus, particular attention should be paid with the presence of the above clinical history during the evaluation of patients with persistent cough. Other factors including smoking, alcoholism, gender, socioeconomic status, history of neurological disease, diabetes mellitus, chronic kidney disease, chronic liver disease and malignancy were not found to be associated with significant pulmonary diseases as compared with other studies. This could be attributed to the fact that only a small number of our patients were smokers, drinkers or had a history of the above chronic diseases and therefore a significant association could not be generated in the analysis. Different gender was observed to have increased risks of different significant pulmonary diseases in former studies. This could explain the discrepancy when compared with our results as our study analysed significant pulmonary diseases collectively. The differences in living standard and general health status of the CSSA and non-CSSA recipients might not solely depend on whether the patients were receiving CSSA due to current financial adversity but also other socioeconomic factors which were not retrievable in this retrospective study. Besides, the majority of our diabetic patients had good diabetic control; they might not be more prone to significant infectious pulmonary diseases which were caused by weakened immunity.
Our study was the first study to show the prevalence of significant pulmonary diseases in Chinese adult patients presenting with persistent cough in primary care in Hong Kong. We have demonstrated that about one fifth of patients with persistent cough had significant pulmonary diseases. Our data also showed that a considerable proportion of patients who had undergone chest radiography, spirometry and sputum bacterial culture had positive findings. Although the number of patients with positive AFB sputum culture might seem small, it should still be obtained for patients with persistent cough in our locality as there was a high prevalence of pulmonary tuberculosis in Hong Kong. At present, doctors might be following different international guidelines on the management of persistent cough as there were no clear local guidelines available. Our study findings provide evidence based guidance on the diagnostic approach to the management of patients with persistent cough. We recommend that chest radiography, sputum for bacterial and AFB culture should be done for all patients with persistent cough lasting for 3 weeks or more after exclusion of non-respiratory causes while spirometry should be arranged early after active pulmonary infection is excluded.
Limitations
There were several limitations in this study. Firstly, some patients who presented with persistent cough lasting for 3 weeks or more might not be coded with ICPC code R05 and hence were not included in our retrospective study. Besides, a minute number of patients (0.6%) did not have red flag symptoms documented in the consultation notes which could lead to misclassification bias. Prospective study with implementation of standardized protocols for data collection would have the advantage of minimizing potential sources of bias. Secondly, subjects were recruited from two GOPCs in a local district which limited the generalizability of our results to the whole population of Hong Kong. Thirdly, a small number of patients were lost to follow up (6%) or refused investigations (0.1%) despite clinically indicated. Therefore, the proportion of positive investigation results and prevalence of significant pulmonary diseases might be underestimated. As mentioned in the discussion section, the diagnosis of chronic lung diseases might also be underestimated as some patients with active lung infection treated might not attend our clinics again to follow up for mild chronic lung symptoms. Finally, the sample sizes of some of the associated factors might be too small to generate a significant association in our analysis. Further studies with larger sample size are required to arrive at more precise estimates [36,37].
Conclusion
Our study demonstrated that about one fifth of patients presented with persistent cough lasting for 3 weeks or more had significant pulmonary diseases in primary care. Significant proportions of patients had positive initial investigation findings. The presence of red flag symptoms, having a history of other chronic lung diseases and being older were significant associated factors. This illustrated that comprehensive clinical evaluation including detailed history, chest radiograph, sputum bacterial and AFB culture and spirometry was warranted in these patients for timely detection and intervention of underlying significant pulmonary diseases.
Acknowledgement
We would like to thank Dr. Chow Kai Lim for performing the statistical analyses and providing the data sets.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not for profit sectors.
References
- Lo YYC, Lam CLK, Lam TP (2010) Hong Kong primary care morbidity survey 2007–2008. The Hong Kong Practitioner 32: 17-26.
- Morice AH, McGarvey L, Pavord I (2006) Recommendations for the management of cough in adults. Thorax 61: i1-i24.
