Psychosocial Differences between Children’s Weight Groups
Received: 22-Aug-2018 / Accepted Date: 21-Sep-2018 / Published Date: 28-Sep-2018 DOI: 10.4172/2165-7904.1000374
Keywords: Childhood obesity; Psychosocial; Depression; Motivation; Self-efficacy; Parent-childrelationship
Background
Childhood obesity in Israel is among the highest in western society. Official data published by the Israeli Ministry of Health in 2013 indicated that 30.7% of fifth grade children are overweight or obese (BMI percentile ≥ 85). Moreover, 13.3% of the children are considered morbidly obese (BMI percentile ≥ 97) [1]. The consequences of obesity are not only medical; and many obese children are troubled by psychosocial issues.
There is no consensus among researchers regarding the existence of psychosocial difficulties and their impact among overweight and obese children [2]. Several studies have found a variety of emotional difficulties such as low self-esteem, depression, anxiety and social problems [3-7].
In adults, the prevalence of depression is higher among obese [8], with women having higher rates of depression than men [9]. Only in the last 20 years’ experts started to recognize the presence of depression in children [10]. Obese children have more depressive symptoms compared to their normal weight peers [7,11,12]. Few studies pointed that obese, especially morbid obese female adolescents are at higher risk for depression [13-15]. Moreover, the overall quality of life (QoL) of overweight children was found to be lower compared to normal weight peers [15].
The two main factors that motivate obese adults to lose weight are the understanding of health risks associated with obesity and the dissatisfaction from their appearance [16,17]. The motivating reasons for weight loss in children are not well established. Physical activity is an important part of obesity treatment and prevention programs, it is interesting that adults and children demonstrate different motivating reasons toward physical activity; in adults, the motivators will generally be health related or improvement of body appearance while children are motivated to participate in physical activity mainly by social issues such as fun and enjoyment [18].
In the first years of life, parents and families are the most influential social environmental factor. Probably, behaviors such as eating, engagement in physical activity and sedentarism are closely related to the parents’ actions and beliefs [19-21]. Adolescence is a challenging period in parent-child relationship, characterized by less emotional closeness and more confrontations and arguments [22]. Lack of communication between parents and their adolescent child is known to be related to risky behaviors, suicidal behaviors, as well as to abnormal body weight, depression and low self-esteem [23]. Few studies reported higher rates of conflicts between overweight children (mainly male adolescents) and their parents, compared to normal weight peers [24], especially at and about meals [25].
Current reported research on the psychosocial consequences of childhood obesity includes mainly children participating in treatment programs for childhood obesity. This selection bias led some investigators to argue that the reported characteristics are unique to treated obese children only, although several studies found no differences between treated and non-treated obese children [11,14]. Psychosocial difficulties are inseparable from the period of adolescence, but these difficulties among overweight children may appear at a relatively very early age. Kindergarten children describe their overweight peers as lazy, unattractive, and sad and find them undesirable for play [26]. It seems that the negative esteem of children to the overweight child relates to the visually of obesity, as opposed to other chronic diseases where the disease has no effect on the child's appearance (e.g. asthma). Moreover, obesity is regarded to be a "controlled" situation, where the child is blamed for being obese unlike other chronic diseases or disabilities [27].
The purpose of the current study was to assess the prevalence of depressive symptoms, self-efficacy, and relationship with the parents and motivation for weight loss, among children of different weight groups.
Methods
One hundred and fifty-two children, ages 9-18 years old, participated in the study. The study population was recruited from the pediatric endocrinology clinic and the child health and sport center at Meir Medical Center, Kfar-Saba, Israel. Children with obesity due to a disease, medication use and children who were unable or unwilling to fill the questionnaires were excluded from the study.
The study was approved by the institutional review board of the Meir Medical Center and by the ethics committee of Bar-Ilan University. All children and their parents singed informed consent forms prior to their participation.
Anthropometrics
Standard, calibrated scales and stadiometers were used to determine height, weight, and BMI. As BMI changes with age, we calculated the BMI percentile (BMI percentile) for each child using the standards from the Centers for Disease Control, National Center for Health Statistics [28]. Subjects were divided to three weight groups according to their BMI percentiles: Normal weight (BMI percentiles>5<85), overweight and obese children (BMI percentiles≥ 85<97) and morbid obese children (BMI percentiles ≥ 97). Mean age of all participants was 12.25 ± 2.20 years with no age differences between the groups.
