Psychosocial factors associated with quality of life in palliative care and end of life adult cancer patients: an umbrella review
Received: 17-Feb-2025 / Editor assigned: 20-Feb-2025 / Reviewed: 13-Mar-2025 / Revised: 14-Apr-2025 / Published Date: 01-Jun-2025
Abstract
Background: Little is known about what factors affect Quality of Life (QoL) in persons with cancer who are in the palliative phase of their disease. This Umbrella Review (UR) aims to systematically examine psychological, social and clinical factors affecting QoL in the Palliative Care of advanced cancer. Methods: Four scientific databases (PubMed, Embase, Scopus, and PsycInfo) were searched to identify systematic reviews between 2021 and 2023, involving adult cancer patients in PC, and analyzing the relationship between QoL and psychosocial and/or clinical factors. The data extraction and synthesis process followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, and risks of bias were assessed using the Assessment of Multiple Systematic Reviews 2 (AMSTAR2) rating scale. Results: Three systematic reviews were included, with different study designs and a total of 182,647 subjects across different cancer types. Depression and spirituality/religiosity emerged as recurrent themes impacting QoL. Additionally, clinical variables such as pain intensity, fatigue, and medical treatment strategies revealed associations with QoL. Family support/function was identified as the only social factor positively influencing QoL. Conclusion: Findings highlight the importance of addressing spirituality, anxiety, depression, and family support in Palliative Care settings to improve the QoL of cancer patients and caregivers. This UR is a useful resource for researchers, clinicians, and policymakers because it underlines the association between QoL and a variety of psychosocial and clinical factors in EoL cancer patients and gives an overview of the concept of QoL in this cancer population.
Keywords
Cancer; Quality of life; Palliative care; Umbrella review
Introduction
Globally, cancer is the second leading cause of death and according to the World Health Organization (WHO) each year it is estimated that 56.8 million people are in need of Palliative Care (PC). PC is defined by the WHO [1] as “active total care of the patients whose disease is not responsive to curative treatment; focusing on specific needs and preferences of individuals”, thus providing help in a wide range of issues including for example communication, understanding of treatments, and acceptance of diagnosis and severity of illness [2]. It occurs across a continuum, beginning at the time of diagnosis of a serious illness until End of Life (EoL).
A full integration of PC in an oncological setting is now considered the standard when caring for patients with advanced cancer. In recent years, several studies on PC focused on providing support for patients nearing EoL. Considering the lack of consensus in the definition of this type of population [1], in the present study EoL patients include cancer patients who received a prognosis <12 months and who have stopped undergoing curative treatment. EoL patients in PC, as well as their families and/or caregivers receive physical, emotional, social, spiritual and psychosocial support, including both supportive programs and hospice care. Indeed, the goal of PC is to provide a holistic care approach and control symptoms during the course of advanced disease also while antineoplastic treatment can still be appropriate [3,4].
Hence, the overall aim of PC is to improve QoL of patients and their families and/or caregivers using a team approach to personalize interventions [5]. When the goal of treatment is no longer cure, high-quality palliative cancer care can provide appropriate management and QoL control across the entire disease trajectory until the EoL. Although the concept of QoL does not have the same meaning to every person [6,7], some aspects of QoL are universal [8] and are best characterized by four different domains: physical health, psychological wellbeing, social health, and overall health and system. When applied in the context of an individual coping with PC, QoL is largely affected by disease progression; at the same time, it incorporates information from multiple life domains [9]. The physical QoL component assesses health status, body functions, symptoms, sexual well-being, and body image. The psychological QoL component focuses on psychological functioning, mood indicators, cognitive phenomena, personal meaning of the cancer and life threatening experience, and emotional limitations. The emotional domain is interconnected with the social domain, which evaluates the impact of cancer on social roles and the importance of social support networks.
Evidences suggest that early identification of the need for PC has different benefits both for patients and caregivers, such as better QoL [10], a good accompaniment to end of life and death [11] and better adjustment. Coherently, people with long-term illnesses are estimated to be two to three times more likely to experience low grade of QoL (with higher psychological distress or mental health issues) than the general population [12,13]. Psychological aspects such as anxiety and depression, coping strategies, communication, resilience and decision making have been previously reported as important factors affecting patients’ overall well-being.
Even though several studies have been already conducted focusing on the relationship between psychosocial factors and QoL in patients and caregivers [14], no previous Umbrella Review has been conducted to summarize all the factors impacting on QoL in PC.
Therefore, the aim of this umbrella review is to synthesize the psychosocial factors related to QoL in EoL adult cancer patients.
Methods
An Umbrella Review (UR) is a narrative compilation into one document with text, tables, and graphics of evidence from multiple systematic reviews and meta-analysis. It permits to examine what is known and not known in order to provide a summary of existing research syntheses related to a given topic or question. In this paper an UR was conducted to synthesize the psychosocial factors related to QoL in EoL cancer patients [15].
This UR was registered in the International Prospective Register of Systematic Reviews (PROSPERO- protocol number: CRD42023413281) and was conducted following the guidelines from Joanna Briggs Institute (JBI) [16].