[Crossref] [Google Scholar] [PubMed]
- Song WJ, Chang YS, Faruqi S, Kim JY, Kang MG, et al. (2015) The global epidemiology of chronic cough in adults: a systematic review and meta-analysis. Eur Respir J 45: 1479-1481.
[Crossref] [Google Scholar] [PubMed]
- Morice AH (2004) The diagnosis and management of chronic cough. Eur Respir J 24: 481-492.
[Crossref] [Google Scholar] [PubMed]
- Irwin RS, Baumann MH, Bolser DC, Boulet LP, Braman SS, et al. (2006) Diagnosis and management of cough executive summary. Chest 129: 1S-23S.
[Crossref] [Google Scholar] [PubMed]
- Gibson PG, Chang AB, Glasgow NJ, Holmes PW, Katelaris P, et al. (2010) CICADA: Cough in children and adults: Diagnosis and assessment. Australian Cough Guidelines summary statement. Med J Aust 192: 265-271.
[Crossref] [Google Scholar] [PubMed]
- Terasaki G, Paauw DS (2014) Evaluation and treatment of chronic cough. Med Clin North Am 98: 391–403.
[Crossref] [Google Scholar] [PubMed]
- Koo HK, Jeong I, Lee SW, Park J, Kim JH, et al. (2016) Prevalence of chronic cough and possible causes in the general population based on the Korean national health and nutrition examination survey. Medicine 95: e4595.
[Crossref] [Google Scholar] [PubMed]
- Lai K, Chen R, Lin J, Huang K, Shen H, et al. (2013) A Prospective, multicenter survey on causes of chronic cough in China. Chest 143: 613–620.
[Crossref] [Google Scholar] [PubMed]
- Tey F (2016) Chronic Cough: Common causes in sudanese young adults. J Lung Pulm Respir Res 3: 79-80.
- Yousaf N, Montinero W, Birring SS, Pavord ID (2013) The long term outcome of patients with unexplained chronic cough. Respir Med 107: 408–412.
[Crossref] [Google Scholar] [PubMed]
- Ferkol T, Schraufnagel D (2014) The global burden of respiratory disease. Ann Am Thorac Soc 11: 404-406.
[Crossref] [Google Scholar] [PubMed]
- Kaushik N, Smith J, Linehan M, Frank T (2015) Prevalence of chronic cough in a population based survey. Eur Respir J 46: 1139.
[Crossref]
- Rosen MJ (2006) Chronic cough due to bronchiectasis: ACCP evidence based clinical practice guidelines. Chest 129: 122S-131S.
[Crossref] [Google Scholar] [PubMed]
- Chung KF, Pavord ID (2008) Prevalence, pathogenesis, and causes of chronic cough. Lancet 371: 1364-1374.
[Crossref] [Google Scholar] [PubMed]
- Kvale PA (2006) Chronic cough due to lung tumors: ACCP evidence based clinical practice guidelines. Chest 129: 147S-153S.
[Crossref] [Google Scholar] [PubMed]
- Kang MG, Song WJ, Kim HJ, Won HK, Sohn KH, et al. (2017) Point prevalence and epidemiological characteristics of chronic cough in the general adult population. Medicine 96: e6486.
[Crossref] [Google Scholar] [PubMed]
- Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, et al. (2007) Infectious diseases society of America/American thoracic society consensus guidelines on the management of community acquired pneumonia in adults. Clin Infect Dis 44: S27-S72.
[Crossref] [Google Scholar] [PubMed]
- Bhattacharya A (2006) Role of sputum cultures in diagnosis of respiratory tract infections. Lung India 23: 20-24.
- Vogelmeier CF, Criner GJ, Martinez FJ, Anzueto A, Barnes PJ, et al. (2017) Global strategy for the diagnosis, management and prevention of chronic obstructive lung disease 2017 report: GOLD executive summary. Respirology 22: 575-601.
[Crossref] [Google Scholar] [PubMed]
- Mijiti P, Yuehua L, Feng X, Milligan PJ, Merle C, et al. (2016) Prevalence of pulmonary tuberculosis in western China in 2010-11: A population based, cross-sectional survey. Lancet Glob Health 4: e485–e494.