Sexual maturity (Tanner stage) among the overweight, obese and morbid obese children was evaluated by a trained pediatric endocrinologist. Normal weight children self-reported their Tanner stage using a validated questionnaire [29].
Study questionnaires
The participants were asked to complete four questioners: Symptoms of depression, self-efficacy, motivation and relationship with the parents.
Depression: The depression questionnaire, Child Depression Inventory (CDI) [30], is based on self-reporting which measures the level of symptoms of depression amongst children and youth and includes 27 items affecting four fields: Emotional, cognitive, motivational and somatic.
Motivation: The motivation for weight loss scale is a validated, 24 items, questionnaire assessing overweight and obese individuals' reasons for weight loss [31]. The motivation variable contained two indexes: Health and appearance. The questionnaire was developed for adults and adjusted for children.
Self-efficacy: The self-efficacy questionnaire regarding physical activity is a validated scale used to measure psychosocial determinants of physical activity in children [32]. The scale was adjusted so that selfefficacy will relate to the ability to persevere a healthy and active lifestyle.
Parent-child relationship: The Relationship with Father/Mother Questionnaire (RFMQ) [33] was assessed for each parent separately. The questionnaire evaluates the relationship between a child and his parents and included two indexes: Supervision and rejectionconfrontation. The questionnaire uses a scale of 1-5 when higher score represents higher supervision and more rejection-confrontation. Parents were asked to fill demographic and familial questionnaires. Leisure time physical activity was assessed using the Godin Leisure- Time Exercise Questionnaire [34].
Statistical Analysis
A two-way repeated measure ANOVA with Bonferroni corrections was used for a single variable analysis and MANOVA for multiple variable analysis and gender differences. A linear (Pearson) and nonlinear regression and correlation tests were performed between the study variables and BMI percentile. Statistical significance was set at p<0.05. Data are presented as mean ± SD.
Results
One hundred and fifty-two children, ages 9-18 years old, participated in the study. Anthropometric measures are presented in Table 1. Significant between group differences were found, as expected, only in weight related factors (Weight, BMI).
| Parameters | Normal weight (n=46) | Overweight and obese (n=55) | Morbid obese (n=51) | F(2, 149) | Eta² |
|---|---|---|---|---|---|
| Age (Years) | 12.65 ± 2.41 | 12.56 ± 2.54 | 11.90 ± 1.88 | NS | -- |
| Weight (kg) | 43.64 ± 11.95 | 56.17 ± 13.55 | 73.32 ± 20.92 | 42.17*** | 0.36 |
| Height (cm) | 153.98 ± 12.73 | 150.21 ± 11.87 | 151.46 ± 9.30 | 1.41 | 0.02 |
| BMI (kg/m²) | 18.04 ± 2.28 | 24.54 ± 2.59 | 31.50 ± 5.78 | 144.44*** | 0.66 |
| Maturity level (Tanner stage) | 2.78 ± 1.55 | 2.67 ± 1.45 | 2.69 ± 1.57 | 0.07 | 0 |
| Birth-weight (kg) | 3.18 ± 0.42 | 3.19 ± 0.57 | 3.23 ± 0.66 | 0.11 | 0 |
| Weeks of pregnancy | 39.35 ± 1.55 | 39.18 ± 1.94 | 38.93 ± 2.34 | 0.54 | 0.01 |
Table 1: Anthropometric measurements of the study groups where ***p<0.001.
A statistically significant non-linear relationship was found between birth weight and future child BMI percentile, β=0.22, p<0.05. Small, or large babies, with birth weight <2.5 kg and >3.5 kg, were found to have higher future BMI percentile. This relationship was most significant in the morbid obese group, β=0.34, p<0.05.