Data sources and search strategy
A search strategy was built and adapted by a research librarian (A. V. A) for the following four electronic databases: PubMed, Embase, Scopus and PsycInfo. This search string was optimized with a combination of several search terms divided into the following topics: Cancer, Quality of Life, Factors, Psychosocial, Impact, End of Life. Specific search strings developed for each database are presented in Table 1 and Table 2.
| Author & Year of Publication | Study Origin | Study Design | Studies Included | Participants | Cancer Group | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of studies included | Type of studies included | Years of published included articles | Country of origin of included studies | Number of patients in included articles | Range number of patients in included articles | Socio-demographic characteristics | Cancer type | ||||
| Gayatri et al. 2021 |
Indonesia | systematic review | 55 | 36 cross-sectional, 15 cohort studies, 2 RCTs, and 2 quasi-experimental studies. | 1999-2019 | Asia (n = 40), Latin America and Caribbean region (n = 10), and Africa (n = 5) | 11380 | Range number of included pts: 15-1245 |
sex: varied among studies | all cancer types | 4305 |
| Age range: 18-94 | blood | 25 | |||||||||
| breast | 640 | ||||||||||
| cervical cancer | 224 | ||||||||||
| cervix | 39 | ||||||||||
| colon and rectum | 373 | ||||||||||
| digestive | 5 | ||||||||||
| esophageal | 105 | ||||||||||
| esophagus | 62 | ||||||||||
| gallbladder | 20 | ||||||||||
| gastric | 123 | ||||||||||
| gastrointestinal | 228 | ||||||||||
| genitourinary tract | 24 | ||||||||||
| gynecological | 315 | ||||||||||
| head and neck | 998 | ||||||||||
| hepatobilary | 114 | ||||||||||
| larynx | 10 | ||||||||||
| liver | 281 | ||||||||||
| lung | 2093 | ||||||||||
| no number reported | 1042 | ||||||||||
| non small cell lung | 10 | ||||||||||
| oropharynx | 22 | ||||||||||
| ovarian | 14 | ||||||||||
| pancreas | 49 | ||||||||||
| prostate | 6 | ||||||||||
| rectum | 13 | ||||||||||
| respiratory tract | 41 | ||||||||||
| stomach | 193 | ||||||||||
| uterine cervix | 6 | ||||||||||
| Flyum et al. 2021 |
Norway | systematic review and meta-analysys | 11 | 5 prospective/longitudinal, 6 cross-sectional | 2009-2020 | Austria (n=1), Canada (n=1), Denmark and Sweden (n=1), Finland (n=3), Netherlands (n=1), Poland (n=2), South Corea (n=1), Turkey (n=1) | 839 | Range number of included pts: 35-1978 |
Age range: > 18 | colon and rectum | 839 |
| sex: varied among studies | |||||||||||
| Bai et al. 2015 |
Georgia (USA) | systematic review | 36 | 32 cross-sectional, 4 longitudinal | 1996-2014 | Australia (n=2), Canada (n=1), Japan (n=1), Jordan (n=2), Iran (n=1), Italy (n=1), Netherlands (n=1), United States (n=27) | 170428 | Range number of included pts: 45-8805 |
Age range:>18 sex: varied among studie |
all cancer types | 169011 |
| breast | 786 | ||||||||||
| colorectal | 258 | ||||||||||
| prostate | 373 | ||||||||||
Table 1: Characteristics of the included studies (Part A).
| Author & Year of Publication | Factors | Association with QoL | Outcomes | ||
|---|---|---|---|---|---|
| Psychological Factors | Social Factors | ||||
| 1 | Gayatri et al. 2021 |
Family function/support | Positive association -> QoL | Higher family support is associated with better QoL | |
| Depression and anxiety | Negative association -> QoL | Higher depression and anxiety symptoms are associated with lower QoL | |||
| Spirituality/Religiosity | Positive association -> QoL | Spirituality/religiosity is associated with better QoL | |||
| Diagnosis awareness | one study reported positive association -> QoL; three studies reported a negative association -> QoL | one study reported positive association -> QoL; three studies reported a negative association -> QoL | |||
| 2 | Flyum et al. 2021 |
Depression | Negative association -> HRQoL | higher levels of depression are associated with lower HRQoL | |
| Feeling of coherence | Positive association -> HRQoL | higher feeling of coherence is associated with better HRQoL | |||
| Intrusive thoughts | Negative association -> HRQoL | intrusive thoughts is associated with lower HRQoL | |||
| Awareness of terminal disease | Negative association -> HRQoL | awareness of terminal disease is associated with lower HRQoL | |||
| 3 | Bai et al. 2015 |
Spirituality (Faith and Meaning/Peace) | Positive association -> QoL | higher overall spiritual well-being is associated with better QOL | |
Table 2: Characteristics of the included studies (Part B).
Inclusion and exclusion criteria
For the present UR clear exclusion and inclusion criteria were established to avoid biases that may impact on the quality of the research. Hence, the research was limited to (a) systematic reviews, (b) without geographical restrictions, (c) conducted from 1st January 2012 to January 2023 (the research was limited to this year because the field of Palliative medicine and care is rapidly changing), (d) including adult cancer patients (>18 years), (e) in PC and (f) investigating the relationship between QoL and psychosocial factors. These eligibility criteria were established according to the research question (PICO questions; P: end of life adult cancer patients; I: not applicable; C: not applicable; O: factors affecting QoL).
The exclusion criteria for the present UR included (a) non-psychosocial factors associated with QoL (e.g. economic, cultural, pharmacological outcomes), (b) non-EoL adult cancer patients (e.g. survivors, other diseases aside from cancer, caregivers, families of EoL cancer patients, children…).
Literature search and data selection
Starting from this search strategy, two researchers (D. S. and V. V. ) started the preliminary screening independently (based on the reading of titles and abstracts) by importing results into Rayyan [17], an online Software, using the “blinded” mode. Duplicates from different electronic databases were removed. In case of disagreements in the decisions of the eligibility of studies, a third reviewer (C. M.) was involved and ensued a group discussion with the full-text review to reach a consensus supervising the entire process of decision. All the potentially admissible articles retrieved for full-text screening were accessed using the inclusion and exclusion criteria. Any doubts for the final inclusion were settled through consensus. The reference lists of all the included articles were also screened to find other relevant articles that were not identified during the automatic search. The grey literature was not considered.