[Crossref] [Google Scholar] [PubMed]
- Torres A, Peetermans WE, Viegi G, Blasi F (2013) Risk factors for community-acquired pneumonia in adults in Europe: A literature review. Thorax 68: 1057–1065.
[Crossref] [Google Scholar] [PubMed]
- Choi WI, Dauti S, Kim HJ, Park SH, Park JS, et al. (2018) Risk factors for interstitial lung disease: A 9 year Nationwide population based study. BMC Pulm Med 18: 96.
[Crossref] [Google Scholar] [PubMed]
- Djousse L, Dorgan JF, Zhang Y, Schatzkin A, Hood M, et al. (2002) Alcohol consumption and risk of lung cancer: The framingham study. J Natl Cancer Inst 94: 1877–1882.
[Crossref] [Google Scholar] [PubMed]
- Morice AH, Jakes AD, Faruqi S, Birring SS, McGarvey L, et al. (2014) A worldwide survey of chronic cough: A manifestation of enhanced somatosensory response. Eur Respir J 44: 1149–1155.
[Crossref] [Google Scholar] [PubMed]
- Fuseini H, Newcomb DC (2017) Mechanisms driving gender differences in asthma. Curr Allergy Asthma Rep 17: 19.
[Crossref] [Google Scholar] [PubMed]
- Mannino DM, Buist AS (2007) Global burden of COPD: Risk factors, prevalence and future trends. Lancet 370: 765-773.
[Crossref] [Google Scholar] [PubMed]
- Tuberculosis Risk Factors (2016) Centre for Disease Control and Prevention.
- Hamilton W, Sharp D (2004) Diagnosis of lung cancer in primary care: A structured review. Fam Pract 21: 605-611.
[Crossref] [Google Scholar] [PubMed]
- Bidwell JL, Pachner RW (2005) Hemoptysis: Diagnosis and management. Am Fam Physician 72: 1253-1260.
[Google Scholar] [PubMed]
- Singh D, Miravitlles M, Vogelmeier C (2017) Chronic obstructive pulmonary disease individualized therapy: Tailored approach to symptom management. Adv Ther 34: 281-299.
[Crossref] [Google Scholar] [PubMed]
- Ding B, Small M (2017) Disease burden of mild asthma: Findings from a cross sectional real world survey. Adv Ther 34: 1109-1127.
[Crossref] [Google Scholar] [PubMed]
- Collard HR, Pantilat SZ (2008) Dyspnea in interstitial lung disease. Curr Opin Support Palliat Care 2: 100-104.
[Crossref] [Google Scholar] [PubMed]
- Sahoo U, Singh SK, Basa S, Mohan U (2015) A study of the epidemiological pattern of pulmonary tuberculosis patients undergoing treatment at tuberculosis units of Lucknow. Asian J Biomed Pharm Sci 5:19-23.
- Hill AT, Sullivan AL, Chalmers JD, De Soyza A, Elborn JS, et al. (2018) British thoracic society guideline for bronchiectasis in adults. BMJ Open Respir Res 5: e000348.
[Crossref] [Google Scholar] [PubMed]
- Wells AU, Hirani N (2008) Interstitial lung disease guideline. Thorax 63: v1-v58.
- Bateman ED, Hurd SS, Barnes PJ, Bousquet J, Drazen JM, et al. (2008) Global strategy for asthma management and prevention: GINA executive summary. Eur Respir J 31: 143-178.
[Crossref] [Google Scholar] [PubMed]
Citation: Wong HKQ, Chan PF, Lai KPL (2023) Prevalence of Significant Pulmonary Diseases in Chinese Adult Patients Presenting with Persistent Cough in Primary Care in Hong Kong; A Pilot Study. J Respir Med 05: 155
Copyright: © 2023 Wong HKQ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 374
- [From(publication date): 0-0 - Jul 16, 2025]
- Breakdown by view type
- HTML page views: 181
- PDF downloads: 193