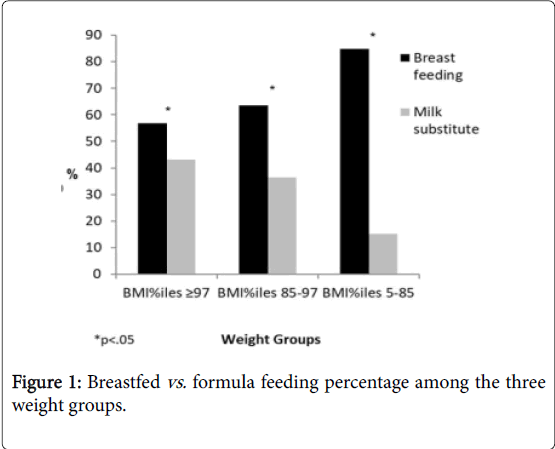
Patient and familial characteristics are presented in Table 2. Significant between groups differences were found in father, mother and sibling overweight, and in the way the child was fed as a baby: 84.8% of the normal weight group were breastfed (>10 weeks exclusive breastfeeding) compared to only 56.9% in the morbid obese group.
| Characteristics | Factors | Normal weight | Overweight & obese | Morbid obese | X2 | |||
|---|---|---|---|---|---|---|---|---|
| -- | N | % | N | % | N | % | ||
| Gender | Male | 24 | 52.2 | 21 | 38.2 | 24 | 47.1 | 2.06 |
| Female | 22 | 47.8 | 34 | 61.8 | 27 | 52.9 | ||
| Child order | Firstborn | 17 | 37 | 23 | 47.9 | 15 | 33.3 | 2.26 |
| Not firstborn | 29 | 63 | 25 | 52.1 | 30 | 66.7 | ||
| Marital status | Married | 44 | 95.7 | 46 | 85.2 | 42 | 82.4 | 4.27 |
| Not married | 2 | 4.3 | 8 | 14.8 | 9 | 17.6 | ||
| Familial overweight | ||||||||
| Father | No | 33 | 71.7 | 24 | 43.6 | 13 | 25.5 | 21.02*** |
| Yes | 13 | 28.3 | 31 | 56.4 | 38 | 74.5 | -- | |
| Mother | No | 34 | 73.9 | 27 | 49.1 | 18 | 35.3 | 14.74*** |
| Yes | 12 | 26.1 | 28 | 50.9 | 33 | 64.7 | -- | |
| Siblings | No | 44 | 95.7 | 32 | 65.3 | 20 | 44.4 | 28.05*** |
| Yes | 2 | 4.3 | 17 | 34.7 | 25 | 55.6 | -- | |
| Feeding in infancy | Breastfed | 39 | 84.8 | 35 | 63.6 | 29 | 56.9 | 9.30* |
| Formula | 7 | 15.2 | 20 | 36.4 | 22 | 43.1 | -- | |
Table 2: Patient and familial characteristics (*p<0.05, **p<0.01, ***p<0.001).
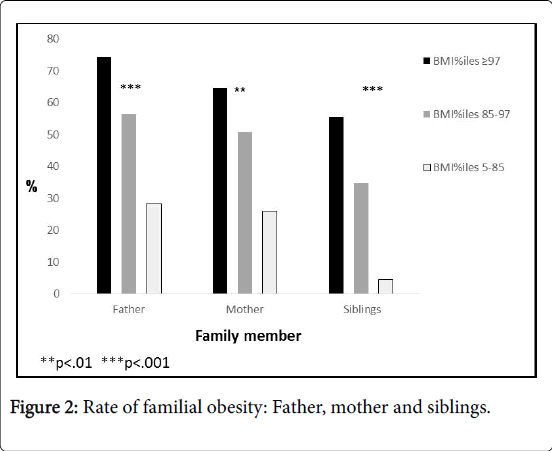
The percent of overweight parents/siblings increased with the child's weight status. In the morbid obesity group, the highest percentage of overweight fathers (74.5%), mothers (64.7%) and siblings (55.6%), was found.
We found a statistically significant between weight group difference in the number of “good friends” as reported by the parents, F (2,120)=3.96, p<.05, Eta²=0.06. The morbid obese group had the lowest number of good friends (4.93 ± 2.98) compared to normal weight (6.55 ± 3.25). Bonferroni analysis indicated that this difference was statistically significant between the morbid obese group and both the normal and overweight groups.