Consequently, an Excel© worksheet designed by the research team with registered included articles was organized as follows: publication data (title, authors, year), study origin, studies characteristics (number of studies included in each review, study design, year of publication of included articles, country origin of included articles), aim of each review, participant details (total number, sociodemographic characteristics if included in the reviews), type of cancer diagnosis and methodological quality of the included reviews. Authors also collected clinical factors that were identified in studies researching psychosocial factors.
Data synthesis
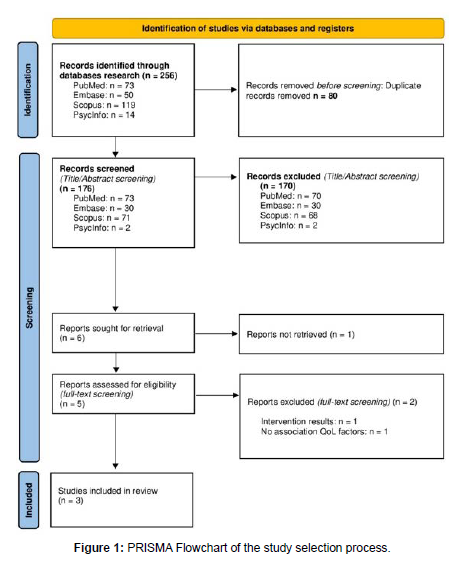
The selected reviews were reported using the guidelines for Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [18]; the PRISMA application was independently carried out by two researchers (D. S. and V. V.). Subsequently, the evaluation process was reviewed by a third investigator (C. M.). Once the consensus of the reviewers was reached, these data were incorporated into the Excel table.
Assessment of methodological quality and risks of bias
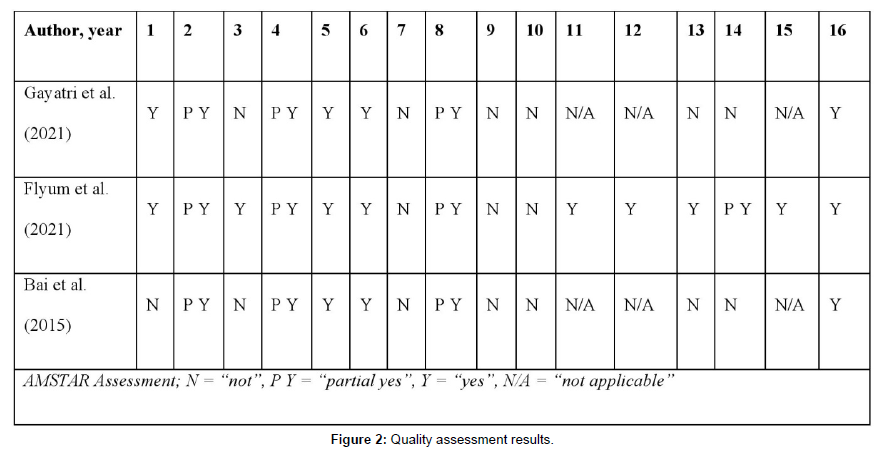
Finally, two investigators (DS and VV) independently assessed the methodological quality of included Systematic Reviews and Meta-analysis using the Assessment of Multiple Systematic Reviews 2 (AMSTAR2, [19]) rating scale. Any disagreements about the rating were solved through discussion. This checklist includes 16 items to evaluate the quality and the bias of the selected studies. Each article received a score based on the number of positive, partial positive and negative responses (the higher was the rate of positive responses, the lower was the risk of bias).
For this UR AMSTAR 2 rating guidelines were followed but the scoring was modified for item 1 (“Did the research questions and inclusion criteria for the review include the components of PICO?”), where the authors decided to give the following scores: “Yes”, “Partially yes”, or “Not”. “Yes” was rated if the Systematic Review (SR) had a clear and predefined research question and all the elements of PICO were explicitly described somewhere in the SR’s report. The rating “partially yes” was used when the PICO questions were partially described in the SR. For example, if the SR reported only study population and outcome, the authors gave “partially yes”, instead of “not”.
Results
Data extraction and analysis
Through the scientific database research, 256 potentially relevant references were found in PubMed, Embase, Scopus and PsycInfo; after the detection of duplicates, 176 reviews remained for the screening of titles and available abstracts. After this screening, 169 articles were excluded. The most common reason for exclusion was type of paper (e.g. commentaries, editorials). A detailed overview of the study selection process and exclusion reasons can be found in Figure 1. A total number of 6 reviews remained for the screening based on the full-text. Of these, one review was excluded because the full-text was not available, two studies were excluded because one presented interventional outcomes and the other one did not investigate the relationship between QoL and psychosocial factors. For these reasons, 3 studies were included in the present UR (Figure 1).
From: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi: 10.1136/bmj.n71
Study characteristics
A total number of three SRs met inclusion and exclusion criteria, of which one includes also a meta-analysis [20]. One SR was published in 2015 [21] and the other two in 2021; the articles included in each of the included SRs spanned from 1996 to 2020 in terms of their publication years. The included SRs cover different study design: cross-sectional studies (n=74), cohort studies (n=15), RCTs (n=2), quasi-experimental studies (n=2), and longitudinal studies (n=9) were conducted. The number of studies included in each SR ranged from 11 to 55. Although all three included articles featured an explicit search strategy, study selection methodology, and PRISMA flowchart, only one study explicitly declares to follow a protocol previously registered on PROSPERO [22].
Even though the number of included studies is limited, the total amount of examined subjects was 182.647. Despite all the included SRs referred to the palliative care, the summarized articles included different cancer populations (Table 1), except for one SR focusing on only rectum and colon cancer [20]. Furthermore, population also varies for number (with a total range between 15-8805), sex and study origin. Indeed, one study was published by European institutions [20], while the remaining two were conducted respectively in Indonesia [22] and in the United States [21]. Most of the included studies in the three SRs are from Asia (n=46), followed by America and Caribbean regions (n=30), and Europe (n=11); few articles included Africa (n=5) and Oceania (n=2) researches.