Leisure time physical activity was statically different between the groups, F (2, 120)=13.40, p<0.001, Eta²=0.183. Normal weight children were more active, with an average of 3.95 ± 2.19 active days/week. This amount decreased as the weight status increased, with average of 2.41 ± 1.53 active days/week at the overweight children and only 2.09 ± 1.36 active days/week in the morbid obese children.
Parent-Child Relationship
Parent-child relationship indexes are presented in Table 3. We found significant differences in father and mother supervision, p<0.05, and father rejection-confrontation, p<0.01, with increasing score as the weight degree was higher. In a two-way repeated Bonferroni measures we found statistically significant differences only between the normal weight and morbid obesity weight, p<0.01. Although boys' average score was higher than the girls' average score in all the indexes, no significant interaction of gender X weight groups was found, F (8,286)=0.30, p>0.05 (Figures 1 and 2).
| Parameters | Normal weight | Overweight and obese | Morbid obese | Calculation | ||||
|---|---|---|---|---|---|---|---|---|
| Indexes | M | SD | M | SD | M | SD | F(8,292) | Eta² |
| Supervision | ||||||||
| Mother | 2.04 | 0.59 | 2.32 | 0.84 | 2.51 | 1.71 | 4.35* | 0.05 |
| Father | 2.16 | 0.57 | 2.27 | 0.68 | 2.51 | 0.84 | 3.46* | 0.04 |
| Rejection-confrontation | ||||||||
| Mother | 1.54 | 0.63 | 1.57 | 0.75 | 1.69 | 0.72 | 0.63 | 0.01 |
| Father | 1.53 | 0.39 | 1.55 | 0.49 | 1.84 | 0.72 | 5.03** | 0.06 |
Table 3: Parent-child relationship indexes (*p<0.05, **p<0.01).
Interestingly, we found a significant difference in the child-parent relationship based on the way the child was fed as a baby. Maternal rejection-confrontation index was significantly lower in breastfed infants (1.49 ± 0.58) compared to formula fed infants (1.85 ± 0.86, p<0.01) with no between group difference).
Depression, Self-Efficacy and Motivation
Significant between weight groups differences were found in depression and appearance’s motivation (Table 4). Statistically significant correlations were found between the child’s BMI percentile and appearance motivation (r=0.21), symptoms of depression (r=0.17), and relationship with the mother (supervision factor) (r=0.17).
| Parameters | Range | Normal weight | Overweight and obese | Morbid obese | Calculation | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variables | -- | M | SD | M | SD | M | SD | F(8,286) | Eta² | |
| Depression | 1-3 | 1.22 | 16 | 1.25 | 19 | 1.43 | 32 | ***11.14 | 13 | |
| Self-efficacy | 1-5 | 4.19 | 66 | 4.1 | 65 | 4.04 | 58 | 72 | 1 | |
| Motivation | 1-5 | |||||||||
| Health | -- | 3.49 | 98 | 3.68 | 93 | 3.86 | 86 | 2 | 3 | |
| Appearance | -- | 2.39 | 87 | 2.69 | 98 | 3.06 | 1.05 | **5.89 | 7 | |
Table 4: Depression, self-efficacy and motivation among study participants (**p<0.001, ***p<0.01).
The average depression score was highest among the morbid obesity group and decreased with the degree of obesity. Bonferroni correction analysis found significant differences between morbid obesity group and both normal weight and overweight groups, p<0.001. Appearance was a strong motivator to reduce/maintain weight among morbid obese children and significantly higher compared to the normal weight group, p<0.01.
In summary, significant differences were found between morbid obesity and normal weight group in the depressive symptoms, motivation for weight loss and parent-child relationship. In addition, significant differences between the weight groups were found in familial obesity, in the way the child was fed as a baby, in the amount of physically active days and in number of friends.
Discussion
Our study evaluated demographic, familial and emotional differences between normal weight, overweight, obese and morbid obese children.
We found a non-linear relationship between birth weight and childhood obesity, as demonstrated in previous studies [35-37]. Birth weight reflects intrauterine conditions, interestingly children born either at low or high birth weight were found to have higher likelihood to become obese as older children. Possible reasons for this finding are both psychosocial and physiologic [38,39]. It was suggested that intrauterine growth retardation is associated with the development of more efficient energy systems that when exposed later in life to an energy rich environment may lead to overweight and obesity [40]. In addition, maternal weight during pregnancy is known to influence the infant’s birth weight [37]. Although this was not evaluated in the current study, we did find higher prevalence of overweight and obese mothers in the morbid obesity group. These two risk factors: High or low birth weight and maternal overweight may help us to identify a population at risk for childhood obesity and start early prevention programs.
Familial obesity is considered an important determinant in the child’s weight status. Our morbid obese group had the highest prevalence of mother, father and sibling’s obesity, as previously reported [2,41-43]. Interestingly, sibling's weight status was found to be closely related to the child weight status. While this may reflect familial genetic predisposition towards obesity, it may also suggest that eating, physical activity and sedentary habits of siblings develop in the same environment and emphasizes the fact that the treatment of childhood obesity should include the whole family.
Previous studies reported that obese children have different psychosocial characteristics and more distress compered to overweight and normal weight children [44]. Our findings regarding parent-child relationship showed significant between group differences in mother and father supervision factors. According to the children’s report in our study, the degree of supervision increased as BMI percentile increased. There are few studies, focused on parenting styles, supporting these findings [45,46]. However, since most of the studies are cross-sectional, they cannot distinguish between cause and effect, namely, did the increase in BMI percentile lead to higher supervision, or close parental supervision lead to higher BMI percentile. Increased parental supervision may lead to unwanted results such as resistance and opposition, leading to weight gain. Stein and colleagues demonstrated that in parents that restricted food consumption from their overweight children without volitional involvement of their children, the process lead to continuous weight gain [44]. A recent meta-analysis did not support making general parenting styles, parental demandingness, responsiveness, and the quality of the parentchild relationship a main target of preventing and treating obesity [45]. We found a higher father rejection-confrontation as BMI percentile increases. Adolescents, especially females, reported that they have more difficulties to communicate with their fathers [23,47]. Mother and father supervision and father rejection-confrontation were both found to be higher in boys. This supports other studies suggesting that during adolescence girls have more parental support and closeness compered to boys [33,48]. Interestingly, children that weren’t breastfed as babies reported higher feeling of mother rejection-confrontation compared to children who were breastfed as babies. This finding can be explained by John Bowlby's Attachment Theory [49] which claims that early life attachment is a crucial psychobiological factor that will influence the child’s later development and personality. We found lower breastfeeding rates as BMI percentile increased. Previous studies have demonstrated that breastfeeding may be protective from development of childhood obesity. This can be explained by both psychological factors as well as by the unique ingredients of mother milk and by development of hunger and satiation mechanisms during babies’ breast feeding [36,50]. More research is needed to explore the relationship between childhood obesity, breast feeding and motherchild relationship.
We found that the motivation appearance score is higher in the more obese children. Other studies also found that obese children are mainly troubled by their appearance [51], unlike adults, who are troubled by the health consequences of obesity and by appearance dissatisfaction [16,17]. Appearance and social issues were also the main causes for children's self-referral to a tertiary center weight management program [52]. This is an important message to health care professionals caring for obese children. Probably “frightening” children with the health consequences of obesity will have much less impact than enhancing obese children’s motivation for weight loss by focusing on improvement of appearance.
As in adult studies [7,53], we found higher symptoms of depression in the morbid obese group compared with overweight and normal weight groups. We also found a positive correlation between symptoms of depression and BMI percentiles. These findings are supported by variety of studies [2,6,10-14,54], and are extremely important since in Israel 13.3% from the fifth-grade children are morbid obese [1].
In adults, there are two main explanations to the relationship between depression and obesity: Physiological and emotional. Physiologically, obesity is a low grade inflammatory state, and inflammation is suggested to be an important mediator between obesity and depression [55]. Emotionally, as in adults, in children obesity is related to emotional distress and low quality of life [2,53]. Since the majority of previous studies are cross sectional, a causal relationship cannot be determined. However, some longitudinal studies in children found that symptoms of depression predicted weight gain and later obesity in adulthood, especially in girls [8,56]. Whether the depression itself or the anti-depressive medical treatment or the combination of the two leads to obesity needs to be further evaluated. Along with the depressive symptoms, morbid obese children exhibit social difficulties [57] and it is not surprising that the parents of our morbid obese children reported that their children have less social contacts and less “good friends” compered to overweight and normal weight peers.