A more comprehensive overview is available in Table 1 and Table 2.
QoL and associated psycho-social and clinical factors
The SRs investigate the relationship between QoL and different psychological factors. Overall, there are no common factors to all three SRs, but depression is reported as a main factor across two of them [20,22] and spirituality/religiosity is identified as a main factor throughout two SRs [21,22]. Evidence shows that spirituality/religiosity is positively associated with QoL (higher scores in spirituality are associated with better QoL), meanwhile depression (analyzed in association with anxiety in one systematic review) seems to be negatively associated with QoL (presence of depression is associated with lower QoL). Other investigated psychological factors affecting QoL are feeling of coherence, intrusive thoughts, and awareness of terminal disease.
Only one social factor was investigated in one of the included studies: family support/function, referring to behaviors and roles that operate within a family system, was positively associated with QoL [22].
Finally, two SRs also investigated the association between clinical variables on QoL. Specifically, one review [22] reported that undergoing medical treatment or symptom management strategies positively impact on QoL, while pain intensity and fatigue negatively affect QoL. The other SR showed that the effects of targeted treatments and the severity of the disease are associated with lower QoL [20].
Quality assessment results
Quality appraisal was independently conducted on the included three SRs by two authors (D. S. and V. V.). Any disagreements about the rating were solved through discussion with a third researcher (C. M.).
Although all three SRs reported critically low scores (because the reviews have more than one critical flaw), Flyum et al. satisfied a greater number of the suggested criteria [20], while Bai et al., and Gayatri et al. showed more “not” than “yes” [21,22], as shown in Figure 2.
Discussion
The present UR investigated factors associated with QoL, especially categorizing them in psychological, social, and clinical domains and specifying their positive or negative associations on EoL patients’ well-being. To the best of our knowledge, this is the first UR of SRs on the key clinical and psychosocial factors affecting QoL in adult cancer patients, without limitation on the type of cancer. A total number of 3 published SRs were selected and analyzed, including a total of 182.647 subjects suffering from different cancer types, but mostly focusing on lung, colorectum, and breast cancer.
Overall, QoL is an essential component in the cancer trajectory, especially during palliative and EoL care [23-27]. In fact, the evaluation of QoL in advanced cancer patients is an important procedure both in the identification of a patient’s overall condition and in the evaluation of services’ quality. Different studies have described and analyzed QoL impairments in PC settings, thus highlighting the need for a more comprehensive approach that integrates medical care with subjective outcomes [28].
In the present UR, findings showed that spirituality and religiosity are the most investigated factors in this cancer phase: they are consistently associated with higher scores in QoL and are defined as spiritual comfort, thus being a central aspect in PC patients [29]. Indeed, EoL patients frequently found greater relief and hope in spiritual belief practice when coping with the terminal phase; patients facing physical decline and severe symptoms often look for replies to questions about death and meaning of life, thus focusing on the importance of spirituality for their well-being [30,31]. Generally, spiritual well-being is considered a determinant factor influencing QoL and involves different dimensions such as faith, meaning of life and peace of mind [32].
Nevertheless, the growing focus on spirituality as a factor influencing QoL needs some consideration. Despite the extended recognition of their importance in oncology, religion and spirituality remain difficult to gauge and are hard to define in an unambiguous and unique way. Over the past decades, there has been a shift in the meaning of spirituality: traditionally, it was primarily associated with deep religious spirit, but it has since been expanding to encompass a broader range of connotations and interpretations. In general, it is now widely accepted that the concepts of religion and spirituality are connected in a wider construct embracing different domains, such as beliefs and practices that are not only associated with a religious organization, but also include experiences, a sense of purpose and connection to the moment, which implies mental well-being too [33]. In this way, spirituality and religiosity can positively affect cancer patients’ ability to cope with cancer, allowing them to be in contact with the present moment and encourage the acceptance of the current condition. Moreover, these abilities have been associated with several psychological factors, such as social support mechanism, resilience, coping strategies [34]. Consequently, several researches have demonstrated that higher levels of spirituality are associated with lower levels of psychological distress, depression, hopelessness, and suicidal ideation among advanced cancer patients [35-39]. These findings are in line with the associations reported in this UR, highlighting the important interconnection between psychosocial and clinical status in EoL care.
Furthermore, the presence of depression and anxiety has emerged as a significant factor that is closely associated with QoL. In this case, the outcomes have shown that patients reporting higher anxious and depressive symptoms also displayed lower QoL. This is in line with other researches in which EoL cancer patients show higher risk of psychological distress, anxiety and existential distress [37]. Being diagnosed with an incurable illness can lead to psychological symptoms, distress and significant emotional suffering [40]. In addition to these psychological challenges, these patients commonly have to deal with existential thoughts regarding death and loss of meaning of life [41]. Additionally, they also experience physical symptoms related to their illness, such as pain, fatigue, and social symptoms which include feeling of isolation and detachment from others. The relationship between depression, physical and social suffering is reciprocal: each influences and affects the other [42]. Depression can intensify physical suffering, exacerbating pain and social discomfort; conversely, chronic physical suffering can contribute to the development or worsening of depression symptoms and isolation. The interplay between these aspects is complex and multifaceted, emphasizing the interconnected nature of mental and physical health. Besides, a significant overlap exists between symptoms used to diagnose mood disorders and the symptoms frequently encountered by advanced cancer patients [43], such as pain, sleep disturbance, symptoms of fatigue, and weight loss. Indeed, the reciprocal effects of physical suffering and affective disorders are generally supported by evidence demonstrating that interventions targeted on one domain could also affect the other [44]. On the other hand, some authors have suggested that the social decline and social isolation experienced by many EoL patients may be a natural part of the dying process and does not necessarily lead to loneliness, depression or anxiety [45]. Interestingly higher levels of distress, depression, and anxiety were correlated with higher levels of unmet needs and lack of family or social support across different cancer types in patients with advanced cancer [46]. Though little has been analyzed in the collected SRs, it would be interesting to investigate these aspects giver their importance along with social support. Recent studies have indeed shown the interrelation between social support, better QoL, and mental health in PC patients. Responding to patients’ need of support could positively impact on their well-being, probably affecting their perceived self-esteem and sense of dignity, reducing their anxiety of death, and improving their coping abilities with the dying process [47]. Additionally, receiving support from caregivers, especially relatives and closest friends, has resulted as being a crucial component in reducing psychological distress [48], both for patients and caregivers.