We also found that overweight, obese and morbid obese children are less active at leisure time respective to their obesity degree. This supports the notion that childhood obesity, social environment and physical activity are well related [58-60], and highlights the importance of evaluating and including a behavioral/psychological component in the treatment of childhood obesity, especially in morbid obesity children.
In summary, we are facing a global epidemic of childhood obesity that not only bears medical complications, but also puts the obese child and his family in a troubling psychosocial distress. Addressing these difficulties, should be an integral part in any effort to prevent or treat childhood obesity.
This study is part of a Ph.D. Thesis carried out under the supervision of Prof. Yaacov Katz, School of Education, Bar-Ilan University, Israel.
References
- World Health Organization (2013) Growth data, school children in Israel. Director of public health, Ministry of health, Israel.
- Latzer Y, Stein D (2013) A review of the psychological and familial perspectives of childhood obesity. J Eat Disord 25: 7.
- Franklin J, Denyer G, Steinbeck KS, Caterson ID, Hill AJ (2006) Obesity and risk of low self-esteem: A statewide survey of Australian children. Pediatr 118: 2481-2487 .
- Strauss RS (2000) Childhood obesity and self-esteem. Pediatr 105: 15-20
- Eliakim A, Nemet D (2008) Physical activity in children in health and disease. Edition 1, Yahlom print, Kfar-Saba, Israel. Pp.136-137.
- Esposito M, Gallai B, Roccella M, Marotta R, Lavano F, et al. (2014) Anxiety and depression levels in prepubertal obese children: A case-control study. Neuropsychiatr Dis Treat 10: 1897–1902.
- Onyike CU, Crum RM, Lee HB, Lyketsos CG, Eaton WW (2003) Is obesity associated with major depression: Results from the third national health and nutrition examination survey. Am J Epidemiol 158: 1139-1147.
- Pulkki RL, Elovainio M, Kivimaki M, Mattsson N, Raitakari OT, et al. (2009) Depressive symptoms and the metabolic syndrome in childhood and adulthood: A prospective cohort study. Health Psychol 28: 108–116.
- Harrington R (1999) Depressive disorders. John Wiley & Sons Ltd, New York, USA. Pp. 233-265.
- Braet C, Mervielde I (1997) Psychological aspects of childhood obesity: A controlled study in a clinical and nonclinical sample. J Pediatr Psychol 22: 59-71 .
- Pott W, Albayrak O, Hebebrand J, Pauli PU (2010) Course of depressive symptoms in overweight youth participating in a lifestyle intervention: Associations with weight reduction. J Dev Behav Pediatr 31: 635-640 .
- Crow S, Eisenberg ME, Story M, Neumark SD (2006) Psychosocial and behavioral correlates of dieting among overweight and non-overweight adolescents. J Adolesc Health 38: 569-574.
- Gibson LY, Byrne SM, Blair E, Davis EA, Jacoby P, et al. (2008) Clustering of psychosocial symptoms in overweight children. Aust N Z J Psychiatry 42: 118-125.
- Blaine B (2008) Does depression cause obesity: A meta-analysis of longitudinal studies of depression and weight control. J Health Psychol 13: 1190-1197 .
- Pinhas HO, Singer S, Fradkin A, Modan D, Reichman B, et al. (2006) Health-related quality of life among children and adolescents: Associations with obesity. Int J Obes 30: 267-272 .
- Wee CC, Davis RB, Phillips RS (2005) Stage of readiness to control weight and adopt weight control behaviors in primary care. J Gen Intern Med 20: 410-415.
- O'Briena K, Venn BJ, Perry T, Greene TJ, Aitken W, et al. (2007) Reasons for wanting to lose weight: Different strokes for different folks. Eat Behav 8: 132-135.