The present findings thus highlight the importance of addressing spirituality, anxiety, depression, and family support in PC and EoL settings in order to improve the overall well-being and QoL of cancer patients during this stage of their disease.
Clinical and physical factors associated with QoL have also been here summarized. In line with results previously reported for psycho-social factors, physical symptoms management strategies are associated with better QoL; while patients experiencing relief from adverse reactions or side effects show lower discomfort and mental distress. Conversely, patients with higher perceived pain intensity or higher levels of fatigue, exhibit a lower adaptation to their condition [22]. In addition, advanced cancer patients experience a range of symptoms for which standard medical treatments may not provide sufficient relief [49]. In line with this, symptom management improves not only the patients’ QoL but could also affect the physical and emotional burden on caregivers, leading to a better QoL for both. The psychological and social determinants of QoL in the advanced and terminal phase of cancer therefore reinforce the concept of Palliative care as a discipline based on a comprehensive approach to cancer disease, encompassing not only the physical aspects of symptoms, but also addressing the psychological, social, and spiritual dimensions of suffering. In this way, PC should guarantee that by providing comprehensive relief of symptoms and considering the person as a whole and all aspects of their well-being are attended [50].
Strengths and limitations
There are strengths and limitations in the present work that deserve exploration.
Specifically, studying EoL and PC cancer patients poses a lot of challenges such as ethical considerations, variability of PC models, heterogeneity of patients, cultural and social differences, and as result this population appears underrepresented in scientific research studies. For this reason, this UR stands as the first investigation in adult cancer patients at this stage of the disease pathway, aiming to explore factors related to QoL. As guidelines continue to evolve concerning symptom management and the provision of care needed (such as spiritual care, psychological care, nursing care), efforts have been made to incorporate this population in research cancer studies whenever feasible and appropriate, with the goal of enhancing patients’ well-being and mental health.
In line with these considerations, the number of included studies in the present UR is relatively small, even though the research ranged from 2012 to January 2023 and included studies published in English only. However, more recent studies have focused on this population: two out of three of the included SRs are quite recent, highlighting the growing interest in this type of cancer population. Accordingly, also the limited number of identified factors as results can be attributed to the aforementioned reasons and challenges. The limited time during the palliative phase of treatment has probably contributed to the reduced number of scientific articles investigating aspects related to EoL. Nevertheless, ongoing researches during this cancer phase remains devoted to symptoms management, PC, and efforts to improve QoL for both patients and caregivers in this context.
Finally, AMSTAR levels have highlighted a critically low grade of quality appraisal; for this reason, not only the included reviews should be relied on in order to provide a more comprehensive summary of the available studies on the present topic.
Future studies should be developed to better investigate the specific themes related to palliative care needs; this UR highlights the importance of deeply analysing spirituality and emotional well-being as the most important predictors of QoL in EoL.
Clinical implications
A deeper understanding of psychosocial factors and their impact on QoL in EoL and patients in PC is essential for improving their overall well-being and life satisfaction. The identified factors can be used as a strong starting point by multidisciplinary teams, such as psychologists, social workers, clinicians, and policymakers, to design a patient-centered care system that will be tailored for patients in EoL and palliative care. A patient-centered system will enable the integration of patients’ values and expectations into the development of high-value care, i.e., personalized care focused on patients’ perspectives and needs [51]. This UR identified crucial variables impacting QoL in palliative care; these factors constitute a pivot point for individuals' well-being and self-care management. Recognizing and incorporating these characteristics into high-value care may play a major role in the health management system. For example, depression which is identified as one of the main factors impacting QoL in this cancer stage highlights the importance of the healthcare team in recognizing and addressing it effectively. In this case, the care system will cover not only the clinical aspect but also the psychosocial and emotional issues/needs of cancer patients.
Moreover, the psychosocial factors identified in this UR can be used in developing QoL assessment tools and designing supportive care that aligns with the specific needs of the EoL and PC cancer population. Indeed, psychosocial factors, such as family support, can influence healthy behaviors, strengthening treatment adherence and ensuring clinicians deliver a high-quality care [52]. Additionally, factors impacting QoL can help identify the most relevant challenges that need to be addressed when designing targeted interventions for this cancer care stage. Since QoL is recognized to decrease as the disease progresses, fostering personal well-being is seen as the primary goal of palliative care [25]. Thus, QoL assessment focusing on critical themes in palliative care can contribute to promoting individual well-being, potentially leading to increased QoL [25,53].
Conclusion
Using an UR approach, main factors affecting QoL in cancer patients with advanced disease have been identified. As reported, PC and EoL settings recognize the importance of addressing spirituality, anxiety, depression, family support, and symptoms management to improve the overall well-being and QoL of advanced cancer patients from a comprehensive point of view. This should help patients find comfort and hope, sense of meaning of life, and cope with emotional distress, positively impacting their QoL.
The review was conducted on behalf of the EUonQoL Consortium.
Acknowledgments
We thank Andrea V. Adani for his expertise in developing search strings, which greatly assisted in retrieving relevant literature.
Massimo Costantini for his invaluable assistance and support throughout the project.
We finally would like to thank also co-researchers: Laura Pinnavaia (for her insightful feedback, guidance, and linguistic revision, as a native speaker) and Carina Dantas (for her contributions and comments), who successfully contributed in the completion of this project.