- McWhorter JW, Wallmann HW, Alpert PT (2003) The obese child : Motivation as a tool for exercise. J Pediatr Health Care 17: 11-17.
- Ventura AK, Birch LL (2008) Does parenting affect children's eating and weight status. Int J Behav Nutr Phys Act 5: 15.
- Zeller MH, Boles RE, Reiter PJ (2008) The additive and interactive effects of parenting style and temperament in obese youth seeking treatment. Int J Obes 32: 1474-1480.
- Cislak A, Safron M, Pratt M, Gaspar T, Luszczynska A (2012) Family-related predictors of body weight and weight-related behaviours among children and adolescents: A systematic umbrella review. Child Care Health Dev 38: 321-331.
- Mayseless O (2001) Young Israeli men in the transition from adolescence to adulthood: The role of military service. Studies Edu 5: 159-190.
- Ackard DM, Neumark-Sztainer D, Story M, Perry C (2006) Parent-child connectedness and behavioral and emotional health among adolescents. Am J Prev Med 30: 59-66.
- Zeller MH, Reiter-Purtill J, Modi AC, Gutzwiller J, Vannatta K, et al. (2007) Controlled study of critical parent and family factors in the obesigenic environment. Obesity 15: 126-136.
- Tremblay L, Rinaldi CM (2010) The prediction of preschool children's weight from family environment factors : Gender-linked differences. Eat Behav 11: 266–275.
- Su W, di Santo A, (2011) Preschool children’s perceptions of overweight peers. J Early Child Res 10: 19–31.
- Musher-Eizenman DR, Holub SC, Miller AB, Goldstein SE, Edwards-Leeper L (2004) Body size stigmatization in preschool children: The role of control attributions. J Pediatr Psychol 29: 613-920.
- Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, et al. (2002) 2000 CDC growth charts for the United States: Methods and development. Vital Health Stat 246: 1-190.
- Coleman L, Coleman J (2002) The measurement of puberty: A review. J Adolesc 25: 535-550.
- Kovacs M (1981) Rating scales to assess depression in school-aged children. Acta Paedopsychiatr 46: 305-315.
- Meyer AH, Weissen-Schelling S, Munsch S, Margraf J (2010) Initial development and reliability of a motivation for weight loss scale. Obes Facts 3: 205-211.
- Saunders RP, Pate RR, Felton G, Dowda M, Weinrich MC, et al. (1997) Development of questionnaires to measure psychosocial influences on children's physical activity. Prev Med 26: 241-247.
- Mayseless O, Wiseman H, Hai I (1998) Adolescents’ relationships with father, mother and same gender friend. J Adolesc Res 13: 101-123 .
- Godin G, Shephard RJ (1958) A simple method to assess exercise behavior in the community. Can J Appl Sport Sci 10: 141-146.
- Cunningham SA, Kramer MR, Narayan KMV (2014) Incidence of childhood obesity in the United States. N Engl J Med 370: 404-411.
- Oddy WH, Mori TA, Huang RC, Marsh JA, Pennell CE, et al. (2014) Early infant feeding and adiposity risk: From infancy to adulthood. Ann Nutr Metab 64: 262-270.
- Yu ZB, Han SP, Zhu GZ, Zhu C, Wang XJ, et al. (2011) Birth weight and subsequent risk of obesity: A systematic review and meta-analysis. Obes Rev 12: 525-542.
- Stansfield BK, Fain ME, Bhatia J, Gutin B, Nguyen JT, et al. (2016) Nonlinear relationship between birth weight and visceral fat in adolescents. J Pediatr 174: 185-192.
- Jornayvaz FR, Vollenweider P, Bochud M, Mooser V, Waeber G, et al. (2016) Low birth weight leads to obesity, diabetes and increased leptin levels in adults: the Colaus study. Cardiovasc Diabetol 15: 73.
- Gluckman PD, Hanson MA (2004) Developmental origins of disease paradigm: A mechanistic and evolutionary perspective. Pediatr Res 56: 311-317.
- Fogelholm M, Nuutinen O, Pasanen M, Myohanen E, Saatela T (1999) Parent-child relationship of physical activity patterns and obesity. Int J Obes Relat Metab Disord 23: 1262-1268.