Viktorya Voskanyan is a Ph.D. student in Medical Humanities within the European School of Molecular Medicine (SEMM) at the University of Milan, Italy.
Conflict of Interests
All authors reported no conflict of interest.
Statements & Declarations
Funding
This publication has received funding from the European Union’s Research and Innovation Program HORIZON-MISS-2021-CANCER-02 under Grant Agreement No 101096362 Project EUonQoL.
Data availability
This request is not applicable for Umbrella Review. The tables with all the available information are already presented in the text.
Ethics approval
Ethical approval is not required as we are not collecting participant data as part of this review.
Author Contributions
All authors contributed to the study conception and design. Material preparations, data collection, and analyses were performed D.S, V.V and C.M. The first draft of the manuscript was written by D.S, V.V and C.M, and all authors commented on and edited the manuscript. The final manuscript was read and approved by all authors.
References
- Radbruch L, De Lima L, Knaul F, Wenk R, Ali Z, et al. (2020) Redefining Palliative Care-A New Consensus-Based Definition. J Pain Symptom Manage 60: 754-764.
- Thaniyath T (2019) The Quality of Life of the Patients Under Palliative Care: The Features of Appropriate Assessment Tools and the Impact of Early Integration of Palliative Care.
- Buiting HM, Terpstra W, Dalhuisen F, Gunnink-Boonstra N, Sonke GS, et al. (2013) The Facilitating Role of Chemotherapy in the Palliative Phase of Cancer: Qualitative Interviews with Advanced Cancer Patients. PLoS ONE 8: e77959.
- Fang P, Jagsi R, He W, Lei X, Campbell EG, et al. (2019) Rising and Falling Trends in the Use of Chemotherapy and Targeted Therapy Near the End of Life in Older Patients With Cancer. J Clin Oncol 37: 1721-1731.
- Biswas J, Faruque M, Banik PC, Ahmad N, Mashreky SR (2022) Quality of life of the cancer patients receiving home-based palliative care in Dhaka city of Bangladesh. PLOS ONE 17: e0268578.
- Felce D (1997) Defining and applying the concept of quality of life. J Intellect Disabil Res 41: 126-135.
- Schalock, R. L. (2004) The concept of quality of life: What we know and do not know. Journal of Intellectual Disability Research 48: 203-216.
- Tope DM, Ahles TA, Silberfarb PM (1993) Psycho-Oncology: Psychological Well·Being as One Component of Quality of Life. Psychother Psychosom 60: 129-147.
- Elmqvist MA, Jordhøy MS, Bjordal K, Kaasa S, Jannert M (2009) Health-related quality of life during the last three months of life in patients with advanced cancer. Support Care Cancer 17: 191-198.
- Diamond EL, Russell D, Kryza-Lacombe M, Bowles KH, Applebaum AJ, et al. (2016) Rates and risks for late referral to hospice in patients with primary malignant brain tumors. Neuro Oncol 18: 78-86.
- Cheng SY, Dy S, Hu WY, Chen CY, Chiu TY (2012) Factors affecting the improvement of quality of dying of terminally ill patients with cancer through palliative care: A ten-year experience. J Palliat Med 15: 854-862.
- Naylor C, Parsonage M, McDaid D, Knapp M, Fossey M, et al. (2012) Long-Term Conditions and Mental Health: The Cost of Co-Morbidities.
- Triberti S, Savioni L, Sebri V, Pravettoni G (2019) eHealth for improving quality of life in breast cancer patients: A systematic review. Cancer Treat Rev 74: 1-14.
- Pérez-Cruz PE, Langer P, Carrasco C, Bonati P, Batic B, et al. (2019) Spiritual Pain Is Associated with Decreased Quality of Life in Advanced Cancer Patients in Palliative Care: An Exploratory Study. J Palliat Med 22: 663-669.
- Okoth K, Chandan JS, Marshall T, Thangaratinam S, Thomas GN, et al. (2020) Association between the reproductive health of young women and cardiovascular disease in later life: Umbrella review. The BMJ 371: m3502.
- Aromataris E, Fernandez R, Godfrey CM, Holly C, Khalil H, et al. (2015) Summarizing systematic reviews: Methodological development, conduct and reporting of an umbrella review approach. Int J Evid Based Healthc 13: 132-140.
- Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A (2016) Rayyan-A web and mobile app for systematic reviews. Systematic Reviews 5: 210.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, et al. (2021) The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Systematic Reviews 10: 89.
- Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, et al. (2017) AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ (Clinical Research Ed.), 358: j4008.
- Flyum IR, Mahic S, Grov EK, Joranger P (2021) Health-related quality of life in patients with colorectal cancer in the palliative phase: A systematic review and meta-analysis. BMC Palliative Care 20: 144.
- Bai M, Lazenby M (2015) A systematic review of associations between spiritual well-being and quality of life at the scale and factor levels in studies among patients with cancer. J Palliat Med 18: 286-298.
- Gayatri D, Efremov L, Kantelhardt EJ, Mikolajczyk R (2021) Quality of life of cancer patients at palliative care units in developing countries: Systematic review of the published literature. Quality of Life Research : An International Journal of Quality of Life Aspects of Treatment Care and Rehabilitation 30: 315-343.
- Catania G, Costantini M, Beccaro M, Bagnasco A, Sasso L, et al. (2013) Does quality of life assessment in palliative care look like a complex screening program? Health and Quality of Life Outcomes 11: 7.
- Chung V, Sun V, Ruel N, Smith TJ, Ferrell BR, et al. (2022) Improving Palliative Care and Quality of Life in Pancreatic Cancer Patients. J Palliat Med 25: 720-727.
- Davis MP, Hui D (2017) Quality of Life in Palliative Care. Expert Review of Quality of Life in Cancer Care 2: 293-302.
- Gaertner J, Siemens W, Meerpohl JJ, Antes G, Meffert C, et al. (2017) Effect of specialist palliative care services on quality of life in adults with advanced incurable illness in hospital, hospice, or community settings: Systematic review and meta-analysis. BMJ 357: j2925.
- Thaniyath T (2019) The Quality of Life of the Patients Under Palliative Care: The Features of Appropriate Assessment Tools and the Impact of Early Integration of Palliative Care.
- Buiting HM, Terpstra W, Dalhuisen F, Gunnink-Boonstra N, Sonke GS, et al. (2013) The Facilitating Role of Chemotherapy in the Palliative Phase of Cancer: Qualitative Interviews with Advanced Cancer Patients. PLoS ONE 8: e77959.
- Fang P, Jagsi R, He W, Lei X, Campbell EG, et al. (2019) Rising and Falling Trends in the Use of Chemotherapy and Targeted Therapy Near the End of Life in Older Patients With Cancer. J Clin Oncol 37: 1721-1731.
- Biswas J, Faruque M, Banik PC, Ahmad N, Mashreky SR (2022) Quality of life of the cancer patients receiving home-based palliative care in Dhaka city of Bangladesh. PLOS ONE 17: e0268578.
- Felce D (1997) Defining and applying the concept of quality of life. J Intellect Disabil Res 41: 126-135.
- Schalock, R. L. (2004) The concept of quality of life: What we know and do not know. Journal of Intellectual Disability Research 48: 203-216.
- Tope DM, Ahles TA, Silberfarb PM (1993) Psycho-Oncology: Psychological Well·Being as One Component of Quality of Life. Psychother Psychosom 60: 129-147.
- Elmqvist MA, Jordhøy MS, Bjordal K, Kaasa S, Jannert M (2009) Health-related quality of life during the last three months of life in patients with advanced cancer. Support Care Cancer 17: 191-198.
- Diamond EL, Russell D, Kryza-Lacombe M, Bowles KH, Applebaum AJ, et al. (2016) Rates and risks for late referral to hospice in patients with primary malignant brain tumors. Neuro Oncol 18: 78-86.
- Cheng SY, Dy S, Hu WY, Chen CY, Chiu TY (2012) Factors affecting the improvement of quality of dying of terminally ill patients with cancer through palliative care: A ten-year experience. J Palliat Med 15: 854-862.
- Naylor C, Parsonage M, McDaid D, Knapp M, Fossey M, et al. (2012) Long-Term Conditions and Mental Health: The Cost of Co-Morbidities.
- Triberti S, Savioni L, Sebri V, Pravettoni G (2019) eHealth for improving quality of life in breast cancer patients: A systematic review. Cancer Treat Rev 74: 1-14.
- Pérez-Cruz PE, Langer P, Carrasco C, Bonati P, Batic B, et al. (2019) Spiritual Pain Is Associated with Decreased Quality of Life in Advanced Cancer Patients in Palliative Care: An Exploratory Study. J Palliat Med 22: 663-669.
- Okoth K, Chandan JS, Marshall T, Thangaratinam S, Thomas GN, et al. (2020) Association between the reproductive health of young women and cardiovascular disease in later life: Umbrella review. The BMJ 371: m3502.
- Aromataris E, Fernandez R, Godfrey CM, Holly C, Khalil H, et al. (2015) Summarizing systematic reviews: Methodological development, conduct and reporting of an umbrella review approach. Int J Evid Based Healthc 13: 132-140.
- Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A (2016) Rayyan-A web and mobile app for systematic reviews. Systematic Reviews 5: 210.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, et al. (2021) The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Systematic Reviews 10: 89.
- Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, et al. (2017) AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ (Clinical Research Ed.), 358: j4008.
- Flyum IR, Mahic S, Grov EK, Joranger P (2021) Health-related quality of life in patients with colorectal cancer in the palliative phase: A systematic review and meta-analysis. BMC Palliative Care 20: 144.
- Bai M, Lazenby M (2015) A systematic review of associations between spiritual well-being and quality of life at the scale and factor levels in studies among patients with cancer. J Palliat Med 18: 286-298.
- Gayatri D, Efremov L, Kantelhardt EJ, Mikolajczyk R (2021) Quality of life of cancer patients at palliative care units in developing countries: Systematic review of the published literature. Quality of Life Research : An International Journal of Quality of Life Aspects of Treatment Care and Rehabilitation 30: 315-343.
- Catania G, Costantini M, Beccaro M, Bagnasco A, Sasso L, et al. (2013) Does quality of life assessment in palliative care look like a complex screening program? Health and Quality of Life Outcomes 11: 7.
- Chung V, Sun V, Ruel N, Smith TJ, Ferrell BR, et al. (2022) Improving Palliative Care and Quality of Life in Pancreatic Cancer Patients. J Palliat Med 25: 720-727.
- Davis MP, Hui D (2017) Quality of Life in Palliative Care. Expert Review of Quality of Life in Cancer Care 2: 293-302.
- Gaertner J, Siemens W, Meerpohl JJ, Antes G, Meffert C, et al. (2017) Effect of specialist palliative care services on quality of life in adults with advanced incurable illness in hospital, hospice, or community settings: Systematic review and meta-analysis. BMJ 357: j2925.
- Leung DYP, Chan HYL (2020) Palliative and End-of-Life Care: More Work is Required. Int J Environ Res Public Health 17: 7429.
- Lucchiari C, Masiero M, Pravettoni GG, Wears R (2010) End-of-life decision-making: A descriptive study on the decisional attitudes of Italian physicians. Life Span and Disability 13: 71-86.
- Pinto SMO, Berenguer SMAC, Martins JCA, Kolcaba K (2016) Cultural adaptation and validation of the Portuguese End of Life Spiritual Comfort Questionnaire in Palliative Care patients. Porto Biomed. J 1: 147-152.