- Gomes TN, Katzmarzyk PT, Santos DFK, Souza M , Pereira S, et al. (2014) Overweight and obesity in Portuguese children: Prevalence and correlates. Int J Environ Res Public Health 11: 11398-11417.
- Pachucki MC, Lovenheim MF, Harding M (2014) Within-family obesity associations: Evaluation of parent, child, and sibling relationships. Am J Prev Med 47: 382-391. â€
- Stein D, Weinberger-Litman SL, Latzer Y (2014) Psychosocial perspectives and the issue of prevention in childhood obesity. Front Public Health 2: 104.
- Pinquart M (2014) Associations of general parenting and parent-child relationship with pediatric obesity: A meta-analysis. J Pediatr Psychol 39: 381-393.
- Rhee KE, Lumeng JC, Appugliese DP, Kaciroti N, Bradley RH (2006) Parenting styles and overweight status in first grade. Pediatrics 117: 2047-2054.
- Al Sabbah H, Vereecken CA, Elgar FJ, Nansel T , Aasvee K, et al. (2009) Body weight dissatisfaction and communication with parents among adolescents in 24 countries: International cross-sectional survey. BMC Public Health 9: 52
- Helsen M, Vollebergh W, Meeus W (2000). Social support from parents and friends and emotional problems in adolescence. J Youth Adolescence 29: 319-335.
- Bowlby J (1969) Attachment and loss, Volume I: Attachment New York: Basic Books.
- Gale C, Logan KM, Santhakumaran S, Parkinson JR, Hyde MJ, et al. (2012) Effect of breastfeeding compared with formula feeding on infant body composition: A systematic review and meta-analysis. Am J Clin Nutr 95: 656-69.
- Mariano-Veloso S, Gaspar Matos M, Fonseca H, Carvalho M, Alves Diniz J, et al. (2012) Cross-sectional psychosocial differences between clinical and nonclinical samples of overweight adolescents. Arch Exerc Health Dis 3: 123-131.
- Yaeger-Yarom G, Nemet D, Eliakim A (2011) Causes and patterns of referral to a tertiary, multidisciplinary program for the treatment of childhood obesity. J Pediatr Endocr Met 24: 303-306 .
- Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, et al. (2010) Overweight, obesity, and depression: A systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry 67: 220-229.
- Quek YH, Tam WW, Zhang MW, Ho R (2017) Exploring the association between childhood and adolescent obesity and depression: A metaâ€analysis. Obes Rev 18: 742-754.
- Shelton RC, Miller AH (2010) Eating ourselves to death and despair: The contribution of adiposity and inflammation to depression. Prog Neurobiol 91: 275-299.
- Anderson S, Cohen P, Naumova EN, Must A (2006) Association of depression and anxiety disorders with weight change in a prospective community-based study of children followed up into adulthood. Arch Pediatr Adolesc Med 160: 285-291 .
- Zeller MH, Reiter-Purtill J, Ramey C (2008) Negative peer perceptions of obese children in the classroom environment. Obesity 16: 755-762.
- Lin LJ, Chang HY, Luh DL, Hurng BS, Yen LL (2014) The trajectory and the related physical and social determinants of body mass index in elementary school children: Results from the child and adolescent behaviors in long-term evolution study. J Obes 9.
- Sawka K J, McCormack GR, Nettel-Aguirre A, Blackstaffe A, Perry R, et al. (2014) Associations between aspects of friendship networks , physical activity, and sedentary behaviour among adolescents. J Obes 12.
- Kremera P, Elshaugb C, Lesliec E, Toumbouroud JW, Pattone GC, et al. (2014) Physical activity, leisure-time screen use and depression among children and young adolescents. J Sci Med Sport 17: 183-187.
Citation: Pantanowitz M, Katz Y, Eliakim A, Nemet D (2018) Psychosocial Differences between Children’s Weight Groups. J Obes Weight Loss Ther 8: 374. DOI: 10.4172/2165-7904.1000374
Copyright: © 2018 Pantanowitz M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3570
- [From(publication date): 0-2018 - Nov 22, 2025]
- Breakdown by view type
- HTML page views: 2698
- PDF downloads: 872