- Puchalski CM, Kilpatrick SD, McCullough ME, Larson DB (2003) A systematic review of spiritual and religious variables in Palliative Medicine, American Journal of Hospice and Palliative Care, Hospice Journal, Journal of Palliative Care, and Journal of Pain and Symptom Management. Palliative & Supportive Care 1: 7-13.
- Visser A, Garssen B, Vingerhoets A (2010) Spirituality and well-being in cancer patients: A review. Psycho-Oncology 19: 565-572.
- Dong M, Wu S, Zhu Y, Jin S, Zhang Y, et al. (2017) Secular examination of spirituality-prosociality association: Survey research in nonreligious-based populations in China. Archiv für Religionspsychologie 39: 61-81.
- Koenig HG (2008) Concerns About Measuring “Spirituality” in Research. Journal of Nervous & Mental Disease 196: 349-355.
- Balducci L (2019) Geriatric Oncology, Spirituality, and Palliative Care. J Pain Symptom Manage 57: 171-175.
- Balboni TA, Paulk ME, Balboni MJ, Phelps AC, Loggers ET, et al. (2010) Provision of spiritual care to patients with advanced cancer: Associations with medical care and quality of life near death. J Clin Oncol 28: 445-452.
- Bovero A, Leombruni P, Miniotti M, Rocca G, Torta R. (2016) Spirituality, quality of life, psychological adjustment in terminal cancer patients in hospice. Eur J Cancer Care 25: 961-969.
- Lloyd-Williams M, Reeve J, Kissane D (2008) Distress in palliative care patients: Developing patient-centred approaches to clinical management. Eur J Cancer (Oxford, England: 1990) 44: 1133-1138.
- McCoubrie RC, Davies AN (2006) Is there a correlation between spirituality and anxiety and depression in patients with advanced cancer? Supportive Care in Cancer: Official Journal of the Multinational Association of Supportive Care in Cancer 14: 379-385.
- Nelson CJ, Rosenfeld B, Breitbart W, Galietta M (2002) Spirituality, religion, and depression in the terminally ill. Psychosomatics 43: 213-220.
- Marton G, Monzani D, Vergani L, Pizzoli SFM, Pravettoni G, et al. (2022) Optimism Is a Strategy for Making a Better Future. European Psychologist 27: 41-61.
- Tao Y, Yu H, Liu S, Wang C, Yan M, et al. (2022) Hope and depression: The mediating role of social support and spiritual coping in advanced cancer patients. BMC Psychiatry 22: 345.
- Fitzgerald P, Lo C, Li M, Gagliese L, Zimmermann C, et al. (2015) The relationship between depression and physical symptom burden in advanced cancer. BMJ Supportive & Palliative Care 5: 381-388.
- Teunissen SCCM, Wesker W, Kruitwagen C, de Haes HCJM, Voest EE, et al. (2007) Symptom prevalence in patients with incurable cancer: A systematic review. J Pain Symptom Manage 34: 94-104.
- Laird BJA, Scott AC, Colvin LA, McKeon AL, Murray GD, et al. (2011) Pain, Depression, and Fatigue as a Symptom Cluster in Advanced Cancer. J Pain Symptom Manage 42: 1-11.
- Seow H, Stevens T, Barbera LC, Burge F, McGrail K, et al. (2021) Trajectory of psychosocial symptoms among home care patients with cancer at end-of-life. Psycho-Oncology 30: 103-110.
- Hart NH, Crawford-Williams F, Crichton M, Yee J, Smith TJ, et al. (2022) Unmet supportive care needs of people with advanced cancer and their caregivers: A systematic scoping review. Crit. Rev. Oncol. Hematol. 176: 103728.
- Emanuel LL, Solomon S, Chochinov HM, Delgado Guay MO, Handzo G, et al. (2023) Death Anxiety and Correlates in Cancer Patients Receiving Palliative Care. J Palliat Med 26: 235-243.
- Benson JJ, Washington KT, Landon OJ, Chakurian DE, Demiris G, et al. (2023) When Family Life Contributes to Cancer Caregiver Burden in Palliative Care. J Fam Nurs 29: 275-287.
- Moens K, Higginson IJ, Harding R, Euro Impact (2014) Are there differences in the prevalence of palliative care-related problems in people living with advanced cancer and eight non-cancer conditions? A systematic review. J Pain Symptom Manage 48: 660-677.
- Kittelson SM, Elie MC, Pennypacker L (2015) Palliative Care Symptom Management. Critical Care Nursing Clinics of North America 27: 315-339.
- Marzorati C, Pravettoni G (2017) Value as the key concept in the health care system: how it has influenced medical practice and clinical decision-making processes. J Multidiscip Healthc 10: 101-106.
- Applebaum AJ, Kent EE, Ellington L, Campbell G, Donovan H, et al. (2024) Top Ten Tips Palliative Care Clinicians Should Know About Caring for Family Caregivers. J Palliat Med 27: 930-938.
- Hoomani Majdabadi F, Ashktorab T, Ilkhani M (2022) Impact of palliative care on quality of life in advanced cancer: A meta-analysis of randomised controlled trials. Eur J Cancer Care (Engl) 31: e13647.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Radbruch L, De Lima L, Knaul F, Wenk R, Ali Z, et al. (2020) Redefining Palliative Care-A New Consensus-Based Definition. J Pain Symptom Manage 60: 754-764.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Sala D, Marzorati C, Voskanyan V, Grasso R, Pietrobon R, Heide I, et al. (2025) Psychosocial Factors Associated with Quality of Life in Palliative Care and End of Life Adult Cancer Patients: An Umbrella Review. J Palliat Care Med 15: 765.
Copyright: © 2025 Sala D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 771
- [From(publication date): 0-0 - Dec 09, 2025]
- Breakdown by view type
- HTML page views: 667
- PDF downloads: 104